Journal of Medical Diagnostic Methods
Open Access
ISSN: 2168-9784
ISSN: 2168-9784
Review - (2020)Volume 9, Issue 1
A respiratory monitoring medical device can assist clinical providers and the medical staff with real-time data to make life-changing decisions on time. Health care providers are starting to analyze the outcomes and studies of pulmonary diseases such as Chronic Obstructive Pulmonary Disease (COPD), Congestive Heart Failure (HF) and Asthma. Monitoring the patient's respiratory health before the pulmonary disease starts to escalate should be a priority as innovation continues to grow in the healthcare arena. Wearable medical devices can reduce healthcare expenses, reduce readmission, and improve the quality of life for patients. This research paper will help further identify the gaps in adverse consequences when dealing with COPD, HF, and Asthma. Furthermore, the research will highlight populations that are at most risk and up and coming respiratory patient monitoring devices that are penetrating the healthcare space. Respiratory patient monitoring devices through telehealth can reduce healthcare costs, reduce readmission, increase clinician efficiency, and allow the physician to have a more proactive approach regarding patients' respiratory health.
Respiratory disease; Pulmonary disease; Medical device; Asthma; Chronic Obstructive Pulmonary Disease (COPD); Congestive Heart Failure (HF); Strados labs; Patient monitoring; Telehealth; Telemedicine
COPD, HF, and Asthma remain a significant economic burden in the healthcare system. As the prevalence of these diseases continues to grow the search for a solution in both the technology and healthcare industries continues to occur. They affect 1%- 3%, 4%-10%, and 8%-19% of the population, respectively, and frequently coexist [1]. COPD is becoming one of the leading reasons why Americans die, COPD, the third most common cause of death in the United States, affects nearly 14.8 million people, experts estimate [1]. As pulmonary diseases increase, there are numerous challenges to overcome. One of these barriers is the lack of access to affordable and high-quality care. The objective of this research paper is to conduct a literature review on COPD, HF, and Asthma, in addition to this, we will analyze and examine the different technologies that could be used to monitor patient respiratory health. Lastly, we will indicate potential telehealth programs that could help reduce pulmonary diseases through medical devices and technology-based platforms.
This section will introduce the background of COPD, HF, and Asthma. Also, identify populations with respiratory diseases. Chronic Obstructive Pulmonary Disease (COPD) is set to be the third commonest cause of death by 2020 globally [2]. Chronic Obstructive Pulmonary Disease (COPD) and Congestive Heart Failure (HF) are progressive disorders, and often the terminal stage of pulmonary and cardiac disease leading to death. It is estimated today that 15 million people have COPD and 6.5 million people have CHF in the US [2]. According to the World Health Organization (WHO), 14% of deaths worldwide in 2015 were caused by pulmonary diseases (specifically, Chronic Obstructive Pulmonary Disease (COPD), lower respiratory infections, and lung cancers. Pulmonary diseases such as Asthma are also a leading cause of disability [3]. The literature review will guide us in understanding how certain populations may be suffering from COPD, HF, and Asthma.
Chronic obstructive pulmonary disease background
Chronic Obstructive Pulmonary Disease is an umbrella term used to describe progressive lung diseases including emphysema, chronic bronchitis, and refractory (non-reversible) Asthma. This is a group of lung diseases that block the airway and make it difficult to breathe. COPD is often treatable but cannot be cured. Signs that show COPD can manifest as shortness of breath, tightness in the chest, coughing with or without mucus and wheezing. Triggering events include smoking, second-hand smoking, inhaling consists of bad air involving chemicals and fumes. Chronic Obstructive Pulmonary Disease (COPD) is growing in recognition as a major chronic disease and a key cause of acute medical admissions [4].
Jackie Smedley’s story stood out because of the outcome she is facing since deciding to follow her parents smoking habits at a young age. Additionally, it indicated how life has become extremely hard for her to complete daily activities. “In 2013, I have diagnosed with stage 2 COPD” [5]. “I am now on oxygen 24/7, even the simplest tasks have become a burden” [5]. Jackie’s outcome now is depending on the oxygen tank to get her through daily tasks and still live a meaningful life. The cost of her receiving oxygen and medications to treat the COPD illness can be expensive. Furthermore, if the patient’s mobility decreases then meeting these expensive demands to treat COPD will be difficult and eventually lead to death. In patients with HF, the prevalence of COPD is up to 35%, and less than 25% of patients have COPD GOLD stage III or IV [6]. COPD is more severe in patients with HF with preserved ejection fraction and when HF and COPD coexist, the hazard of death is increased by 39% but can even exceed the mortality in individual disease by threefold [6].
Heart failure background
Heart failure is a major public health problem, affecting 26 million people worldwide [7]. Patients with COPD that are consistently wheezing and having shortness of breath should be evaluated for HF. The heart fails when blood cannot pump which could slow down circulation through the body and it is common for patients to have to swallow around the legs. HF is the end stage of all diseases of the heart and is a major cause of morbidity and mortality [7]. These respiratory diseases should be monitored and controlled to prevent diseases from spreading and most importantly, escalating to death threating situations.
The Center for Diseases Control and Prevention heat map in Figure 1 shows the areas that are suffering from heart failures. The northern Texas and Oklahoma area seems to be a huge area of concern.
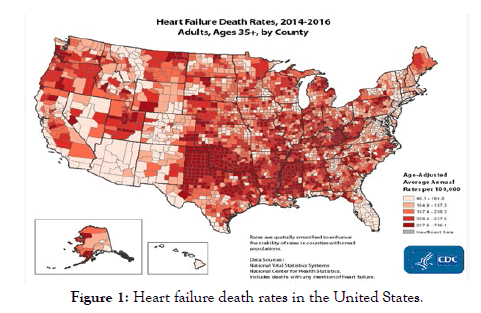
Figure 1: Heart failure death rates in the United States.
Congestive Heart Failure is the most common discharge diagnosis for Medicare beneficiaries [8]. Patients with heart failure need to track their symptoms and discuss those symptoms with a medical provider. Readmission after hospitalization for Congestive Heart Failure is common among Medicare beneficiaries, with almost half of the patients readmitted within 6 months [8]. HF cannot be cured, but early diagnosis and treatment can help people who have HF live longer and live more active lives [7].
Asthma background
Respiratory diseases continue to grow and become a critical problem for individuals. Asthma is a common diagnosis for patients. As of 2011, about twenty-three million Americans are dealing with the disease [9]. Asthma usually first appears during childhood, and it is the most common serious chronic disease among children in the United States [9]. It affects nearly seven million people under the age of eighteen [9]. Asthma has no cure, but patients can manage their condition using inhalers, generally the first line of treatment [10]. Asthma is a common chronic disorder of the airways characterized by periods of reversible airflow obstruction known as asthma episodes or attacks [11]. Asthma attacks are caused by chronically hyperactive (a contraction of the muscles surrounding the airways) and inflamed airways, leading to airflow obstruction [11]. Asthma can’t be cured but it can be controlled. A patient may notice it from having allergies, exercising or other reasons that may have the patient uncomfortable. The uncomfortable situations the patients encounter is wheezing, shortness of breath, coughing, and tightness of chest. Asthma tends to have multiple classifications that are ranging from mild intermittent to severe persistent.
The Center for Diseases Control and Prevention (CDC) estimated 39.5 million people (12.9%), including 10.5 million (14.0%) children in the United States had been diagnosed with asthma in their lifetimes (Centers for Disease Control and Prevention, 2013). An action plan with a physician needs to take place to better control this disease. In today’s world technology is being used to monitor and track Asthma symptoms so they will not escalate. The barrier of having to consistently refill the inhaler and purchasing prescribed medications can take a toll on the patient’s finances. The estimated total cost of asthma to society, including medical expenses ($50.1 billion per year), loss of productivity resulting from missed school or workdays ($3.8 billion per year) [11]. In addition to the expensive cost, it may take to keep up with Asthma, low-income households class deal with Asthma at a high rate than other income classes. Current asthma are more prevalent among adults who lived in households with an income less than $15,000 (13.3%), $15,000 to less than $25,000 (10.3%), $25,000 to less than $50,000 (8.3%), and $50,000 to less than $75,000 (8.0%) compared with adults who lived in households with an income of $75,000 or more (7.0%) [11].
Over the last 20 years, the global burden of asthma has increased by almost 30% [10]. It will be a challenge for the healthcare industry to figure out how to address these new patients who have Asthma. From a global perspective, it seems important to see what is going on in other countries around the topic of Asthma. Researchers with the Health Effects Institute, a Boston-based nonprofit that studies the health effects of pollution, recently reported that air pollution in India and China alone contributed to more than half of the four million deaths worldwide due to air pollution in 2015 [10]. A common factor that leads to Asthma seems to be centered around air pollution for individuals and the air they are inhaling daily.
Populations with respiratory disease in the US
The areas and populations in the United States of America that are suffering from COPD, Asthma and other chronic respiratory diseases are growing in numbers. Countries with the highest rates of COPD in 2014 were concentrated in central Appalachia but could also be found in other states in the southern half of the United States as far west as Colorado. Counties with the lowest rates of COPD in 2014 were found near Washington, DC; New York, New York; and San Francisco, California; along the Texas- Mexico border; in central Colorado; and in northern Utah [12]. The correlation could be linked to the condition of leaving in those states, air pollution, lack of healthcare access, resources and medication that could be available. The countries with the highest mortality rates from asthma were located along the southern half of the Mississippi River and in Georgia and South Carolina [12]. And as for other chronic respiratory diseases, Mortality rates from this group of diseases were generally highest in southern counties stretching from Mississippi to South Carolina and were also elevated in counties in northern Maine and western counties stretching from Wyoming and Utah to California and Oregon [12].
Internet of Things (IoT) and Smartphone-based continuous health monitoring devices generate a large amount of data and results in high energy expenditure [13]. Thus, exploring the power reduction technique has become the most essential to maximize the battery life of IoT and Smartphone devices [13]. In this context, the signal compression was explored to reduce the amount of data that needs to be transmitted that can significantly reduce the power consumption of wireless modules [13]. The use of ambient assisted living technology, namely technology to improve the quality of life of people at home, is becoming a common trait of modern society [14]. However, there is a lack of respiratory monitoring devices currently on the Internet of Medical Things (IOMT) industry compare to other monitoring types of diseases. Some examples of devices that are moving healthcare forward are iRyhtm-Zio Patch for heart health, Apple Watch with ECG for heart, and CGM devices for Diabetes just to name a few. The respiratory care devices’ global market is expected to grow at a high single-digit CAGR from 2019 to 2026 to reach $23,510.9 million by 2026 [15]. The need for respiratory devices is emerging and vendors in this space are aware of this necessary need to making sure they have the best device that will help the patients live a better and longer life.
Table 1 shows some of the up and coming respiratory patient monitoring devices that can advance healthcare by the functionalities they offer. Technology support clinicians on how to make proper and accurate decisions for a patient.
| Medical Devices/Functionalities | Strados Lab | Propeller Health | Cohero | In Courage |
|---|---|---|---|---|
| Wearable | X | X | ||
| System monitoring and collecting data | X | X | ||
| Mobile application friendly | X | X | X | |
| Symptom detection | X | X | ||
| Mobility | X | X | X |
Strados Labs founded in 2016. Strados Labs is making strides to help patients, suffering populations and health systems improve the patient respiratory health. Additionally, help the clinicians better monitor the patient as they try to prevent escalation and reduce the illness by monitoring them closely using a wearable biosensor. Strados Labs states, the scientific team at Strados Labs led by an MBA, MD, MD/Ph.D., clinicians and engineering advisors with over 50 years of experience. Working together, they engaged with patients and care teams to design user-friendly sensors, create collection methodologies, and develop data processing software that creates a more holistic view of a patient’s respiratory health [16]. Some of the incredible functionality this sensor has is around motion sensors, tapping sequence control, microphone array and can collect data (breathing intensity, heart rate, respiratory rate, activity level, coughing and wheezing, etc.). These diseases have been a problem for a long time and the usage of technology can help. In the hospital, wheezing accounts for approximately 25% of admissions in children rising to 50% in winter and the majority are under 5 years of age [17]. Most children who later develop chronic symptoms or atopic asthma start with discreet recurrent episodes of virus-related wheeze, which are clinically indistinguishable from lo those seen in a large number of children who stop wheezing after a few years [17]. Wheezing for most patients starts at an early age and can escalate easily if not is not monitored or treated. Cough is often regarded as a critical symptom of COPD and CHF and listening to cough is still an important mechanism for physicians to gauge disease onset and severity [2]. The sensor has an application integration component that can be used for tracking and listening on a mobile device for coughing, wheezing, etc. The rechargeable sensor is compatible with all devices and connected via Bluetooth. Lastly, the sensor can be placed comfortably on the skin of the patient or even be attached to clothing wear (tank top, straps, bra, etc.).
Strados Labs has some competitors in the space that are also trying to make their mark in the respiratory disease’s patient monitoring arena. Propeller Health is a medication management system. This device has an inhaler tracking and medication usage component but lacks objective pulmonary symptoms data (i.e. lung sounds). A study was done where patients were asked to bring the Propellor Health device in to see if they are using the correct techniques. Study findingsData from 7,558 patients, collected by Propeller Health’s digital medicine, showed that the majority of patients (84%) took less than 30 seconds between the first and second puff of their rescue or controller inhaler. Further, 67% waited less than 15 seconds between inhalations. Only 16% of patients waited more than 30 seconds between puffs, the minimum amount of time necessary to complete the recommended steps [16]. Furthermore, it was discovered that 84% of these patients are using their own inhaler incorrectly. The Propeller Health sensor is attached and paired to a patient inhaler to help manage their Asthma and COPD. The sensor provides a daily Asthma forecast along with reminders and alerts regarding their health which overall could reduce flare-ups and provide more symptoms freedays. Propellor Health has implemented a recent enhancement regarding their digital spirometer which can help patients and physicians determine the stage of the disease and how patients are responding to the treatment.
Cohero Health which is the second device that is one of Strados Labs competitor that is also focused on respiratory diseases. Cohero Health has a few products ranging from mSpirometer™ lung function sensor, BreatheSmart® App and HeroTracker® sensors. In one embodiment, the system also collects lung function data, e.g., from a spirometer, and then processes all the controller inhaler data, the rescue inhaler data, and the lung function data, to generate alerts and other messages [18]. The four products are used as a smart inhaler tracker, a monitoring system, recording real-time information and used to set reminders/alerts for medication. This helps give insights to keep the patient healthy. Also, your caregivers will be more in the loop of what is going on with your respiratory health.
The InCourage system is the third device patient can wear this system has a vest to help deliver a unique form of patient care. The InCourage system consists of a Therapy Unit (TU), an inflatable garment, and interconnecting hoses. The TU delivers pulsating air to the garment resulting in rhythmic inflation and deflation of the garment against the patient’s chest [19]. InCourage system vest is attached to the machine and creates compression to the patient’s chest that allows movement through the lungs. The mucus that generally gets stuck in the lungs is now loose, thin and able to move through the patient lungs. InCourage has been particularly useful for patients who have both COPD and bronchiectasis [19]. The InCourage system is more of a reactive approach for a congested patient.
The telehealth virtual visits market in the US is expected to reach approx. The US $813.29 million in 2021 [20]. From 2016 to 2017, by comparison with telehealth’s 53 percent growth rate, national usage of urgent care centers increased 14 percent, of retail clinics 7 percent and of ASCs 6 percent, while that of ERs decreased 2 percent [21]. Telehealth programs could enhance the importance of medical devices, connected health, and wearable biosensors. Telehealthcare is a broad term used to encompass the delivery of health-care services and information through ICT [22]. It includes clinical applications such as remote monitoring, lives videoconferencing between patients and providers, and access to specialist services such as consultation and medical imaging, as well as nonclinical services such as provider training, administrative meetings, and continuing education of health professionals using ICT services [22]. Recent studies have shown that 76 percent of U.S. patients regard to access to care as a higher priority than human interactions with their healthcare providers and that 70 percent of U.S. patients regard communicating with providers via text, email, or video rather than in person as an acceptable option [23]. In terms of respiratory care, remote monitoring, consultations, pulmonary rehabilitation (PR), pharmacy, and sleep monitoring can promote the patient-provider relationship and will each be discussed in subsequent sections [22]. This allows patients with respiratory illnesses who are in rural areas to be able to receive proper care at home. Telehealth programs can not only reduce readmissions, but it can reduce the healthcare cost for the patients. Telehealth can make receiving care convenient for the patient. All the patients need is a smartphone. That is enough for them to receive proper telehealth consultation. This allows for remote patient monitoring which is an important component for Telehealth to be activated.
From the point of activation, Figure 2 shows the cycle that the patient monitoring device will go through to transmit and communicate data electronically. Once that has been received by the medical professionals then they can now intervene when necessary to prevent escalations of the respiratory illness.
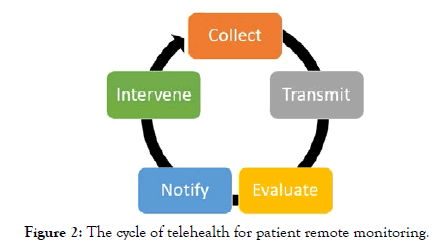
Figure 2: The cycle of telehealt h for patient remote monitoring.
As telehealth programs continue to spread worldwide and respiratory illnesses continue to grow medical devices could be leveraged in telehealth programs. The University of Pittsburgh Medical Center (UPMC) started a program to see if patients with HF will benefit from an early action prevention standpoint. It has been successful, and it is now expanding to four conditions with one of them being COPD. Medicare patients who enroll in the program are 76% less likely to be readmitted within 90 days than those who aren’t UPMC Health Plan members 65 and older who enroll are 74% less likely to be readmitted over the same time period [24]. This is a valuable method to reduce healthcare expenses and to focus more on patient health at the same time. Another growing Telemedicine program is the one developed from a school-based Asthma management program in Rochester, New York. Asthma is a common chronic disease and many children do not receive the proper care to treat which is why it can flare up and escalate to be something more serious down the road. Telemedicine is used in cities worldwide and has been used in Rochester, New York for more than 10 years, now serving all schools in the city school district with mobile telemedicine units and having performed >14,000 visits. Additionally, there is reimbursement for telemedicine visits by local payers, making it a sustainable system of care [25]. Rochester, New York school district is setting an example of how to improve respiratory health in a local community may lack access to healthcare. This is a cost-effective, efficient, and proactive way to facilitate care to children around the area.
The home base for many medical devices such as Strados Labs is Georgia. A few telehealth programs are implemented there however, more around respiratory health could be done. Becker report states, The Georgia Department of Public Health aims to deploy more than 20 additional statewide telemedicine programs within the next two years [26]. Congress Mulls and US Representative Earl Leroy Carter (Georgia) is introducing a bill The Better Respiration through Expanded Access to Tele-Health (Breathe) Act which will allow for COPD patients to be treated. This will give respiratory therapists the ability to treat Medicare patients battling COPD at their homes and rural parts of the south.
Medical devices that can work together with telehealth programs can serve as a critical role in the delivery of quality care. Technological solutions represent new opportunities to help elderly people and their caregivers in daily life. Understanding human behavior becomes thus essential in the Ambient Assisted Living field especially for prevention and monitoring applications [14]. Pulmonary and respiratory diseases comprise a large proportion of the global disease burden, responsible for both mortality and disability [3]. This burden is especially concentrated in the developing world, where air pollution levels are generally high and resources for diagnosing these diseases are very limited. It is safe to draw a correlation that air pollution could be one of the leading reasons that some areas are suffering from respiratory diseases. Improved education and monitoring of children with asthma have been shown to be highly effective in controlling symptoms and preventing failure of outpatient therapy [27]. This is an opportunity for wearable sensors and medical devices to better monitor patient illness. This would allow clinicians to analyze the data that is retrieved from these medical devices and help provide a more holistic and accurate care approach for the patients [28].
The limited studies around respiratory telehealth programs have made the correlation difficult to identify in terms of how technology can be implemented to a remote monitoring-based program. The research indicates that even though there are limited studies focused specifically around medical devices being leveraged in respiratory telehealth programs that there is a noticeable correlation between how effective medical devices can be in a rural telehealth program. Furthermore, it appears that it can enhance the overall patient respiratory health by monitoring the patient closely. The future research should consist of a deeper dive around how cost-effective medical devices in respiratory telehealth programs could be for a patient, how it could reduce readmission rates, the clinical alerts/reminders advantages in medical devices and most importantly how it can prevent respiratory illnesses such COPD, HF, and Asthma from advancing to life-threatening stages. Identifying health systems and areas that could leverage these technologies to serve patients with respiratory diseases would be a key piece for future research. Physicians will be able to understand the patient’s condition by having regular virtual updates and monitoring methodologies that will better assist the physician’s point of care.
Citation: Onwuzuruike F, Delmonico NK, Sneha S (2020) Effective Medical Device Use-Helping Clinicians Monitor Patients Respiratory Health. J Med Diagn Meth 9:288. doi: 10.35248/2168-9784.20.9.288
Received: 27-Dec-2019 Accepted: 20-Jan-2020 Published: 30-Jan-2020 , DOI: 10.35248/2168-9784.20.9.288
Copyright: © 2019 Onwuzuruike F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.