Journal of Yoga & Physical Therapy
Open Access
ISSN: 2157-7595
ISSN: 2157-7595
Research Article - (2023)Volume 13, Issue 4
Aim: To explore the effects of cognitive therapeutic exercise combined with Neuromuscular Training (NMT) on the balance and walking function of patients after anterior cruciate ligament reconstruction and to provide a theoretical basis and practical reference for rehabilitation exercise after anterior cruciate ligament reconstruction.
Methods: A total of 58 patients 6-8 weeks after anterior cross reconstruction were randomly divided into an experimental group (cognitive therapeutic exercise combined with NMT) and a control group (NMT) for 8 weeks. Standing balance and walking function were tested before and after the intervention.
Results: In the standing balance test, the total length of the elliptic X axis, elliptic Y axis, and COP track were decreased in both experimental and control groups before and after the intervention, with significant differences compared with baseline (P<0.01).
Conclusion: Both cognitive therapeutic exercises combined with NMT and NMT alone can improve the balance and walking function of patients, and mental therapeutic exercise combined with NMT is superior to NMT alone in improving the balance and walking function of patients.
Anterior cruciate ligament reconstruction; Neuromuscular training; Cognitive therapeutic exercise; Balance
Anterior Cruciate Ligament (ACL) injury is one of the common sports injuries [1]. Most ACL-injured patients undergo Anterior Cruciate Ligament Reconstruction (ACLR), which can effectively reduce secondary injuries caused by the pulling of meniscus, articular cartilage, and surrounding ligaments [2]. In the early stage after ACLR, graft maturity was insufficient, knee stability was reduced [3], and gait was still stiff 6-12 months after ACLR [4]. Changes in gait and other therapeutic strategies can reveal changes in proprioception, balance, muscle strength, and recruitment [5]. With time accumulation, intra-articular cartilage damage is accelerated, and the incidence of osteoarthritis is increased [6]. Therefore, ACL injury is considered neurophysiological dysfunction rather than a simple peripheral musculoskeletal injury [7].
Neuromuscular Training (NMT) can improve neuromuscular control of the ACLR posterior knee, enhance knee stability, reduce the risk of re-injury [8], Promote the recovery of motor ability after ACLR [9], and improve biomechanical abnormalities of the lower extremity in the ACLR [10]. Nagelli, et a [11] studied the effect of NMT on knee biomechanics during a single-leg landing mission and proved that standardized knee biomechanics and neuromuscular control were established after NMT was performed in ACLR. A further study demonstrated that NMT could significantly improve the knee biomechanics of athletes resuming exercise after ACLR [12]. Mandelbaum, et al [13] proved that NMT could continuously reduce the incidence of ACL injury in female athletes. In addition to muscle strength, pain, and proprioception, there are cognitive problems among the factors affecting the recovery after ACLR. However, the current rehabilitation training program has almost no cognitive intervention training. The cognitive part regulates the sensory and therapeutic part’s functions, enabling them to prepare and respond when the environment and tasks change [14]. Perfetti proposed cognitive therapeutic exercise to restore therapeutic function through brain function reorganization and rebuild a new cognitive therapeutic mode [15]. The process of functional recovery is a learning process, and movement is a complex form of interaction with the external environment, which depends on the integration of various cognitive functions [16]. The learning process is based on the continuous improvement of the brain’s cognitive process [17].
Based on this, this study applied cognitive therapeutic exercise combined with NMT to patients after ACLR and compared the effect of NMT alone to explore whether cognitive therapeutic exercise combined with NMT can improve the balance and gait of patients after ACLR more than NMT alone.
Participants
In this study, 58 patients aged 18-40 years after 6-8 weeks of ACLR were randomly divided into two groups: The experimental group (cognitive therapeutic exercise combined with NMT) and a control group (NMT), with 29 cases each. One case in each group fell off due to other reasons. All patients have fully understood and understood the impact of the trial and signed patient informed consent. Inclusion criteria were patients after unilateral ACLR surgery with a graft to the vastus or semitendinosus tendon of the knee. The exclusion criteria were concurrent collateral ligament and posterior cruciate ligament injury, joint dislocation, or other fractures. History of knee injuries, such as fractures, ligament strains, and osteoarthritis; combined with sensory disorders, cardiovascular and cerebrovascular diseases, and mental diseases; cognitive dysfunction. This study was approved by the Ethics Committee of Beijing Rehabilitation Hospital Affiliated to Capital Medical University (No:2021bkkf-037). The basic information of patients is shown in Table 1, and the flow chart of the experiment is shown in Figure 1.
| Criteria | Experimental table group (n=28) | Control group (n=28) | t/X2 | P |
|---|---|---|---|---|
| Gender (male/female) | 12/16 | 13/15 | 0.072 | 0.788 |
| Age (years) | 30.43 ± 7.43 | 30.23 ± 7.76 | 0.102 | 0.919 |
| Height (m) | 1.72 ± 0.08 | 1.69 ± 0.09 | 0.66 | 0.42 |
| Weight (kg) | 69.30 ± 11.10 | 68.60 ± 9.68 | 1.614 | 0.209 |
| BMI (kg/m2) | 23.40 ± 2.00 | 23.79 ± 1.94 | 1.088 | 0.281 |
| Affected side (left/right) | 13/15 | 11/17 | 0.292 | 0.589 |
Table 1: Basic information of patients (x̄ ± s).
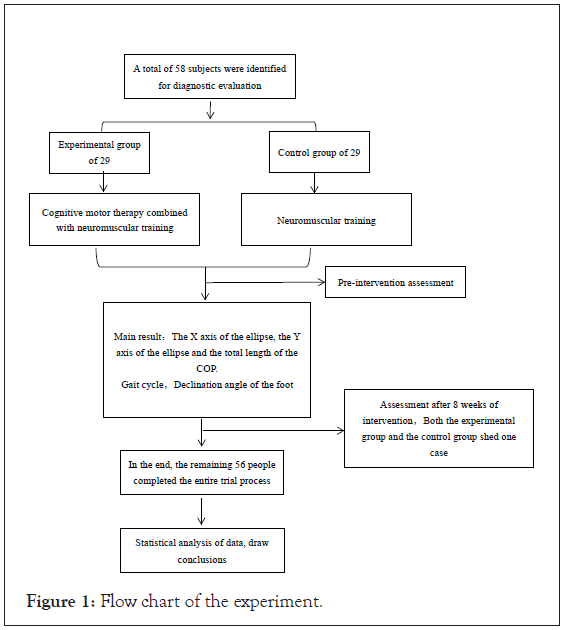
Figure 1: Flow chart of the experiment.
Positive rate of each test was calculated respectively. Chi-square tests for statistical analysis were performed using the SPSS Statistical 20.0 software (Armonk, NY, USA) [11]. A p-value inferior to 0.05 was considered that the difference is significant.
Experimental progress
In this study, patients with ACLR were randomly divided into experimental groups and control groups. The experimental group received 30 minutes of NMT followed by 15 minutes of cognitive therapeutic exercise, 5 times a week, 45 minutes each time, 40 times in total. The control group underwent NMT for 45 minutes, 5 times a week, 45 minutes each time, 40 times in total.
Neuromuscular training
The first stage (1-4 weeks of treatment): (1) Joint motion training method: The patient sat at the bedside, legs naturally drooped, a roller was placed on the sole, and the patient was asked to maximize knee flexion and extension actively. (2) Strength training: Mussel opening and closing exercise of hip abduction and external rotation under the condition of hip abduction and external rotation in the lateral decubitus position with 45° knee flexion and 90° elastic band resistance to exercise the gluteus maximus gluteus medius; supine glute bridge exercises to work the core and glutes; Leg lift training: Performed in a leg lift trainer, the amount of resistance is determined by the range that the patient can tolerate. (3) Weight training and center of gravity transfer: Unilateral weight training, starting from 50% of body weight under patient tolerance, until standing on one leg for more than 30 seconds; Forward and backward weight transfer training: The affected side has weight transfer in the front and rear front and rear feet standing position.
The second stage (5-8 weeks of treatment): (1) Strength training: Hip joint abduction and extension training under the condition of resistance with a standing elastic band; Sitting resistance extension knee training, resistance size to the patient can bear the range of decision; (2) Walking training: Obstacle walking training.
Cognitive therapeutic exercise
All patients were selected first passive movement, 3 consecutive no- error answers after the active movement, 3 times no error after the next task, the task is divided into: In different flexion of the hip, knee, and ankle plantar flexion angle in the heel, popliteal fossa and toe to identify the different hardness of cotton block; Identify different positions on the grid when the heel is in contact with the bed surface and standing on one leg; Identify the different angles of ankle plantar flexion and dorsiflexion when standing at different knee and hip flexion angles.
Data collection
The instrument adopts Zebris (Germany) gait analysis platform and FDM-System system to measure the biomechanical characteristics of the plantar while standing. Balance function measurement: center of gravity moving track total length. The walking function was measured, including gait cycle and foot deflection angle.
Statistical analysis
SPSS 20.0 software was used for data analysis, and the data were in line with normal distribution. Mean standard deviation (mean ± SD) was used for data representation, chi-square test was used for counting data, the independent sample t-test was used for the comparison of measurement data between two groups, and paired sample t-test was used for intra-group comparison. The difference significance criterion was P<0.05 was a significant difference, P<0.01 was a very significant difference.
Balance
At baseline, there was no significant difference between the two groups in the elliptic X axis, elliptic Y axis, and COP track total length (P>0.05); the values of the three indexes were all decreased after the intervention. The reduction was more evident in the experimental group, and there was a very significant difference between the two groups (P<0.01). The total length of the elliptic X axis, elliptic Y axis, and COP track in the experimental group decreased significantly compared with baseline (P<0.01), the total length of elliptic X axis, elliptic Y axis and COP track were decreased in control group, and there were significant differences compared with baseline (P<0.01). The relevant results are shown in Figures 2-4.
Figure 2: COP track. Note: (EG) Experimental group; (CG) Control group. (##) comparison between the two groups; (**) Intra-group comparison.
Figure 3: Total length of elliptic X axis. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra- group comparison.
Figure 4: Total length of elliptic Y axis. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Gait cycle
At baseline, there was no significant difference in the percentage of the support phase, and swing phase between the two groups (P>0.05), the percentage of the support phase increased, and the percentage of the swing phase decreased after the intervention, especially in the experimental group, and there was a very significant difference between the two groups (P<0.01). The percentage of the support phase increased, and the percentage of the swing phase decreased in experimental groups, showing significant differences compared with baseline (P<0.01). The percentage of the support phase increased and the percentage of the swing phase decreased in the control group, and there were significant differences compared with baseline (P<0.01). The relevant results are shown in Figures 5 and 6.
Figure 5: Graph showing percentage of Support phase. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Figure 6: Graph showing percentage of Swing phase. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
There was no significant difference between the two groups at baseline (P>0.05). The percentage of single and double supported phases on the affected side increased after intervention, while the percentage of single supported phase on the healthy side decreased, especially in the experimental group, and there was a very significant difference between the two groups (P<0.01). The percentage of single and double supported phase on the affected side increased, while the percentage of single supported phase on the healthy side decreased, showing significant differences compared with baseline (P<0.01). The percentages of single and double supported phases increased on the affected side and decreased on the healthy side of the control group, showing significant differences compared with baseline (P<0.01). The relevant results are shown in Figures 7-9.
Figure 7: Affected side single supported phase. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Figure 8: Healthy side single supported phase. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Figure 9: Double supported phases. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra- group comparison.
Foot deflection angle
At baseline, there was no significant difference in foot deflection between the two groups (P>0.05). Both the healthy side and the affected side foot decreased after the intervention, but there was no significant difference between the experimental group and the control group (P>0.05), there was a significant difference in the reduction of the affected side foot angle in the experimental group (P<0.05). The declination of the healthy and affected foot decreased in both groups, showing significant differences from baseline (P<0.01). Both the healthy side and the affected side of the foot decreased in the control group, and there were significant differences compared with baseline (P<0.01). The relevant results are shown in Figures 10 and 11.
Figure 10: Declination angle of the healthy side. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Figure 11: Declination angle of the affect side. Note: (EG) Experimental group; (CG) Control group; (##) comparison between the two groups; (**) Intra-group comparison.
Balance
Human static standing balance usually selects the moving track of indicator COP to objectively reflect human balance ability according to the length and speed of the COP shaking track [18]. Some studies found that after ACLR, the total length of the COP moving track and the length of the elliptic X-axis increased compared with normal people, and the difference was statistically significant [19]. This indicated that after ACLR, the patient had increased shaking and decreased balance when standing. Another scholar studied the balance function of patients after ACLR compared with healthy adults [20]. Comparing the stress center under the balance task of standing on one leg and standing on two legs while performing cognitive tasks, the results also showed that patients after ACLR sacrificed balance to optimize the cognitive function performance. The total length of elliptic X axis, elliptic Y axis and COP track in the static plantar pressure center movement trajectory of the experimental group and the control group were reduced before and after the intervention. The reduction in the experimental group was more evident than that in the control group, and there was a very significant difference between the two groups. Compared with conventional NMT alone, cognitive therapeutic exercise combined with NMT not only trains the muscle strength and range of motion of therapeutic control, but also focuses on cognitive training, especially the perception of joint position. Patient perception is improved by moving several joints simultaneously to increase complexity and difficulty.
Gait cycle
This study studied the effects of cognitive therapeutic exercise combined with NMT on the gait cycle after ACLR. It was found that the affected side support phase was prolonged, and the swing phase was decreased in both the experimental group and the control group compared with baseline. The single and double supported phases on the affected side lengthened, while the single supported phase on the healthy side decreased. The results showed that both NMT and cognitive therapeutic exercise combined with NMT improved the percentage of gait cycles after ACLR. Lin [21] found that increasing knee extensor muscle strength could improve gait biomechanics; black burn [22] found that improving proprioception could restore gait biomechanics and reduce the risk of osteoarthritis; NMT in the experimental group and the control group improved walking function by increasing muscle strength and proprioception.
Foot deflection angle
Foot deflection refers to the angle between footprints and the direction of travel during walking. Studies have shown that there is no significant difference in foot deflection angle before the age of 60 [23]. The variation of foot deflection is related to the health condition of human lower limbs. Femoral neck torsion, knee osteoarthritis and plantar diseases will affect the direction and size of foot deflection [24]. In this study, the influence of cognitive therapeutic exercise combined with NMT on the foot deflection of the healthy posterior side and the affected side of ACLR was studied. It was found that the foot deflection of the experimental group and the control group was reduced compared with baseline, indicating that NMT and cognitive therapeutic exercise combined with NMT could improve the foot deflection of the posterior healthy side and the affected side after ACLR. Compared with the control group, the experimental group had no significant difference in improving the healthy side foot angle, but had significant improvement in the affected side. There was no difference between the experimental group and the control group in the healthy side foot deflection angle, which may be related to the intervention time. It may also be that cognitive therapeutic exercise in this study focused more on the ankle sagittal plane training and less on the joint position awareness training on the horizontal plane.
Cognitive therapeutic exercise combined with NMT and NMT alone can improve a patient's balance function, gait cycle and foot deflection in walking function. In addition, cognitive therapeutic exercise combined with NMT is superior to NMT alone in improving patient’s balance function and walking function, which is suggested to be added to the rehabilitation training after ACLR in the future. Cognitive therapeutic exercise combined with NMT is easy to use, and patient participation is recommended to continue to be widely used in other diseases.
Thanks to all authors for their hard work on this study. Thanks for the financial support provided by Beijing Rehabilitation Hospital Affiliated to Capital Medical University.
This research was funded by the 2021-2023 Special Science and Technology Development Project of Beijing Rehabilitation Hospital, Capital Medical University (#2021-003) and Undergraduate Research Innovation project of Capital Medical University (#XSKY2022372).
Data available on request due to ethical restrictions. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
ZJ, WC and MY designed the study. ZJ and JL instructed participants to exercise and acquired and collected the data. ZJ, WC and JL performed the statistical analysis. ZJ and WC wrote the first draft of the manuscript. ZL and MY wrote sections of the manuscript. MY critically reviewed and revised the manuscript. All authors contributed to this article and approved the submitted version.
All the authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The present study results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
The clinical trial protocol was reviewed and approved by the Clinical Research Ethics Committee of Beijing Rehabilitation Hospital, Capital Medical University (#2021bkky-037). The patients/participants provided their written informed consent to participate in this study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ma Y, Zhu J, Wang C, Jin L, Fan Z, Wang Y, et al. (2023) Effects of Cognitive Therapeutic Exercise Combined with Neuromuscular Training on Balance and Walking Function after Anterior Cruciate Ligament Reconstruction. J Yoga Phys Ther.13:397.
Received: 07-Apr-2023, Manuscript No. JYPT-23-23347; Editor assigned: 10-Apr-2023, Pre QC No. JYPT-23-23347 (PQ); Reviewed: 24-Apr-2023, QC No. JYPT-23-23347; Revised: 01-May-2023, Manuscript No. JYPT-23-23347 (R); Published: 08-May-2023 , DOI: 10.35248/2157-7595.23.13.397
Copyright: © 2023 Ma Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.