International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2020)Volume 8, Issue 6
Background: This research study aims to find the effect of modified bobath cuff on energy expenditure and fatigue during level surface walking among subjects with hemiplegic shoulder subluxation.
Objective: The objective of this study is to measure the amount of energy consumption during level surface walking among hemiplegic subjects having shoulder subluxation with modified bobath cuff. The objective of this study is to measure the fatigue of hemiplegic subjects having shoulder subluxation with modified bobath cuff.
Subjects and method: 30 subjects with shoulder subluxation were included in this study by a convenient sampling method. The subjects were given with a modified bobath cuff. The cardiorespiratory parameters (VO2, VCO2, and energy expenditure) were measured using COSMED k4b2 and fatigue was measured using the MFI20 questionnaire. All the measurements were acquired before the use of bobath cuff and 2 weeks following the onset of bobath cuff use.
Results: There was a significant difference between in cardiorespiratory functions the two conditions following the application of bobath cuff with p<0.05. There was a significant difference in general and mental fatigue but no difference was found in physical, reduced activity, and reduced motivation.
Discussion and conclusion: The modified bobath cuff is significantly efficient in terms of energy expenditure and fatigue in subjects with shoulder subluxation.
Modified bobath cuff; Shoulder subluxation; Cardiorespiratory functions; Fatigue; MFI scale
Stroke (cerebrovascular accident) is an acute neurologic syndrome that reflects focal involvement of the central nervous system and is due to a disturbance of the cerebral circulation [1-3]. Asymmetrical hemiplegic stroke gait has an irregularity in gait spatial and temporal parameters including posture control, muscle weakness, abnormal muscle tone, and abnormal muscle activation patterns, mostly affecting the paretic side [4]. Cerebrovascular disorders (CVD) are increasing in prevalence and incidence in India due to the rapid escalation of risk factors including hypertension, diabetes mellitus, smoking, and obesity affecting the considerable proportion of the adult population [5]. The global burden of disease study shows that of the 9.4 million deaths in India, 619,000 were due to stroke, and disability-adjusted life years (DALYs) lost were 28.5 million highlighting the fact that CVD leads to considerable mortality and morbidity [6].
Among the entire patho-hemiplegic gait with influences of pain and damaged joint kinematics, and increased energy expenditure during the performance of activities of daily living (ADL) is noticed [7-9]. Active rehabilitation including bracing on stroke hemiplegia is the standard choice for clinicians [10-12]. Stroke hemiplegia with upper extremity shoulder subluxation, is a common clinical problem with pain, limitation of movement, injury to the neurovascular tissues around the shoulder joints, and delayed neurological recovery [13-16].
To stop shoulder subluxation progression general clinical principal is to provide arm support by pillow with proper positioning of upper limbs and lower limbs within a wheelchair or other standard medicated assistive devices [17-19]. The shoulder sling is the best clinical non-operative option to decrease pain and stop subluxation in standing posture and gait [20].
The shoulder sling is still standard treatment modality for shoulder subluxation in stroke patients [19-22]. Shoulder strapping is useful in the first period after stroke [21-24].
The bobath sling is designed to provide comfort for the patients and to manage shoulder subluxation. The strap goes behind the unaffected side as well as to the affected side of the subluxed shoulder. Additional straps with two straps on each side of the shoulder connect in a figure-of-eight across the trunk. Besides, the shoulder with the subluxation has a pad beneath the proximal humerus for support. The pad is designed to position the humerus into the abduction and to avoid internal rotation of the humerus. The main purpose of the bobath sling is to decrease the shoulder subluxation, normalize muscle tone, as well as prevent internal rotation of the humerus and maintain a relaxed arm position. This technique is aimed to decrease the chance of developing contractures by placing the arm in a neutral position and allowing arm movement.
Uninhibited primitive reflexes are responsible for this posture caused pelvic retraction and elevation, hip extension, adduction, and internal rotation; knee extension; plantar flexion of the ankle; and, inversion of the foot [25]. So the common problems associated with hemiplegia in upper extremity y is characterized by flexion contractures of the elbow, wrist, and fingers, a frozen shoulder, painful hemiplegic shoulder, shoulder subluxation, and shoulder hand syndrome. In lower limb hip contracture spasticity, genu recurvatum, knee flexion contracture, equino- varus contracture of ankle joint, foot drop, and claw toes respectively [26].
Human locomotion involves smooth advancement of the body through space with the least mechanical and physiological energy expenditure [27], but the gait of hemiplegic patients with stroke is characterized by asymmetry in stride times and stride length, slow velocity, poor joint and posture control, muscle weakness, abnormal muscle tone and abnormal muscle activation patterns, mostly affecting the paretic side [4]. The persistent gait deviation increases energy expenditure [7] and can lead to pain and joint damage [8]. Besides, in hemiplegic patients, it was reported that the energy expenditure was increased during the performance of activities of daily living (ADL) due to the impairment of cardiopulmonary functions, therefore, the cardiovascular loading was also increased [9]. Minimization of unnecessary energy expenditure and cardiovascular loading during gait would be important for gait rehabilitation in patients with stroke.
Energy expenditure of walking for persons with hemiplegia is variable, depending on the extent of neurologic dysfunction and spasticity. The hemiplegic population generally consists of older individuals with a high prevalence of cardiovascular disease, who are often further deconditioned by the effects of acute illness and bed rest before active rehabilitation. Exercise capacity is therefore typically reduced. Because of the marked reduction in the speed of walking, the rate of oxygen consumption during walking for persons with hemiplegia is less than the rate for normal subjects walking at their customized walking speed, despite the in- efficiency of the gait pattern and high energy cost [9-11,28-31].
Most of the studies in this field have concentrated on the effect of different kinds of slings and other conventional management for the prevention of shoulder subluxation. There is a little effective study on the impact of bobath cuff on energy expenditure, in hemiplegic subjects with shoulder subluxation. So this study might be helpful to provide objective data on modified bobath cuff which have been in controversy over their usefulness and effect on energy expenditure. This study is mainly focused on the effect of energy expenditure, maximal aerobic capacity (VO2 max), maximal anaerobic capacity (VCO2), and heart rate along with fatigue in subjects with hemiplegic shoulder subluxation.
The study was approved by the ethical committee of the National Institute for Locomotor Disabilities (Divyangjans), Kolkata, India. The study period was for 1 year and was performed at the dept. of prosthetics and orthotics, National Institute for Locomotor Disabilities (Divyang jan), B.T. road, Bon-Hooghly, Kolkata-700090. The study population was subjects with hemiplegic shoulder subluxation, the sample size was taken 30, sampling design was a convenient sampling design, the study design was prospective pre-post quasi-experimental study design, and the subject design was same controlled design.
The inclusion criteria were both male and female, with an age range of 40-65 years; the patient diagnosed with hemiplegic shoulder subluxation and must be ambulatory, patient continuing therapy session, ability to understand and follow the command, and with Brunnstrom stage 3-5 (Figure 1). Parameter studied are energy expenditure (kcal/min/m), maximum aerobic capacity (VO2 max) (ml/min), maximum anaerobic capacity (VCO2 max) (ml/min), heart rate (beats per minute), O2 expenditure. Study tool and instrument used is Cosmed-k4b2. Independent Study variable was modified bobath cuff and dependent was energy consumption.
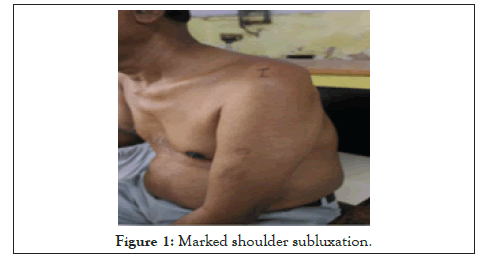
Figure 1: Marked shoulder subluxation.
The study procedure was from March 2017 to February 2018, acute stroke patients presenting with hemiplegia and shoulder subluxation were recruited to the study. The subjects were screened first according to the inclusion and exclusion criteria reported to the NILD OPD. Aim of the study and procedure was explained to the selected patient. Informed consent was obtained from all participants, and the study was approved by the institutional ethical and scientific committee before patients were recruited. Participants were assessed and evaluated. The demographic data like age, gender, height, and body weight were taken. Orthotic assessment and physical evaluation for shoulder subluxation was done. The distance between the inferior border of the acromion and the upper border of the humeral head was measured, as determined by palpation, with a tape measure. The subacromial gap measurement was determined using a tape measure with the patient sitting unsupported in an upright posture without a backrest or armrests, with the arm in a neutral position hanging by the side of the body.
The subjects (n=30) were asked for a 20-meter walk test at a self-selected speed. Then the standard parameters for the cardiorespiratory functions like PCI/O2 expenditure, VO2, VCO2, heart rate, and energy expenditure were then recorded using COSMED k4b2. The subjects then called for the follow- up and post-intervention data was taken. With the application bobath cuff subjects were asked to walk for a 20-meter walkway test at a self-selected speed and then the standard parameters for the cardio-respiratory functions like O2 expenditure, VO2, VCO2, heart rate and energy expenditure was measured using Cosmed k4b2 along with the fatigue through mfi20 questionnaire (Figure 2). After the pre and post data collection, data analysis was done using statistical tools.
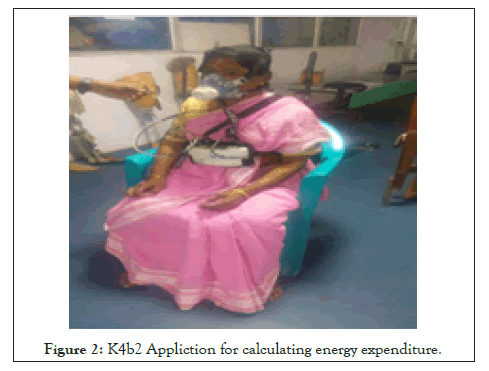
Figure 2: K4b2 Appliction for calculating energy expenditure.
Before testing, both the Cosmed K4b2 and the Medgraphics analysers were warmed-up for a minimum of 20 minutes. Following the warm-up period, the O2 and CO2 analysers of both systems were calibrated using reference gases of known concentrations. Each participant completed two trials in the same session which varied only concerning the device used to measure VO2 (Cosmed K4b2 or Medgraphics). The test order was randomly determined. Although the Cosmed K4b2 is designed to facilitate the measurement of VO2 and VCO2 in a non-laboratory setting, a treadmill was used to ensure a constant walking speed and facilitate comparison of data from the two analysers. Participants were permitted to select their own “comfortable” walking speed, which ranged from 2.7-4.6 mph, at 0%grade. Both tests were performed at this identical speed with a 10-minute “wash-out” period in between.
After an initial 10 minute rest period, participants were fitted with either the Medgraphics system or Cosmed K4b2 analyser, then continued to sit for two additional minutes to allow adaptation to the equipment. After 2 minutes, the participant stood for 30 seconds and allowed to walk for 30 meters self-selected velocity in level surface walking. The test was stopped and the participant was immediately seated, with breath collection continuing for an additional 2 minutes.
After completing the first test, the analyser was removed and the participant rested for 10 minutes while seated. Immediately following the rest period, a second test was performed using the alternate system and following the procedures described above [32].
The k4b2 is the first COSMED portable system for intrapulmonary gas exchange analyser on a true breath by breath basis. Sports medicine, research, human performance, gait lab, occupational health, cardiology, cardiac rehabilitation, clinical nutrition, and application that requires the measurements of the cardiorespiratory response either in the field or in the lab. Several methods can be used to validate devices that predict energy expenditure: Indirect calorimetry: this method measures respiratory gas exchange (oxygen uptake and carbon dioxide production) to allow calculation of energy expenditure. Room calorimetry: this method involves a specially designed chamber that houses an individual for extended periods. Energy expenditure can be determined either through indirect calorimetry (gas exchange) or through direct calorimetry (heat production).doubly-labelled water (dlw): in this method, a person drinks water containing stable isotopes of hydrogen and oxygen, which then equilibrate in the body. carbon dioxide production is determined from the differential rate of elimination of 2 h and 18 min. Direct observation: in this method, investigators keep a log of the time spent doing different activities, and the energy cost of these activities is then determined from the compendium of physical activities indirect calorimetry appropriate criterion for minute-by-minute energy expenditure.
The Cosmed k4b2 is an example of portable metabolic measurement systems that measure gas exchange (VO2 and VCO2) and calorie expenditure [33]. K4b2 instruments were validate with the pilot study and original research work in this study set up with the affiliation with The West Bengal University of Health Sciences, Kolkata.
The modified bobath cuff is the combination of bobath shoulder roll and the roylan humeral cuff. The modified bobath cuff consisted of a humeral cuff section which is made up of the drill cloth and inside the drill cloth, a 2 mm evathene foam was used. The standard measurements were taken for the construction of the cuff by taking the maximum and minimum arm circumference and the distance from the acromion to 2” above the lateral epicondyle. Then the cuff was stitched and a bobath roll using 2 mm evathene foam and drill cloth was made and attached to the bobath cuff through Velcro hook and loop. The bobath cuff was worn over the subluxed side and a strap passes under the axilla of the sound side and fastened through Velcro attachment. The bobath roll provides an upward directed force which keeps the humerus against the gravity and thus the cuff suspension (Figure 3).
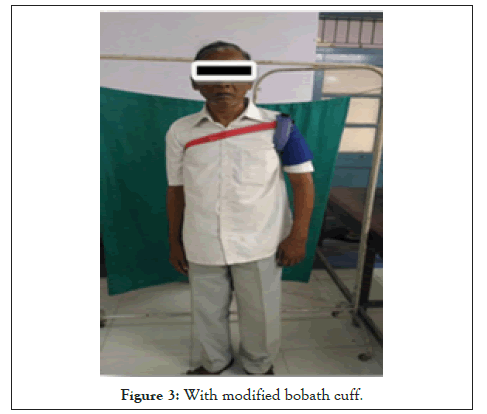
Figure 3: With modified bobath cuff.
For statistical analysis, data were entered into a Microsoft Excel spread sheet and then analysed by SPSS 24.0. And graph pad prism version 5. Paired t-tests were a form of blocking and had greater power than unpaired tests. Explicit expressions that can be used to carry out various t-tests are given below. In each case, the formula for a test statistic that either exactly follows or closely approximates a t-distribution under the null hypothesis is given. Also, the appropriate degrees of freedom are given in each case. Each of these statistics can be used to carry out either a one- tailed test or a two-tailed test. Once the t-value is determined, a p-value can be found using a table of values from the student’s t-distribution.
This study shows that the mean difference in the distribution of the VO2(ml/min) in the two groups was found to be statistically significant (p<0.0001); mean difference of the VCO2 (ml/min) in two groups was statistically significant (p<0.0001); mean difference of the O2 expenditure between two groups was found statistically significant (p<0.0001); the mean difference of the heart rate between two groups was found with p=0.4065; and the mean difference of the energy expenditure (kcal/min) between two groups was found to be statistically significant (p<0.0003) respectively (Table 1 and Figure 4).
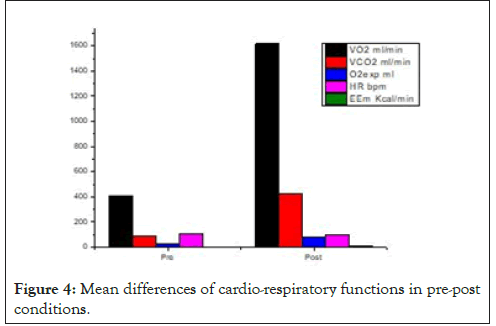
Figure 4: Mean differences of cardio-respiratory functions in pre-post conditions.
| Number | Mean | SD | Minimum | Maximum | Median | T Statistic | p-value | |||
|---|---|---|---|---|---|---|---|---|---|---|
| VO2 ml/min | POST | 30 | 1617.0636 | 262.3070 | 1007.5300 | 2028.1634 | 1633.5155 | 24.3054 | <0.0001 | |
| PRE | 30 | 409.1040 | 72.7687 | 234.7961 | 518.4480 | 429.5524 | ||||
| VCO2 ml/min | POST | 30 | 426.9122 | 76.1173 | 246.5148 | 540.5641 | 440.6166 | 23.0871 | <0.0001 | |
| PRE | 30 | 88.0264 | 25.8840 | 51.5092 | 148.8104 | 80.8338 | ||||
| O2 exp ml | POST | 30 | 76.8354 | 11.1267 | 55.9972 | 94.2466 | 78.2838 | 21.2564 | <0.0001 | |
| PRE | 30 | 27.8798 | 5.9436 | 15.1978 | 41.3100 | 27.3866 | ||||
| HR bpm | POST | 30 | 102.2000 | 11.3757 | 82.0000 | 128.0000 | 103.5000 | 0.8362 | 0.4065 | |
| PRE | 30 | 105.0000 | 14.3863 | 85.0000 | 133.0000 | 105.5000 | ||||
| EEm Kcal/min | POST | 30 | 6.6422 | 1.0852 | 4.1144 | 8.3372 | 6.7195 | 3.8632 | 0.0003 | |
| PRE | 30 | 4.6968 | 2.5357 | 0.9821 | 7.5366 | 5.8887 | ||||
Table 1: Distribution of mean, median and standard deviation of two groups in pre and post condition for cardio-respiratory parameters.
From the result of MFI 20 fatigue scale it was found that the mean difference of general fatigue between two conditions was 0.109 with statistically significant for question number 1, 3 and 4 (p<0.0001). The mean difference of mental fatigue is 0.292 with statically significant (p<0.0001).the mean difference of physical fatigue between two conditions was 0.217 with statistically significant for question number 2, 3, and 4 (p<0.0001).the mean difference of reduced activity between two conditions was 0.2 with statistically significant for question number 1,2, and 3 (p<0.0001). The mean difference of reduced motivation between two conditions was 0.333 with statistically significant for question number 1, 3, and 4 (p<0.0001) (Table 2 and Figures 5-9).
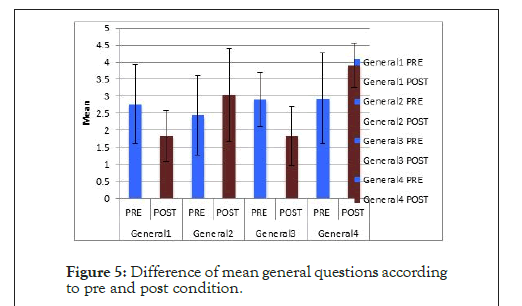
Figure 5: Difference of mean general questions according to pre and post condition.
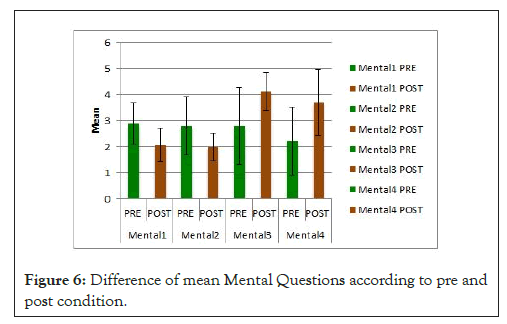
Figure 6: Difference of mean Mental Questions according to pre and post condition.
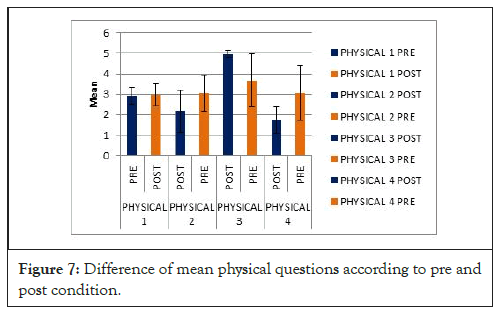
Figure 7: Difference of mean physical questions according to pre and post condition.
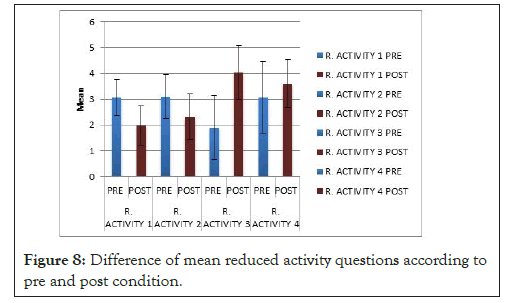
Figure 8: Difference of mean reduced activity questions according to pre and post condition.
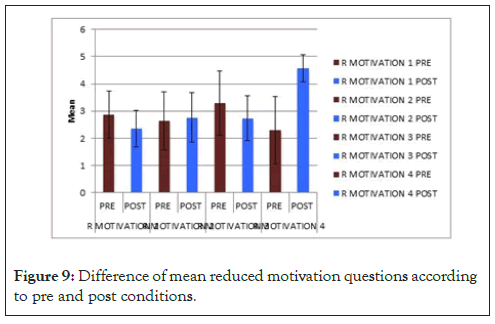
Figure 9: Difference of mean reduced motivation questions according to pre and post conditions.
| Number | Mean | SD | Minimum | Maximum | Median | T Statistic | p-value | ||
|---|---|---|---|---|---|---|---|---|---|
| Mental 1 | PRE | 30 | 2.9 | 0.803 | 1 | 4 | 3 | 4.4458 | <0.0001 |
| POST | 30 | 2.0667 | 0.6397 | 1 | 3 | 2 | |||
| Mental 2 | PRE | 30 | 2.8 | 1.1265 | 1 | 5 | 2 | 3.5254 | 0.0008 |
| POST | 30 | 2 | 0.5252 | 1 | 3 | 2 | |||
| Mental 3 | PRE | 30 | 2.8 | 1.4716 | 1 | 5 | 3 | 4.4454 | <0.0001 |
| POST | 30 | 4.1333 | 0.7303 | 3 | 5 | 4 | |||
| Mental 4 | PRE | 30 | 2.2333 | 1.3047 | 1 | 5 | 2 | 4.4229 | <0.0001 |
| POST | 30 | 3.7 | 1.2635 | 2 | 5 | 4 | |||
| General1 | PRE | 30 | 2.7667 | 1.1651 | 1 | 4 | 3 | 3.6942 | 0.0005 |
| POST | 30 | 1.8333 | 0.7466 | 1 | 3 | 2 | |||
| General2 | PRE | 30 | 2.4333 | 1.1651 | 1 | 5 | 3 | 1.8418 | 0.0706 |
| POST | 30 | 3.0333 | 1.3515 | 1 | 5 | 3 | |||
| General3 | PRE | 30 | 2.9 | 0.803 | 1 | 4 | 3 | 4.9216 | <0.0001 |
| POST | 30 | 1.8333 | 0.8743 | 1 | 3 | 2 | |||
| General4 | PRE | 30 | 2.9333 | 1.3374 | 1 | 5 | 3 | 3.5484 | 0.0008 |
| POST | 30 | 3.9 | 0.6618 | 3 | 5 | 4 | |||
| Physical 1 | PRE | 30 | 2.9333 | 0.403 | 1 | 4 | 3 | 0.371 | 0.9023 |
| POST | 30 | 2.9675 | 0.5497 | 1 | 4 | 3 | |||
| Physical 2 | POST | 30 | 2.1667 | 1.0532 | 1 | 4 | 2 | 3.4427 | 0.0011 |
| PRE | 30 | 3.0333 | 0.8899 | 1 | 5 | 3 | |||
| Physical 3 | POST | 30 | 4.9667 | 0.1826 | 4 | 5 | 5 | 5.4427 | <0.0001 |
| PRE | 30 | 3.6667 | 1.2954 | 1 | 5 | 4 | |||
| Physical 4 | POST | 30 | 1.7333 | 0.6397 | 1 | 3 | 2 | 4.9262 | <0.0001 |
| PRE | 30 | 3.0667 | 1.3374 | 1 | 5 | 3 | |||
| R. Activity 1 | PRE | 30 | 3.0667 | 0.6915 | 1 | 5 | 3 | 5.8431 | <0.0001 |
| POST | 30 | 1.9667 | 0.7649 | 1 | 3 | 2 | |||
| R. Activity 2 | PRE | 30 | 3.1 | 0.8449 | 1 | 5 | 3 | 3.4339 | 0.0011 |
| POST | 30 | 2.3333 | 0.8841 | 1 | 4 | 2 | |||
| R. Activity 3 | PRE | 30 | 1.9 | 1.2415 | 1 | 4 | 1 | 7.2338 | <0.0001 |
| POST | 30 | 4.0333 | 1.0334 | 2 | 5 | 4 | |||
| R. Activity 4 | PRE | 30 | 3.0667 | 1.388 | 1 | 5 | 2.5 | 1.7472 | 0.0859 |
| POST | 30 | 3.6 | 0.9322 | 2 | 5 | 4 | |||
| R Motivation 1 | PRE | 30 | 2.8667 | 0.8604 | 1 | 5 | 3 | 2.5133 | 0.0148 |
| POST | 30 | 2.3667 | 0.6687 | 1 | 3 | 2 | |||
| R Motivation 2 | PRE | 30 | 2.6333 | 1.0662 | 1 | 4 | 3 | 0.524 | 0.6023 |
| POST | 30 | 2.7667 | 0.8976 | 1 | 4 | 3 | |||
| R Motivation 3 | PRE | 30 | 3.3 | 1.1788 | 1 | 5 | 3 | 2.1548 | 0.0353 |
| POST | 30 | 2.7333 | 0.8277 | 1 | 4 | 3 | |||
| R Motivation 4 | PRE | 30 | 2.3 | 1.236 | 1 | 5 | 2 | 9.3013 | <0.0001 |
| POST | 30 | 4.5667 | 0.504 | 4 | 5 | 5 |
Table 2: Distribution of mean, median and standard deviation of two groups in pre and post condition for mfi-20 scale parameters.
Given the above background, we speculated that minimization of unnecessary energy expenditure and cardiovascular loading during gait would be important for gait rehabilitation in stroke patients. Although there has been controversy on the efficiency of an arm sling for treatment of shoulder subluxation or pain, it was reported that an arm sling improved gait pattern [34]. This study provides a rationale for the prescription of bobath cuff in improving the energy expenditure and fatigue in subjects with hemiplegic shoulder subluxation.
Given the above background, we speculated that minimization of unnecessary energy expenditure and cardiovascular loading during gait would be important for gait rehabilitation in stroke patients. Although there has been controversy on the efficiency of an arm sling for treatment of shoulder subluxation or pain, it was reported that an arm sling improved gait pattern [35]. This study provides a rationale for the prescription of bobath cuff in improving the energy expenditure and fatigue in subjects with hemiplegic shoulder subluxation.
Most of the studies on the effect of supplemental aids on oxygen consumption and energy expenditure have been conducted with a main focus on the lower extremities. Study of the effect of supplemental aids for upper extremities on oxygen consumption and energy expenditure is rare.
Hanada and Kerrigan [36] reported that arm immobilization did not increase energy expenditure during level walking at a comfortable gait speed in a healthy person. In this current study it was found that there is a significant difference in energy expenditure with and without the application of the bobath cuff, with a mean difference of 1.9454 which is supported by Kim et al. [37] reporting that arm restriction while walking resulted in significant changes in energy consumption [35,36]. The rate of O2 cost determines the total time required to perform the task of walking. O2 cost may be elevated by either an increased O2 rate or by a low walking speed with a normal rate of O2 consumption.O2 cost may be elevated by either an increased O2 rate or by a low walking speed with a normal rate of O2 consumption, which was observed by waters 1999. In this current study, the O2 consumption rate is high with bobath cuff and low without the same. So, this resistance with bobath cuff of O2 cost (p<0.0001) is adopted by the patients and there is no complaint of cardiorespiratory functions was observed [27].
Acctoastra and Waters et al. the maximal aerobic capacity (VO2 max) is the highest oxygen uptake an individual can attain during physical work while breathing air at sea level. It is the single best indicator of physical fitness [37-39]. Generally, an individual can reach his VO2 max within 2-3 min of exhausting work. Thereafter, the maximum oxygen uptake declines primarily due to a decrease in maximum heart rate. So in this current study the heart rate is decreased with bobath cuff, and VO2 is increased but as such, no cardiorespiratory issue is observed. Astrandsand waters found a proportional relationship between VO2 and heart rate but in this study, the result shows the inversely proportional relationship between VO2 and heart rate with the application of bobath cuff (p<0.0001). Saltin et al. [40] stated that bed rest for 3 weeks can result in a 27% decrease in the VO2 max by decreasing cardiac output, stroke volume, and other factors. So, in the current study without bobath cuff, the VO2 is decreased but with bobath cuff, the post data shows a significant difference in increase VO2. So bobath cuff has a significant effect to increase VO2 max to improve the subluxation and to provide a good cardiorespiratory function [39].
When performing exercise at the same rate of O2 uptake, higher heart rates are associated with leg exercise than with arm exercise. In our study for the short term effect of bobath cuff the heart rate decreased but VO2 increases. So, heart rate is not co-related with VO2, and any cardiorespiratory issues didn’t come out. so, decreasing hour have no direct effect on VO2.similarly, with an increase in VO2 max there is a proportional increase in VCO2 with the application of bobath cuff with a statistically significant difference.
Fatigue after stroke lacks an unambiguous definition and appears to be a multidimensional concept including physical and mental factors. Fatigue in stroke patients has been associated with the higher metabolic load stroke patients experience during activities of daily living. Many patients report fatigue as one of the most difficult sequels to which to adjust 1-5. Previous studies indicated post-stroke fatigue to develop in 39%-69% of patients; the percentage increasing with time from onset 1-9 in this study the fatigue was measured using the mfi20 questionnaire where 5 different kinds of dimensions were postulated to assess the fatigue [40].
In the case of general fatigue, the mean difference between pre and post condition was 0.109 with a decrease in fatigue after the application of bobath cuff similarly a decrease in a mean difference of 0.292 is found in mental fatigue. Whereas there is no such decrease in mean fatigue in physical, reduced motivation, and reduced activity. Reduced motivation and mental fatigue had the highest mean scores (0.33 and 0.29 respectively), and general fatigue with the lowest (0.10). This finding may result in acceptance of bobath cuff in general where the patients feel proper control in his body and thus he feels able to perform certain tasks. With a decrease in mental fatigue after the application of bobath cuff the patients have better control over his/her thoughts and he can regain his inner conscience of doing the respective work [41].
Water et al. suggested that human locomotion involves smooth advancement of the body through space with the least mechanical and physiological energy expenditure, but the gait of hemiplegic patients with stroke is characterized by asymmetry in stride times and stride length, slow velocity, poor joint and posture control, muscle weakness, abnormal muscle tone and abnormal muscle activation patterns, mostly affecting the paretic side. Thaut et al. reported that the energy expenditure was increased of hemiplegic subjects during the performance of activities of daily living (ADL) due to the impairment of cardiopulmonary functions, increasing, the cardiovascular loading.
In normal human locomotion, the role of the upper extremity is to maintain a synchronize, supportive and rhythmic action concerning the head and torso. Where the arms support the opposite reaction forces while walking for the lower extremity in the case of shoulder subluxation, the muscles of the affected side fail to do the same and thus the sound side muscles work in a hyperactive manner to maintain the reaction force, and thus more energy consumption is required by the extremity. With the application of the bobath cuff, the affected side or the paretic arm helps to absorb some amount of these reactive forces and thus helps to minimize the loading on the sound side thereby decreasing the energy expenditure.
Much evidence-based practice suggested that stroke patients having asymmetrical gait pattern with high-level energy expenditure. We observed in this study the bobath cuff maintains congruency of the Glenohumeral joint by minimizing the subluxation and patients doing ADL activities without any cardio-respiratory problems or energy expenditure because of corrective alignment of the shoulder joint by bobath cuff.
MThe present study concluded that the modified bobath cuff is effective in terms of energy expenditure and fatigue in hemiplegic subjects with shoulder subluxation. Although some parameters showed a negative result it does not show any ill effects on cardiorespiratory function among the subjects. The bobath cuff is efficient among hemiplegics without any restriction to cardiorespiratory and metabolic functions. It helps patients to maintain the corrective alignment of Glenohumeral joint for the prevention of further progression of shoulder subluxation. The application of bobath cuff also results in a decrease in post fatigue after the stroke and thus the patient can regain the ability to do his/her ADL activities independently without any complaint of fatigue less.
The limitation of our study was a relatively small sample size for a more detailed analysis of the influence of the examined factors on the outcomes measured. The sample was obtained at a single centre; although it is reflective of this centre, it may differ from the stroke rehabilitation populations at other centres. The adaptation period for the orthosis is less which affects the outcome of the result.
All authors substantially contributed to the acquisition, analysis and interpretation of data for the work. RM was responsible for the work, analyzed and interpreted the data and drafted the manuscript (55%). SS supervised the field methods and provided critical revision (20%). YM, MK and MT (5% each) obtained the data and provided critical revision. HK assisted with data analysis (10%).
The authors declare there are no competing interests.
Citation: Dash R, Raihan HMA, Biswas A, Lenka P (2020) Effect of Modified Bobath Cuff on Energy Expenditure and Fatigue during Level Surface Waking among Subjects with Hemiplegic Shoulder Subluxation: A Prospective study. Int J Phys Med Rehabil 8: 569. DOI: 10.35248/2329-9096.20.08.569
Received: 15-May-2020 Accepted: 05-Jun-2020 Published: 12-Jun-2020 , DOI: 10.35248/2329-9096.21.8.569
Copyright: © 2020 Dash R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.