International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2023)Volume 11, Issue 2
Title: Early detection of chronic kidney disease in a diabetic population. A massive screening program in primary healthcare in a middle-income country.
Background: Early detection of Chronic Kidney Disease (CKD) allows health professionals and patients to take actions to slow physical impairment and prevent or delay dialysis or transplantation and their catastrophic costs. In this study, we aimed to describe a CKD massive screening program in patients with diabetes to explore the feasibility of massive detection of CKD in high risk patients.
Methods and findings: We performed a descriptive, cross-sectional study with people living with diabetes, at the primary healthcare units of the ministry of health in Jalisco, Mexico. They underwent a screening including a health history questionnaire, somatometry, urinary albumin, serum creatinine, and estimated Glomerular Filtration Rate (eGFR) in accordance with the Kidney Early Evaluation Program (KEEP). We described demographic and clinical characteristics of the population by sex and calculated the prevalence of each CKD stage.
Of 7,693 recruited patients, 44% were identified with CKD; 35% were in early stages (1 or 2), and 9% in stages 3 to 5. Less than 1% of total patients had previous CKD diagnosis. Among other clinical characteristics, we found that 83% of all patients were overweight or obese and 79% had blood pressure values over 130/80 mmHg.
Conclusion: This study shows the technical feasibility and usefulness of massive CKD screening campaigns in high risk people at primary healthcare services. Patients with renal function impairment, who require treatment for preventing disease progression, were identified. It is essential to formulate public policies aimed at protocolization of timely medical interventions to address the incidence and prevalence of CKD.
Diabetes mellitus; Chronic kidney disease; Mass screening; Early diagnosis; Keep
ACR: Albumin Creatinine Ratio; BMI: Body Mass Index; CKD: Chronic Kidney Disease; DM-2: Type 2 Diabetes Mellitus; eGFR: Estimated Glomerular Filtration Rate; ESRD: End-Stage Renal Disease; INEGI: National Institute of Statistics and Geography; KEEP: Kidney Early Evaluation Program; RRR: Remaining Renal Reserve; SESAJ: Jalisco State Health Services.
The prevalence of type 2 Diabetes Mellitus (DM-2) and its complications has increased steadily around the world, mainly in medium and low income countries. In 2019, they caused approximately 71.84 deaths per 100,000 inhabitants (95% UIC 58.4-87.2) [1]. Mexico is among the countries with the higher diabetes prevalence. According to the national health and nutrition survey, in 2020, 10.6% of the population aged 20 years or older had a diabetes diagnosis. Moreover, the diabetes prevalence increased 6.5% in the previous 8 years [2]. The National Institute of Statistics and Geography (INEGI) ranked diabetes as the third leading cause of death, with 13.9% of deaths in 2020 [3].
Nephropathy is a frequent complication of people living with diabetes and is one of its main causes of mortality. Inadequate control of DM-2 causes renal damage and leads to Chronic Kidney Disease (CKD), defined as a Glomerular Filtration Rate (eGFR) less than 60 ml/min per 1.73 square meters, or evident renal damage, persisting for 3 months or more [4]. At its most advanced stage, CKD is known as End Stage Renal Disease (ESRD), and involves catastrophic expenses associated with the need for therapies to survive, such as different forms of dialysis or renal transplantation [5].
CKD manifests symptoms only in advanced stages of the disease. Therefore, it is usually identified late when there is no possibility of reversing it. Thus, as renal damage progresses, the remaining renal reserve is insufficient and the only option for preserving life is replacement therapy. This impact can be reduced if CKD is identified and managed efficiently from its early stages. This opportunity is a shared responsibility: a) For the patient living with DM-2; b) For the primary health care personnel in direct contact with the patient; and c) For the National Health System responsible for the required supplies [6].
Among the main causes that hinder timely detection of CKD in patients living with DM-2 are the following: 1) Lack of a protocolized model for CKD care in primary healthcare services. 2) Poor training of primary healthcare professionals to identify risk factors and to act accordingly. 3) Limited actions and resources for early detection in high risk patients. 4) Lack of a public policy that integrates early detection and timely management of CKD with performance metrics to monitor deviations and progress [6]. These problems are particularly evident in public services that serve most of the population.
One strategy for timely detection of kidney damage is the international screening protocol known as Kidney Early Evaluation Program (KEEP) [7]. This protocol aims to detect early stages of CKD among high risk individuals and allows screening in large vulnerable population groups. KEEP was developed by the international kidney foundation and adapted to the Mexican population by the Mexican Kidney Foundation [8,9]. According to this program, proteinuria defines the risk of accelerated impairment of the Remaining Renal Reserve (RRR).
In this paper, we present the implementation and results of a CKD screening exercise in Mexico following the KEEP, aiming to explore the feasibility of massive detection of the disease in high risk patients. We ran the program in DM-2 patients with or without arterial hypertension, who were affiliated to public healthcare services in Jalisco, Mexico, during September 2011 and March 2012. The information obtained contributes with evidence for the design and implementation of public policies towards the construction of an early and protocolized CKD care model at the national level and potentially useful for other middle income countries.
Study design and participants
We carried out a descriptive, cross-sectional study with a population previously diagnosed with DM-2 in the metropolitan area of Guadalajara, Jalisco, Mexico. We called for all people with DM-2 diagnosis who were registered in the Jalisco state health services (SESAJ, acronym in Spanish), to attend public squares on specific dates and times to undergo on-site screening. As inclusion criteria we asked people to be affiliated to the SESAJ, to be 18 years or older, to have a previous DM-2 diagnosis, and to agree to participate in the study. We excluded individuals who were beneficiaries of a social security institution, those receiving treatment for ESRD, or with history of renal transplantation.
Procedures
We performed detection and characterization of CKD according to the KEEP methodology [7], whose rights of use in Mexico belong to the Mexican kidney foundation, the institution that coordinates and supervises the screening. We chose this methodology because it offers on-site results, it allows us to estimate the RRR, and because by determining the presence of albuminuria, it provides a risk criterion for the rapid deterioration of this reserve.
Prior to screening, we made some arrangements with state authorities including the planning of the program operations, the definition of the public areas for the application of the tests, the selection of the personnel who would participate in the brigades coordinated by the SESAJ and the designation of their leader. A total of 80 health professionals performed the screening. They were divided into four groups or brigades and distributed around Guadalajara city and its metropolitan area.
At the same time, we developed an excel mask for data collection paying special attention to the construction of restrictions in the registration fields. All fields were set as mandatory to avoid recording cases with missing data.
All 80 health professionals involved received a six-hour training in early detection of CKD and screening methodology including weight, height, and blood pressure measurement, and on-site measurement of standardized serum creatinine and urinary albumin and creatinine.
As we did not have the possibility to communicate directly with patients, all those attending for consultation in their health units during the two months prior to the established screening date were invited to participate. In addition, the invitation was disseminated through a vehicle mounted loudspeaker in areas close to the health units. Convening patients with diabetes to attend the screening was the task of each health jurisdiction. Patients living in remote areas were transported by SESAJ personnel to the place and day designated for the screening.
Screening for CKD was performed in the last week of August 2011 and in March 2012 by the previously trained brigades. The procedures were organized in six screening modules, as described in Figure 1. A detailed description of the KEEP is available elsewhere [7,10,11].
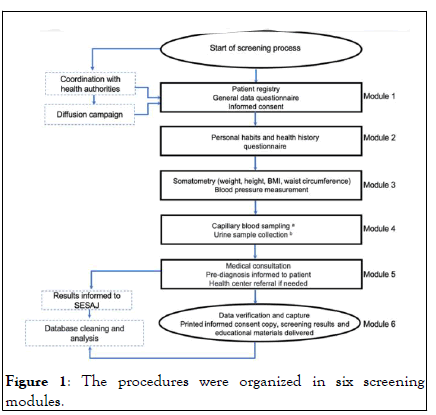
Figure 1: The procedures were organized in six screening modules.
We used standardized serum creatinine for eGFR estimation using the modification of diet in renal disease study formula that defines RRR [12]. Urinary albumin and creatinine were expressed as albumin/creatinine index which is used to estimate the rate of RRR deterioration [13]. We defined CKD stages according to the KDIGO 2020 clinical practice guideline for diabetes management in CKD patients [4]. Stage 1, eGFR of 90 mL/min/1.73 m2 or greater and Albumin Creatinine Ratio (ACR) of 30 mg/g or greater; stage 2, eGFR of 60 to 89 mL/min/1.73 m2 and ACR of 30 mg/g or greater; stage 3, eGFR of 30 to 59 mL/min/1.73 m2; stage 4, eGFR of 15 to 29 mL/min/1.73 m2; and stage 5, eGFR less than 15 mL/min/ 1.73 m2.
For quality monitoring of the program, we performed validation of the on-site digital puncture tests in 200 patients, with venipuncture tests, which required pre-analytical handling, sending to a reference laboratory for processing and reporting.
Data analysis
We described participant demographic and clinical characteristics using frequencies and percentages or central tendency and dispersion measures as appropriate. In accordance with the criteria mentioned in the methods section, we used the ACR and eGFR to classify patients into those with CKD and those without CKD. Patients with CKD were in turn classified according to their stage of disease. Frequencies and percentages of patients in each stage were calculated for total population and by sex.
Ethical considerations
The data collection and analysis project were approved by the research ethics committee of the school of medicine of the Pan American university, and the research ethics committee of the national institute of public health. Study was performed in accordance with the ethical standards of the 1964 declaration of Helsinki and its amendments.
All patients signed an informed consent form and received a printed copy with their screening results, as well as educational materials on CKD. Screening results were appropriately anonymized before analysis.
The screening was carried out in two periods, each lasting 2 weeks. The first period was carried out in August 2011 and was attended by 5,183 participants from health regions X, XI, XII, and XIII of the SESAJ. Given the high population with DM-2, a second screening was scheduled for March 2012, for health regions III, IV, and IX. A total of 7,693 patients attended the screening.
Being a member of a social security institution was initially considered an exclusion criterion. However, 34 patients (0.4%) from the Mexican social security institute requested the screening, and it was not denied. The remaining 99.6% of the patients were the responsibility of the SESAJ and reported having access to them.
From 7,693 total patients, 5,544 (72.1%) were women. The average age was 58 ± 12.1 (59.8 ± 12.5 for men and 57.85 ± 12.10 for women) with a range of 18 to 97 years old. The average age at the time of diabetes diagnosis was 51.1 years old (SD=13.1) for men and 49.1 (SD=12) for women.
With the health history questionnaire and somatometry, we obtained the clinical data shown in Table 1. Eighty-three percent of the patients were overweight or obese, with a mean Body Mass Index (BMI) of 28.8 (SD=4.8) for men and 30.7 (SD=5.7) for women. Fifty-five percent of the patients, besides living with diabetes, had a previous hypertension diagnosis. Among men, 30% were aware of having hypercholesterolemia, 37% reported neuropathy symptoms and 47.9% had a previous diagnosis of hypertension. Meanwhile, 41.2% of women were aware of hypercholesterolemia, 43% had neuropathy symptoms and 58% had hypertension diagnosis. Among patients with known hypertension diagnosis, only 21% had adequate blood pressure control (<130/80 mm/Hg), whereas 58% of patients without hypertension history had high blood pressure levels (>130/80 mm/Hg). The average time since DM-2 diagnosis was eight years.
| Clinical characteristics | Men n=2,14927.9% | Women n=5,544 (72.1%) |
|---|---|---|
| Continuous variables | X(s) | X(s) |
| Body weight (kg) | 78.6 (15.1) | 71 (14.4) |
| Height (cm) | 164.8 (7.1) | 152 (6.6) |
| Waist circumference (cm) | 101.8 (11.8) | 100.3 (12.2) |
| BMI (kg/cm2) | 28.8 (4.8) | 30.65 (5.7) |
| Systolic blood pressure (mm/Hg) | 150.7 (19.6) | 149.56 (18.2) |
| Diastolic blood pressure (mm/Hg) | 89.5 (12.1) | 87.40 (11.5) |
| Dichotomous variables | N (%) | N (%) |
| Positive smoking (≥ 100 cigarettes) | 1,386 (64.5) | 1,410 (25.4) |
| Previous hypertension diagnosis | 1,029 (47.9) | 3,213 (58) |
| Previous hypercholesterolemia diagnosis | 651 (30.3) | 2,284 (41.2) |
| Previous CKD diagnosis | 1 (0.05) | 4 (0.1) |
| Heart attack history | 72 (3.4) | 139 (2.5) |
| Coronary bypass history | 19 (0.8) | 33 (0.6) |
| Stroke history | 26 (1.2) | 56 (1) |
| Previous heart failure diagnosis | 62 (2.9) | 177 (3.2) |
| Previous arteriosclerosis diagnosis | 46 (2.1) | 138 (2.5) |
| Previous anemia diagnosis | 88 (4.1) | 713 (12.9) |
| Previous retinopathy diagnosis | 228 (10.6) | 637 (11.5) |
| Previous glaucoma diagnosis | 73 (3.4) | 222 (4) |
| Neuropathy symptoms (numbness, tingling or pain) | 797 (37.1) | 2,389 (43.1) |
| Limb amputation history | 73 (3.4) | 53 (0.96) |
| Family history of diabetes | 1,464 (68.1) | 3,907 (70.5) |
Table 1: Clinical characteristics of DM-2 population attending an early mass detection program in Jalisco, Mexico, n=7,693.
Regarding renal function, we found that 40% of the screened patients had albuminuria, which is an indicator of risk of accelerated RRR deterioration; 34% microalbuminuria (30 mg/ g-300 mg/g) and 6% albuminuria (>300 mg/g).
Among all 7,693 patients, 3,393 (44.1%) had glomerular damage as a CKD diagnosis criterion; 2,714 (35%) were in early stages of the disease, i.e., stages one or two, 596 (7.7%) in stage three, 62 (0.8%) in stage four, and 21 (0.3%) in stage five (Table 2).
| CKD stage | Total n=7,693 | Men n=2,149 | Women n=5,544 | |
|---|---|---|---|---|
| Normal renal function | 4,300 (55.9%) | 1,157 (53.8%) | 3,143 (56.7%) | |
| CKD | Stage 1 | 1,701 (22.1%) | 458 (21.3%) | 1,243 (22.4%) |
| Stage 2 | 1,013 (13.2%) | 324 (15.1%) | 689 (12.4%) | |
| Stage 3 | 596 (7.7%) | 175 (8.1%) | 421 (7.6%) | |
| Stage 4 | 62 (0.8%) | 25 (1.2%) | 37 (0.7%) | |
| Stage 5 | 21 (0.3%) | 10 (0.5%) | 11 (0.2%) | |
| Total | 3,393 (44.1%) | 992 (46.2%) | 2,401 (43.3%) |
Table 2: CKD stage in diabetic population according with an early mass detection program in Jalisco, Mexico, n=7,693.
Table 3 shows the number of patients identified in each CKD stage as a proportion of the total patients diagnosed through the on-site quick tests performed in the CKD detection program. Eighty percent of the 3,393 patients diagnosed were in early stages of CKD, namely stages one or two, whereas 1.8% had severely decreased renal function (stage four) and 0.6% were in end stage renal disease (stage five). These two advanced stages total 63 patients. By comparison, while answering the health history questionnaire, only five individuals were aware they had CKD.
| CKD stage | n (%) |
|---|---|
| Stage 1 | 1,701 (50.1) |
| Stage 2 | 1,013 (29.9) |
| Stage 3 | 596 (17.6) |
| Stage 4 | 62 (1.8) |
| Stage 5 | 21 (0.6) |
Table 3: Proportion of patients diagnosed with CKD by disease stage, n=3,393.
This screening exercise demonstrates that it is possible for primary care health services to carry out massive CKD detection campaigns in patients at risk in short periods. State coordination and training for health personnel who participated in the brigades were adequate for early detection of kidney damage in patients with DM-2. This mass screening initiative was successful in terms of the number of patients served. Point of care quick tests turned out to be very efficient. They allowed the screening of a large volume of patients who otherwise might have delayed or avoided diagnosis if it involved attendance to a fixed laboratory with a difficult schedule and possibly at a great distance from home. Point of care technology grants the required tests to be made at the site of the event, with easier sampling. There is no need for vein puncture. Moreover, after a patient's presence at the sampling site, centrifugation, and determination of analyses in a lab are not necessary. As a result, we were able to test 200 individuals per day and still give them their results on the spot.
Although the number of patients screened was satisfactory, we recognize that it could have been even higher, c onsidering the large number of DM-2 patients registered in the SESAJ. A longer, more tailored effort to engage at risk population would likely attract a larger population. On the other hand, the screenings were done during typical working hours, which could explain, at least in part, the higher proportion of women who attended, given the higher rates of employment in men in Mexico. Additionally, men tend to delay seeking medical care more than women [14]. For future programs, more inclusive planning that considers labor and gender differences should be considered.
The results of this mass screening made it easier for the SESAJ to provide patients with DM-2, now identified as having CKD, with timely and protocolized management of this complication in their corresponding health centers. This represented the opportunity to efficiently manage 3,310 patients diagnosed with stages 1, 2 and 3 of CKD to delay further RRR impairment. The 83 individuals detected in stages 4 and 5 received information about their management options and were channeled to the authorities to be referred to specialized care centers.
The high prevalence of CKD we found in this diabetic population (44%) highlights the need for periodic actions for the early detection of this disease among the population at high risk at the primary health services at a national level. A pilot implementation of the KEEP in Mexico in 2008 showed a CKD prevalence of 22% in Mexico city and 33% in Jalisco [15]. Nevertheless, unlike the program we report here, in that pilot study a wider range of at risk patients such as those with a family history of diabetes and hypertension were included. It is not surprising that the prevalence we found among people already living with diabetes is higher. In 2018, the national prevalence of CKD in the general population was 6.3% and 6.5% for the state of Jalisco. As in our results, the national prevalence in 2018 was slightly higher for men than from women (6.4 and 6.1% respectively) [16]. Another striking aspect is that most of the patients in whom CKD was identified were unaware that they had the disease. This situation had already been identified in other studies. For instance, Whaley-Connell et al. found that less than 10% of patients diagnosed with CKD after screening with the KEEP knew they had the disease [17].
CKD care requires a national public policy that defines the technical competencies of health professionals and the tools required for timely detection and treatment. An ideal protocolized care model should consider a) Trained personnel; b) Hardware and software to capture data and calculate indicators to define short, medium and long-term outcomes; c) Access to a clinical laboratory in the primary health care units or close to them; d) Complete supply of authorized drugs; e) A multidisciplinary team integrating medical, psychological, nutritional, and nursing services; and f) An educational program aimed at informing patients and raising awareness about the best way to live with their disease, including the adoption of healthy habits and behaviors and adherence to treatment.
Among the clinic characteristics of the patients screened, demands attention the fact that more than 80% of patients were overweight or obese and their large waist circumference measurements are correlated with central fat accumulation, metabolic syndrome, and systemic inflammation. A relationship between visceral adiposity, insulin resistance, and microal buminuria has been previously established. These facts come hand in hand with the high blood pressure levels, hypercholesterolemia, and neuropathy symptoms we found. It is worth noting that, despite living with DM-2 for near a decade, few patients live with significant cardiovascular alterations. This allows us to anticipate that they will survive long enough so that, if they do not take actions, they may reach advanced stages of CKD, the so-called ESRD that requires dialysis and/or transplantation and their catastrophic consequences in order to survive. More than half of patients who did not know they had hypertension and almost 80% of those with previous diagnosis had blood pressure levels over 130/80 mm/Hg. The high proportion of patients with elevated blood pressure, regardless of whether they had a previous hypertension diagnosis, underscores the importance of making health care personnel aware of the need to take complete vital signs at each visit and to inform the patient about them.
A limitation for the generalization of our results is that, since we did not have the means to contact patients personally, they were called by means of public calls. The individuals included in the screening were self-selected. It is possible that those who chose to participate had a particular health concern. On the other hand, only registered individuals and therefore residents of the State of Jalisco were called, and it is known that there are some differences in socioeconomic and health conditions among people from different regions of Mexico.
We acknowledge that resource allocation and consumables supply needed to guarantee successful mass detection campaigns and timely treatment of diagnosed patients poses important challenges for Mexico and other low and middle income countries. However, after this mass screening initiative, we concluded that sanitary jurisdictions in Mexico have an infrastructure that allows the organization of brigades for the early detection of albuminuria and CKD. The early detection and sensitization of those DM-2 patients at risk of an accelerated RRR deterioration is technically feasible.
We gratefully acknowledge the administrative and financial support from the general directorate of public health of the Jalisco state health services and the Mexican federal government through the national health protection commission.
This project was initially funded by the general directorate of public health of the Jalisco state health services and the Mexican federal government through the national health protection commission.
Partial financial support for paper publication was received from a public funding grant from the national council of science and technology (Grant number I1200/062/2022). Funding source had any role in the study design, data collection, analysis, or interpretation processes, nor in the decision to submit the article for publication.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
The authors have no financial or non-financial competing interests to declare that are relevant to the content of this article.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Miguela MA, Lastiri-Quirosb HS, Obradorc GT, Palacio-Mejiad LS, Hernandez-Avilae JE, Amezcuaf MM, et al. (2023) Early Detection of Chronic Kidney Disease in a Diabetic Population. A Massive Screening Program in Primary Healthcare in a Middle-Income Country. Int J Phys Med Rehabil. 11:661.
Received: 08-Nov-2022, Manuscript No. JPMR-22-20409; Editor assigned: 10-Nov-2022, Pre QC No. JPMR-22-20409 (PQ); Reviewed: 24-Nov-2022, QC No. JPMR-22-20409; Revised: 23-Jan-2023, Manuscript No. JPMR-22-20409 (R); Published: 30-Jan-2023 , DOI: 10.35248/2329-9096.23.11.661
Copyright: © 2023 Miguela M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.