International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)Volume 9, Issue 5
Background: Interventions related to eye movement, such as optokinetic stimulus or tracking training are beneficial for patients with unilateral spatial neglect. This study aimed to investigate the influence of fixation feedback using visual and verbal cues on the neuropsychological status and self-awareness of patients with unilateral spatial neglect during searching tasks recorded with eye mark recorders.
Methods and findings: This study included 20 inpatients with right hemisphere damage who presented with left unilateral spatial neglect. The patients were randomly divided into two groups for a comparative crossover study. Each intervention period comprised of occupation therapy with or without fixation feedback, which lasted for 5 days. Between interventions, a washout period was allotted for 2 days, which eliminated the effects of the intervention period. A significant difference was observed in the treatment effect of the Behavioral Inattention Test (p=0.04) and the Catherine Bergego Scale score (p=0.01); however, no significant difference was observed in the carry-over and period effects. The limitations include that the crossover comparative studies are considered unsuitable for patients in an acute stage of disease where spontaneous recovery may occur, as in the sample used in this study. Additionally, the number of participants was limited to 20 with no assigned control group.
Conclusion: Fixation feedback using an eye mark recorder improved unilateral spatial neglect and self-awareness. Fixation feedback is an effective top-down approach to unilateral spatial neglect, which demonstrated more significant results compared to normal occupational therapy interventions. Future studies should focus on the intervention effects according to the site of damage.
Unilateral spatial neglect; Fixation; Feedback
BIT: Behavioral Inattention Test; BTT: Baking Tray Test; CBS: Catherine Bergego Scale; GCS: Glasgow Coma Scale; MMSE: Mini Mental Status Examination; OT: Occupational Therapy
Previous studies of patients with unilateral spatial neglect found that rehabilitation causes considerably low functional recovery with long hospitalization stays [1-4]. Additionally, unilateral spatial neglect has a significant influence on the effectiveness of rehabilitation; therefore, it is important to establish effective intervention methods. Previous researches have shown that interventions related to eye movement, such as optokinetic stimulus or tracking training are beneficial for unilateral spatial neglect [5-10]. Similar studies regarding feedback intervention through a variety of means, such as speech or video, have found consistent results [11-16]. Generally, it is common in patients with severe unilateral spatial neglect not to look at the left-side space and for their fixation to gradually drift to the right-side space [1,17-21]. Thus, one factor attributed to unilateral spatial neglect is the difficulty in performing searching eye movements. Many reasons have been posited to explain why patients with unilateral spatial neglect do not look at their neglected side; among which, previous studies have proposed that these patients were unaware of their lack of perception [22,23].
To look at their neglected side, Lawson states that patients with unilateral spatial neglect must be informed regarding their disorder and made aware of where they should direct their efforts [24]. Only encouraging patients to look at their neglected side may not produce sufficient functional improvement.
Furthermore, patients who lack self-awareness regarding their unilateral spatial neglect are thought to have low motivation because they lack understanding regarding the reason for their training [25,26].
Thus, acquiring self-awareness regarding unilateral spatial neglect may be one method for increasing the effectiveness of rehabilitation. Studies on eye movement in unilateral spatial neglect using eye mark recorders can be traced back to the 1980s [27]; additionally, recent technological advancements have caused publications of detailed results [21,28,29].
However, evaluative analysis has been the aim of most research on eye mark recorders; studies regarding the application of these data in treatment remain lacking. To address this, we devised an intervention method for unilateral spatial neglect that feeds back information on fixation while searching for tasks recorded using an eye mark recorder.
We believe that the feedback of fixation information provides patients with information regarding deviations and deficiencies in their searching eye movements. Furthermore, we expect selfawareness to improve through simultaneously providing verbal feedback to encourage patients’ understanding of the fixation information.This study aimed to investigate the effect of fixation feedback using visual and verbal cues on the neuropsychological status and self-awareness of patients with unilateral spatial neglect during searching tasks recorded with eye mark recorders.
This study included 20 inpatients at the Kansai Medical University Hospital (12 male, 8 female; average age, 68.4 ± 9.9 years) who presented with left unilateral spatial neglect, with right hemisphere damage, and no history of cerebrovascular disease. The patient diagnoses were as follows: middle cerebral artery infarction (n=10), posterior cerebral artery infarction (n=1), thalamus hemorrhage (n=5), parietal lobe hemorrhage (n=3), and putamen hemorrhage (n=1). The Behavioral Inattention Test (BIT) was performed within 1 week of onset, wherein all patients received below-cut-off scores in one or more subtests. Detailed information of the participants is provided in Table 1.
| Group | ID | Sex | Age | Lesion location | GCS | MMSE | BIT |
|---|---|---|---|---|---|---|---|
| A | P1 | M | 67 | R. MCA | 14 | 13 | 13 |
| P2 | M | 58 | R. Parietal | 14 | 30 | 89 | |
| P3 | F | 80 | R. Temporo-parietal | 14 | 21 | 55 | |
| P4 | F | 78 | R MCA | 13 | 16 | 87 | |
| P5 | F | 74 | R. MCA | 14 | 19 | 14 | |
| P6 | M | 63 | R. MCA | 15 | 22 | 130 | |
| P7 | F | 62 | R. Thalamus | 14 | 20 | 83 | |
| P8 | F | 58 | R. Putamen | 13 | 18 | 20 | |
| P9 | M | 64 | R. Thalamus | 13 | 11 | 21 | |
| P10 | M | 70 | R. Thalamus | 13 | 12 | 34 | |
| Mean (SE) | 67.4 (7.8) | 13.7 (0.6) | 18.2 (5.6) | 54.6 (40.6) | |||
| B | P11 | M | 81 | R. Temporo-occipital | 14 | 25 | 68 |
| P12 | F | 60 | R Parietal | 15 | 23 | 134 | |
| P13 | M | 78 | R. MCA | 13 | 14 | 67 | |
| P14 | M | 59 | R. MCA | 14 | 26 | 124 | |
| P15 | F | 50 | R MCA | 14 | 16 | 16 | |
| P16 | F | 84 | R. Thalamus | 14 | 26 | 22 | |
| P17 | M | 79 | R. MCA | 14 | 23 | 58 | |
| P18 | M | 78 | R MCA | 13 | 12 | 15 | |
| P19 | M | 67 | R MCA | 14 | 25 | 123 | |
| P20 | M | 58 | R. Thalamus | 14 | 18 | 52 | |
| Mean (SE) |
69.4 (12.0) | 13.9 (0.5) | 20.8 (5.3) | 67.9 (45.3) | |||
Note: F: Female; M: Male; R: Right hemisphere; SE: Standard Error; GCS: Glasgow Coma Scale; MMSE: Mini Mental State Examination score; BIT: Behavioral Inattention Test conventional subtest score; MCA: territory of the Middle Cerebral Artery
Table 1: Demographical and clinical data of 20 patients with unilateral spatial neglect during baseline assessment.
Patients with difficulty communicating due to disturbance of consciousness or dementia and generally unstable physical conditions were excluded from the study. To conduct a crossover comparative study, the patients were randomly divided into two groups. Each group was given a different order of intervention. This study was approved by the Ethics Committee of Kansai Medical University and the Ethics Committee of Kobe University Graduate School of Health Sciences and patients provided informed consent according to the declaration of Helsinki.
Assessment
Disturbances of consciousness, dementia, and unilateral spatial neglect were assessed. Disturbance of consciousness was assessed using the Glasgow Coma Scale (GCS). Dementia was assessed using the Mini Mental State Examination (MMSE). Unilateral spatial neglect was assessed using the BIT, Baking Tray Task (BTT), and Catherine Bergego Scale (CBS).
The GCS is an assessment and classification scale for the disturbance of consciousness presented in 1974 by the University of Glasgow in the UK and is currently widely used worldwide [30]. The MMSE is a questionnaire developed in 1975 in the US to diagnose dementia, which consists of 11 questions with a maximum score of 30 points [31].
The BIT is an international examination method for unilateral spatial neglect that combines six examination categories: (1) line crossing, (2) letter cancelation, (3) star cancelation, (4) copying, (5) line bisection, and (6) drawing tests [32]. The BIT has a cutoff value, and if it falls below that score, unilateral spatial neglect is suspected. The BTT is an examination for unilateral spatial neglect presented by Tham and Tenger, which is reportedly more sensitive than BIT [12,33]. In the BTT, 16 cubes (3.5 cm) are positioned evenly on a 75 cm × 100 cm board, and the number of cubes positioned on the right and left spaces of the board are scored separately. The CBS is a questionnaire that evaluates problems in daily life caused by unilateral spatial neglect [23,34,35]. Items are scored on a 0 to 3 scale of severity, with 0 indicating no neglect and 3 indicating severe neglect. Lower scores on the CBS indicate better functioning (range 0 to 30). The CBS includes observational assessment and selfassessment and uses the value of divergence between the total scores to assess self-awareness regarding unilateral spatial neglect.
In the present study, the initial assessment was conducted within 1 week of onset of disease; on the contrary, the second assessment was conducted after the first intervention period. After a two-day washout period, the third assessment was conducted before the second intervention period. The final assessment was conducted after the second intervention period. All participants completed four assessments.
Intervention
All participants were in the acute stage; therefore, we used a crossover comparative study to eliminate the effects of spontaneous recovery insofar as possible. The patients were randomly divided into two groups. Group A consisted of patients who were administered with Occupational Therapy (OT) without feedback in the first intervention period and OT with feedback in the second intervention period. On the contrary, Group B consisted of patients who were administered with OT with feedback in the first intervention period and OT without feedback in the second intervention period. Each intervention period lasted for 5 days and the washout period lasted for 2 days; the latter was performed to eliminate the effects of the first intervention period.
Intervention method 1-OT without feedback: General OT was conducted, including left arm activation and left-side space scanning tasks. The duration of the intervention was 40 min/ day.
Intervention method 2-OT with feedback: In addition to the 40 minutes of OT per day, fixation data recorded with an eye mark recorder were fed back to the participants. Eye tracking glasses from Senso Motoric Instruments (Germany) were used as the eye mark recorders. For feedback, participant fixation during thesearching task was recorded using the eye mark recorder, and a verbal explanation (such as, "You are not looking at left-side space," or "You keep searching the same place, so search a wider area") was provided while an image or video was presented (Figures 1A and 1B).
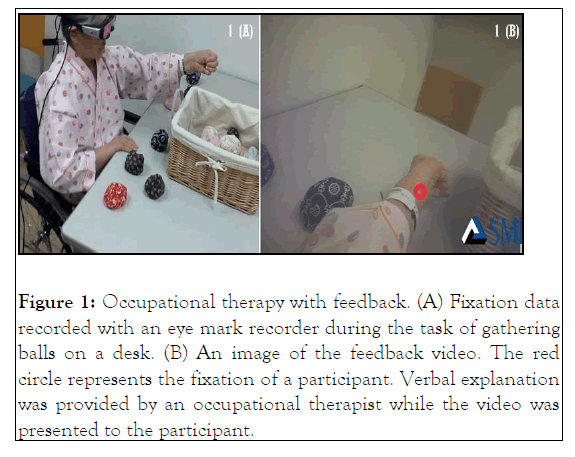
Figure 1: Occupational therapy with feedback. (A) Fixation data recorded with an eye mark recorder during the task of gathering balls on a desk. (B) An image of the feedback video. The red circle represents the fixation of a participant. Verbal explanation was provided by an occupational therapist while the video was presented to the participant.
To prevent a learning effect, we chose tasks that were not directly related to the outcome measures (gathering balls on a desk or naming buildings or articles shown in a picture) for tasks in which feedback was used.
Statistical analysis
The paired t-test was used to examine the effect of the two interventions. The t-test was used to analyze the variation in outcome measures between the two groups. For the BIT, we tested the total and subcategory scores.
Furthermore, we verified the carry-over, treatment, and period effects. The carry-over effect is the effect of a previous experimental treatment that carries over onto a period after the termination of experiment wherein participants no longer experienced the treatment; it was verified by comparing the average values for the sum of time within the group. The treatment effect is the difference in improvement depending on the intervention; it was verified by comparing average values for differences in time within the group. The period effect is the difference in fluctuations depending on the time of intervention, and average values for difference of time were compared; in Group A, average values for the difference of time (intervention method 1-2) and in Group B, average values for the difference of time (intervention method 2-1). Since the carry-over effect has weak power, the significance level was set to 10%, and the significance level of the treatment effect and period effect was set to 5% [36,37]. JMP 14 (SAS Institute Japan Ltd., Japan) was used for the analysis.
All the participants completed the study. To conduct a crossover comparative study, the patients were randomly divided into two groups. No significant difference was observed regarding the characteristics between the two groups.
At the end of OT with feedback intervention, the mean scores significantly improved in the outcome measures (the GCS, MMSE, BIT, BTT, and CBS). On the contrary, OT without feedback significantly improved the scores of all outcome measures; except for the GCS score (Table 2).
| OT with feedback | p-value | OT without feedback | p-value | |||
|---|---|---|---|---|---|---|
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||
| GCS | 13.9 (0.6) | 14.4 (0.5) | <0.01 | 14.2 (0.7) | 14.3(0.7) | 0.16 |
| MMSE | 20.5 (5.2) | 22.0 (4.9) | <0.01 | 20.5 (5.7) | 22.1 (5.3) | <0.01 |
| BIT | 68.5 (45.2) | 99.8 (39.0) | <0.01 | 81.6 (42.8) | 92.2 (43.8) | <0.01 |
| BTT | 1 (2.0) | 3 (3.1) | <0.01 | 1.7 (2.7) | 2.3 (3.1) | 0.03 |
| CBS | 19.0 (8.4) | 9.3 (7.3) | <0.01 | 15.1 (9.6) | 12.0 (9.7) | <0.01 |
GCS: Glasgow Coma Scale; MMSE: Mini Mental Status Examination; BIT: Behavioral Inattention Test; BTT: number of cubes positioned on the left-side spaces of the board in the Baking Tray Task; CBS: score of divergence between observational assessment and self-assessment in the Catherine Bergego Scale; OT: Occupational Therapy
Table 2: The mean for each outcome measure between two interventions (standard error in parenthesis).
No significant difference was observed regarding the carry-over effect in all outcome measures. The treatment and period effectsof the GCS scores were significant (p=0.02 and p=0.04, respectively). Only the treatment effect of the BIT scores was significant (p=0.04). Moreover, significant differences were observed in the treatment effect for the following two subtest categories: the line crossing (treatment effect, p<0.01; period effect, p=0.21) and the line bisection test (treatment effect, p=0.03; period effect, p=0.26).
In the other subtest categories, no significant difference in treatment effect was observed. Similarly, only the treatment effect of the CBS score was significant (p=0.01). There was no significant difference in the treatment effect of the MMSE score (p=0.14) or BTT score(p=0.09) due to the intervention method (Table 3).
| Carry-over effect | Treatment effect | Period effect | |
|---|---|---|---|
| GCS | 0.17 | 0.02 | 0.04 |
| MMSE | 0.87 | 0.14 | 0.8 |
| BIT | 0.39 | 0.04 | 0.07 |
| LCr | 0.22 | <0.01 | 0.21 |
| LCa | 0.55 | 0.06 | 0.02 |
| SC | 0.68 | 0.26 | 0.4 |
| Co | 0.17 | 0.46 | 0.15 |
| LB | 0.16 | 0.03 | 0.26 |
| Dr | 0.8 | 0.87 | 0.62 |
| BTT | 0.92 | 0.09 | 0.02 |
| CBS | 0.69 | 0.01 | 0.06 |
GCS: Glasgow Coma Scale; MMSE: Mini Mental Status Examination; BIT: total score of Behavioral Inattention Test; LCr: Line Crossing test; LCa: Letter Cancelation test; SC: Star Cancelation test; Co: Copying test; LB: Line Bisection test; Dr: Drawing test; BTT: Baking Tray Task; CBS: Catherine Bergego Scale
Table 3: Verification of the carry-over effect, treatment effect and period effect by the t-test (p-value).
This study investigated the benefits of fixation feedback using an eye mark recorder on patients with unilateral spatial neglect. Individual differences are observed in the symptoms of unilateral spatial neglect; furthermore, acute patients demonstrate spontaneous recovery which results in symptomatic improvement. Considering these factors, we believe that a crossover comparative study would enable us to highlight the treatment effect of fixation feedback. Hence, patients were divided into two groups to analyze variations in outcome measures associated with the presence or absence of fixation feedback.
Two outcome measures were used; namely, the BIT and CBS scores. In these measures, the treatment effect was significantly different; however, no significant differences were observed inthe carry-over and period effects. The treatment effect refers to the difference in variation due to the presence or absence of fixation feedback; therefore, the significant treatment effect indicates that OT with feedback had a greater treatment effect compared to OT without feedback. However, this is predicated on the non-significance of the carry-over effect, this is predicated on the non-significance of the carry-over and period effect, which were described in previous sections. Therefore, the effect of the intervention is not considered if the changes occur because of the intervention order or gradual improvement. Our present results suggest that the BIT and CBS scores showed improvement specifically because of fixation feedback, which was not associated with the intervention order and gradual improvement. Previous studies have reported that patients who demonstrated positive changes in self-awareness showed improved scores on neuropsychological tests [23,38]. Similarly, the present study found a correlation between improved scores on neuropsychological tests and changes in self-awareness.
This study was conducted over a short period of only 2 weeks. Nevertheless, a large standard deviation was obtained for each outcome measure; therefore, improvement over time would likely produce a period effect if the intervention period was long. We believe that the significant period effect of the GCS score may be attributed to the improvements in the disturbance of consciousness that can be observed even in the acute stage.
Among the subtest categories of the BIT, fixation feedback was thought exerted a strong effect on the line crossing and line bisection tests. The improvements in these two tests may be attributed to the tasks used for fixation feedback. Therefore, it is possible that, through fixation feedback, patients learned to use searching eye movements in the left-side space. However, no significant treatment effects were observed in other subtest categories. The visual scanning training improves the neuropsychological test scores of patients with unilateral spatial neglect; however, previous reports have found that these effects are limited to examination categories that are highly similar to the training content [12,39]. Considering this, fixation feedback may have a small effect on letter cancelation and star cancelation tests, searching tasks that incorporate interference stimuli, and copying and drawing tests, which are strongly impacted by movement planning. These results suggest that fixation feedbackmay improve searching eye movements in patients with unilateral spatial neglect.
Fixation feedback was also associated with significant improvement of the CBS score; this indicates that fixation feedback improved the self-awareness of patients with unilateral spatial neglect. Langer and Padrone cited that the lack of information and inability to understand the meanings of information were causes of disordered self-awareness [40]. We believe that our study offers information regarding the condition for better understanding of patients. Furthermore, this intervention does not simply provide verbal feedback to encourage patients to search for left-side space; rather, it simultaneously utilized verbal and visual feedback, which presents the participants’ fixation in a visual form. A study by Crosson categorizes self-awareness as intellectual, physical, and anticipatory awareness; furthermore, he proposes a hierarchy for these categories [41]. The CBS is a questionnaire; therefore, it is classified as a measure of intellectual awareness. If fixation feedback is found to be an intervention that encourages the acquisition of intellectual awareness, then it may lead to the subsequent acquisition of physical and anticipatory awareness.
Tham states that improvement due to video feedback for unilateral spatial neglect and self-awareness is only produced in tasks with feedback and cannot be generalized to other tasks [12]. Similarly, in this study, improvements in unilateral spatial neglect symptoms were observed in tasks that used fixation feedback and on comparatively similar outcome measures. However, improvement and self-awareness extended to questions in daily life that were unrelated to tasks that used fixation feedback. This discrepancy may be attributed to using the firstperson perspective in the video shots, which provided feedback that clearly displayed the fixation of the participant; on the contrary, Tham’s research used video shots from the thirdperson perspective. Additionally, the fixation feedback in this study provided information that patients easily understood which may have encouraged self-reflection. Furthermore, a major factor in the generalization of the treatment effects to everyday life was that participants needed to modify fixation movements, namely, eye movements and searching behavior, rather than movements for a specific task. Therefore, it is possible that this resulted in an improvement in self-awareness. The eye mark recorder was originally used for assessment; however, this study suggests its potential as a new intervention method for unilateral spatial neglect.
Based on our present findings, fixation feedback using an eye mark recorder may provide even more powerful results than normal OT interventions as a top-down approach to unilateral spatial neglect.
We used a crossover comparative study to assess the effects of intervention on unilateral spatial neglect, a condition that exhibits significant individual differences in symptom presentation. Originally, crossover comparative studies are often used for chronic illnesses and are considered unsuitable for patients in the acute stage of the disease where spontaneous recovery may occur, as in the sample used in this study. Additionally, the number of participants was limited to 20 with no assigned control group. Therefore, the risk of bias included in these results cannot be ruled out. All participants in thisstudy were patients with stroke in the acute stage; however, the affected site varied. Many studies have reported that the symptoms of unilateral spatial neglect and the recovery process differ based on the site of damage. Future studies should focus on the intervention effects according to the site of damage.
Citation: Hashimoto S, Tanemura R (2021) Effect of Fixation Feedback Using an Eye Mark Recorder on Unilateral Spatial Neglect: A Crossover Comparative. Int J Phys Med Rehabil. 9:610.
Received: 03-Sep-2021 Accepted: 20-Sep-2021 Published: 27-Sep-2021 , DOI: 10.35248/2329-9096.21.9.610
Copyright: © 2021 Hashimoto S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.