Translational Medicine
Open Access
ISSN: 2161-1025
ISSN: 2161-1025
Case Report - (2023)Volume 13, Issue 4
This paper illustrates a rare case of recurrent spontaneous coronary artery dissection (type 2a according to Yip-Saw) occurred in a 35-year-old non-pregnant woman. The invasive assessment revealed a long dissection of the mid Left Anterior Descending Artery (LAD), which could be confirmed by intravascular ultrasound and was treated successfully with two drug eluting stents. Thirty hours later, the patient developed a second event with severe symptoms and new Electrocardiogram (ECG) ischemic changes. The second angiography showed a new spontaneous dissection of the mid Circumflex Artery (CX), which was treated with one drug-eluting stent. The patient was transferred back to the intermediate care unit and was discharged on the dual antiplatelet therapy on the fifth day. The left ventricular ejection fraction was normal. The heart enzymes increased slightly and normalized within four days. The vessel screening showed no abnormalities in the extra coronary arteries. In patients with spontaneous coronary dissection, intracoronary imagining is helpful in choosing the optimal treatment strategy and should be used whenever available. The possibility of early recurrence makes it mandatory to transfer all patients for a prolonged monitoring after a coronary intervention.
Spontaneous coronary dissection; Coronary intervention; Intravascular Ultrasound (IVUS); Case report
Spontaneous coronary artery dissection is a rare presentation of acute coronary syndrome, occurring predominantly in young non-pregnant females. Contrary to atherosclerotic ischemic heart disease, a spontaneous tear in the tunica media, often without plaque formation, leads to myocardial infarction. Up to 10% of patients experience a dissection recurrence. Even though the proper management has not been established so far, the overall prognosis may be good.
A female non-smoker patient, aged 34, sought our emergency department at 6 am due to ongoing retrosternal discomfort. The lady’s night was interrupted at midnight by a sudden severe retrosternal pain which lasted about 40 minutes and got better spontaneously. After a while, the moderate pain re-occurred and lasted until the presentation in out institution. There was no significant medical history and the patient did not take any medications. She was a mother of a 4-year-old son and denied pregnancy. There were no cardiovascular risk factors.
On physical examination no significant abnormalities were found, especially the lung auscultation revealed regular respiratory sounds over the whole area of both lungs. The 12- lead-ECG (Figure 1) demonstrated regular sinus rhythm with no tachycardia but with significant myocardial ischemia (ST elevations in I, AVL, V4, V5, deep inverse T-waves in V2-V5). The bed-side echocardiography ruled out pericardial effusion, but demonstrated a slightly abnormal left ventricular Ejection Fraction (EF 50%) with hypo kinesis of the anterior wall. The patient was referred to the cath lab for emergent invasive angiography due to assumed subacute anterior myocardial infarction.
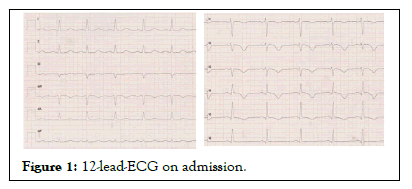
Figure 1: 12-lead-ECG on admission.
On the diagnostic coronary angiogram (Figure 2), a culprit lesion was identified in segment 7 of the LAD: Rather long, with Thrombolysis In Myocardial Infarction (TIMI) 2 flow and with regular vessel diameter of segment 8. Because of ongoing symptoms and ECGs signs, further intracoronary assessment was needed.
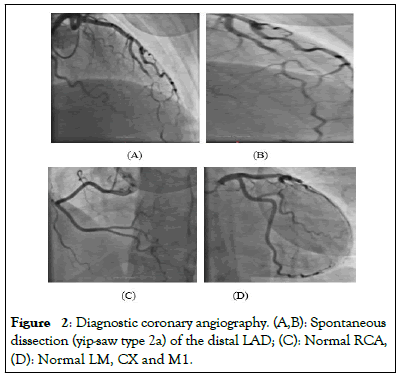
Figure 2: Diagnostic coronary angiography. (A,B): Spontaneous dissection (yip-saw type 2a) of the distal LAD; (C): Normal RCA, (D): Normal LM, CX and M1.
IVUS showed a long coronary dissection with the pathognomic ‘white-black-white’ (between 12 and 3 o’clock), which is pathognomonic for SCAD sign (Figure 3).
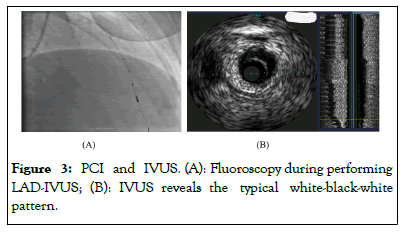
Figure 3: PCI and IVUS. (A): Fluoroscopy during performing LAD-IVUS; (B): IVUS reveals the typical white-black-white pattern.
The decision was made to seal the dissection and so two Drug- Eluting Stents (DES) were implanted (Everolimus; Xience Pro 2.5 × 28 mm and 2.25 × 28 mm). The angiographic and IVUSresults were very good (Figure 4). The patient was transfer to the intermediate care unit and remained completely asymptomatic for 30 hours.
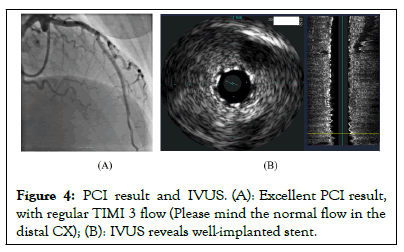
Figure 4: PCI result and IVUS. (A): Excellent PCI result, with regular TIMI 3 flow (Please mind the normal flow in the distal CX); (B): IVUS reveals well-implanted stent.
After 30 hours, the lady complained of a new severe retrosternal pain. The 15-lead-ECG showed acute myocardial ischemia of the lateral wall (Figure 5) and the patient was transferred in the cath lab again. The second coronary angiography showed an excellent result after LAD-Percutaneous Coronary Intervention (LADPCI) and a new flow-limiting dissection of the middle portion of the previously regular CX (Figure 6). This was successfully treated with another DES (Xience Pro, 2.5 × 33 mm; Figure 7).
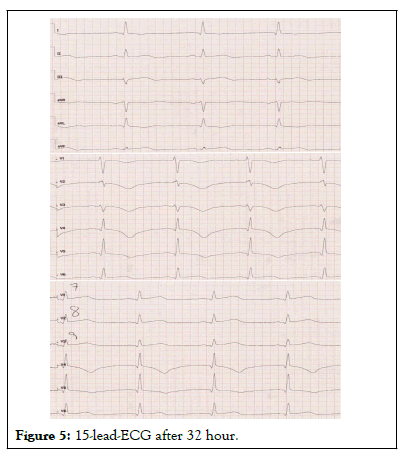
Figure 5: 15-lead-ECG after 32 hour.
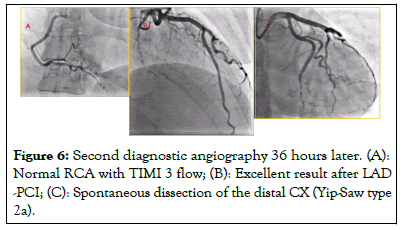
Figure 6: Second diagnostic angiography 36 hours later. (A): Normal RCA with TIMI 3 flow; (B): Excellent result after LAD -PCI; (C): Spontaneous dissection of the distal CX (Yip-Saw type 2a).

Figure 7: PCI and final result. (A): Restoring the TIMI 3 flow by distal wiring (Yip-Saw type 2a); (B): Final PCI result.
Post-PCI the patient stayed three nights in the intermediate care unit and was discharged on the fifth day on the dual antiplatelet therapy (for 12 months). The final echocardiography demonstrated a normal ejection fraction with no relevant abnormalities. The lab analysis showed a slight increase in cardiac enzymes (CK up to 650 U/l, high sensitive troponin I up to 2.5 ng/ml), which normalized within the four days. The ECG on discharge (after five days) showed no acute ischemia (Figure 8). The vessel screening ‘brain-to-pelvis’ with Magnetic Resonance Imaging (MRI) showed no abnormalities in the extra coronary arteries. The patient remained asymptomatic. Although an extensive diagnostic work-up was performed, no relevant abnormalities were found. The extra coronary arteries were regular, no risk factors for atherosclerosis were found and no suspected autoimmune disease was diagnosed. The avoidance of isometric exercises and pre-conception counseling were advised.
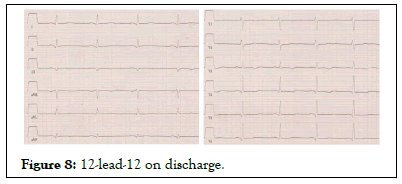
Figure 8: 12-lead-12 on discharge.
Spontaneous Coronary Artery Dissection (SCAD) is defined as a non-traumatic tear in the tunica media of the coronary vessel, with subsequent formation of a true and false lumen [1]. This condition occurs in up to 4% in the general population and is responsible for up to 10% of acute coronary syndromes [1,2]. SCAD has strong gender predominance: over 90% of cases are non-pregnant young women. The 30-day mortality is as low as 1.2% and the prognosis seems to be benign [3].
There are some unanswered issues regarding the development and management of SCAD. The pathophysiology of the disease has not been fully understood. Does the primary event such as spontaneous bleed occur outside or inside the coronary wall? Is there enough evidence to state that this is caused by a rupture of vasa vasorum? If young non-pregnant females are the main disease target, is there any association with female sex hormones and if you to what extent? As the observational studies demonstrated that most cases heal overtime and have a good mid-term prognosis, the interventional treatment should not be performed on a routine basis [4]. The use of intracoronary imaging, preferably Optical Coherence Tomography (OCT), can confirm the suspected diagnosis in most patients. In the current paper however, due to unavailability of OCT, IVUS was used and revealed the typical dissection white-black-white pattern [5].
The proper management has not been established so far and there are no general recommendations due to missing large high-quality data. The conservative approach has been demonstrated to be a safe and effective option due to high rates of spontaneous healing. Yet, the question when and how to perform a PCI, has not been fully answered. Possible strategies are plain old balloon angioplasty, direct stenting, limited wiring or cutting balloons. Most experienced cardiologist would apparently go for PCI with stenting in case of occlusive dissections. In non-occlusive cases, a decision has to be taken individually. In the current type 2a dissection, an operator decided for a PCI with stenting due to persistent symptoms and ECG changes. Two DES were directly implanted. The primary result was excellent.
The recurrence rate of SCAD is up to 10% within first five years [6]. This case is unique because of the early recurrence, just 30 hours after the index event and during the monitoring at the intermediate care unit. Of note, the previously regular CX experienced a type 2a dissection and was treated with one DES. The immediate result was excellent.
In case of a young female with normal life expectancy and potential family planning, a few important issues need to be stressed. Performing a PCI may bring not only benefits but also potential harm: the peri-interventional complication rate is usually higher than in the general population. If treated invasively, co-axial technique and avoidance of aggressive catheter shapes and maneuvers are highly recommended. The primary revascularization goal is to restore the normal coronary flow. Less means more.
In patients with spontaneous coronary dissection, intracoronary imagining is helpful in choosing the optimal treatment strategy and should be used whenever available. The possibility of early recurrence makes it mandatory to transfer all patients for a prolonged monitoring after a coronary intervention.
To conduct this study, the author did not receive any special funding.
The authors declare that they have no competing interests.
On special request, all the collected data can be available.
Marek M. Rogowski: Main conception of the paper, wrote the paper, performed the literature search.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Rogowski MM (2023) Early Recurrent Spontaneous Coronary Artery Dissection: A Case-Report. Trans Med. 13:307.
Received: 10-Nov-2023, Manuscript No. TMCR-23-27974; Editor assigned: 14-Nov-2023, Pre QC No. TMCR-23-27974 (PQ); Reviewed: 28-Nov-2023, QC No. TMCR-23-27974; Revised: 05-Dec-2023, Manuscript No. TMCR-23-27974 (R); Published: 12-Dec-2023 , DOI: 10.35248/2161-1025.23.13.307
Copyright: © 2023 Rogowski MM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.