
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2024)Volume 14, Issue 1
Aim: The aim of this study was to investigate the safety and feasibility of the High-Frequency Oscillatory Ventilation (HFOV) technique for the management of thoracoabdominal malignancies in patients undergoing heavy ion therapy.
Methods: A retrospective analysis of clinical data from 20 patients with thoracoabdominal malignant tumors treated with heavy ion therapy under the control of high-frequency oscillatory ventilation at Gansu Province Wuwei Cancer Hospital was conducted from January 2023 to July 2023. Patient's general conditions, respiratory motion, and other indicators were analyzed and compared before, during, and after the treatment to determine the value of utilizing high-frequency oscillatory ventilation for managing thoracoabdominal malignancies in patients undergoing heavy ion therapy.
Results: Primary or secondary lung malignancies were the most common, followed by pancreatic malignancies. There was no significant difference in heart rate, blood pressure, blood oxygen saturation, or tcpCO2 values before, during, or after treatment (P>0.05). High-frequency oscillatory ventilation improved the patient's tcpO2 values (P=0.000). The lung respiratory motion under high-frequency oscillatory ventilation was 1.42 ± 0.41 mm, which was significantly lower than that in the autonomous respiration state (P=0.000), and there were no occurrences of "missed targeting" during radiotherapy. During the treatment process, one case each of hypertension and hypercapnia was observed, and two patients experienced nausea and vomiting after extubation. Follow-up examinations of all 20 patients revealed no cases of radiation pneumonitis, and repeat CT scans indicated a partial response in all cases, with an average hospitalization time of 25.40 ± 11.05 days.
Conclusion: High-frequency oscillatory ventilation enables thoracoabdominal tumor patients to receive higher doses of precise heavy ion therapy, thereby enhancing treatment efficacy. This approach is safe, causes fewer complications, and reduces hospitalization time.
High-frequency oscillation ventilation; Breathing control; Heavy ions; Precision radiotherapy; Thoracic and abdominal tumors
The incidence of tumors is increasing annually, seriously affecting human health. Surgery and radiotherapy are important treatment modalities for malignant tumors, with approximately 70% of cancer treatment regimens involving radiation therapy. The principle behind radiation therapy is to reduce the size of the tumor area by disrupting cell division through radiation. However, during radiotherapy, it is also possible to affect healthy cells [1,2].
Heavy ion therapy is currently the most advanced technology for tumor radiation therapy. Heavy ion beams are high-LET radiation that benefit physical dose distribution (Bragg peak). There is a minimal risk of exposure to organs located beyond the range endpoint, high biological efficacy in the peak region, and significant therapeutic effects have been achieved in the clinical treatment of tumors thus far [3]. However, the location of thoracoabdominal tumors changes with respiratory motion during treatment, posing a challenge as respiratory motion can cause deviations in the position of the radiation therapy target relative to the accelerator's static irradiation field [1,2]. Respiratory motion is one of the important factors affecting the efficacy of "precision radiation therapy" for thoracic tumors. The relative position between the scatter beam and the target area changes as a result of motion during irradiation, leading to inconsistencies between the actual dose received by the patient and the planned dose [4,5]. This seriously affects the precision of heavy ion radiation therapy for tumor sites and results in unnecessary damage to healthy tissues. Therefore, there is an urgent clinical need for a safe and effective means of controlling respiratory motion during heavy ion therapy.
High-frequency oscillatory ventilation is currently the most advanced high-frequency ventilation technique. It is characterized by a high frequency, small tidal volume, and high mean airway pressure and limits patient's respiratory movements during ventilation [6,7]. We pioneered the application of high-frequency oscillatory ventilation in the treatment of thoracoabdominal tumors subjected to heavy ion therapy. This technology was first introduced in Switzerland and has not been widely used domestically. Preliminary tests involving healthcare professionals and volunteers have demonstrated the safety of high-frequency oscillatory ventilation. Currently, this technology has been successfully applied in the treatment of 20 cases. We retrospectively analyzed the clinical data of these 20 patients and summarized and discussed the value of high-frequency oscillatory ventilation technology in heavy ion therapy, providing insights and references for precision radiation therapy.
General information
High-Frequency Oscillatory Ventilation (HFOV) is a technique used to control the movement of thoracoabdominal organs in patients under deep sedation and adequate muscle relaxation using a high-frequency oscillatory ventilator. Clinical data were retrospectively analyzed for 20 patients with thoracoabdominal malignant tumors who underwent HFOV-controlled heavy ion therapy at Gansu Province Wuwei Cancer Hospital from January 2023 to July 2023. All 20 patients had been previously diagnosed with malignant tumors at other hospitals and had undergone systemic antitumor treatment. Among them, 14 were male and 6 were female, with a median age of 63 years (range: 39-81 years). Patients were generally in good condition, had no contraindications to radiation therapy, and had no current history of severe pulmonary and cardiac dysfunction, severe hypertension, cardiac arrhythmias, refractory hypotension, passive dependence on pulmonary blood flow, acute exacerbation of respiratory and circulatory diseases, or allergies to analgesics or sedatives.
Instruments and equipment
• High-frequency oscillatory ventilator (CareFusion 3100B HFOV, California, USA).
• TCM Combi M transcutaneous oxygen/carbon dioxide tension monitoring device.
• Bedside electrocardiogram monitor.
• Bispectral Index (BIS) monitor.
• Train-of-Four (TOF) neuromuscular stimulator.
Treatment procedure
After obtaining informed consent, patients were deeply sedated (with etomidate and sufentanil) and adequately paralyzed (with rocuronium bromide). Following cessation of spontaneous breathing, tracheal intubation was performed, and 4-D CT positioning was conducted under HFOV control. The initial settings for the HFOV machine were as follows: frequency 480-600 cycles per minute (8 Hz-10 Hz), mean airway pressure (Paw) 10 cm H2O, amplitude 6 cm, tidal volume (Vt) 62.5 ml (determined by amplitude and frequency), inspiratory time 30%, fraction of inspired oxygen (FiO2) 40%, and bias flow 30 L/ min. This ensured adequate airway pressure, oxygen saturation, tidal volume, oxygen partial pressure, and carbon dioxide partial pressure. After positioning, patients were transferred to the Intensive Care Unit (ICU) for assisted ventilation with a conventional ventilator while awaiting target area delineation. After target area delineation, patients were transported to the heavy ion therapy room for heavy ion therapy under HFOV control. Following completion of heavy ion therapy, patients were transferred back to the ICU, awakened, extubated upon restoration of spontaneous breathing, and then sent to a general ward. Remazolam was given deep sedation between the end of localization and the end of heavy ion therapy. Throughout the procedure, noninvasive blood gas analysis was used to monitor PO2 and PCO2 levels, the Bispectral Index (BIS) modified observer’s assessment of alert (MOAA/S) Ramsay score and Richmond Agitation and Sedation Scale (RASS) were used to monitor the level of sedation to ensure patient comfort and safety.
Evaluation criteria
The patients' heart rate (P), blood pressure (mean arterial pressure, MAP), oxygen saturation (SO2), transcutaneous oxygen tension (tcpO2), transcutaneous carbon dioxide tension (tcpCO2), diaphragm movement, subjective feelings during the 2 hours-48 hour post- treatment period, and general condition were monitored. Late-phase side effects and efficacy were also assessed.
Statistical analysis
All statistical analyses were performed using SPSS version 26.0. Normally distributed data are presented as the mean ± standard deviation, and non-normally distributed data are presented as the median (range). Student's t test was used for normally distributed data, and the Mann‒ Whitney U test was used for non-normally distributed data. A significance level of P<0.05 was considered statistically significant.
General clinical data
Among the 20 patients, 9 had secondary lung malignancies, 4 had primary lung malignancies, 5 had pancreatic malignancies, 1 had intrahepatic bile duct malignancy, and 1 had breast malignancy. Thirteen radiation sites were located in the lungs, 5 in the pancreas, 1 in the intrahepatic bile duct, and 1 in the breast, as detailed in Table 1. Primary and secondary lung tumors often presented with multiple lesions, with one patient having 11 metastatic lesions in the left lung. Treatment was completed in a single session for patients with multiple lesions, as illustrated in Figure 1.
| No. | Diagnosis | Site of the radiation |
|---|---|---|
| 1 | Malignant tumor of the liver secondary malignant tumor of the lung | Left lung |
| 2 | Malignant tumor of the colon secondary malignant tumor of the lung | Left lung |
| 3 | Malignant tumor of the liver secondary malignant tumor of the lung | Right lung |
| 4 | Malignant tumor of the lung | Left lung |
| 5 | Rectocolonic malignancy Secondary malignant tumor of the lung |
Left lung |
| 6 | Pancreatic malignancy | Pancreas |
| 7 | Pancreatic malignancy | Pancreas |
| 8 | Pancreatic malignancy | Pancreas |
| 9 | Intrahepatic bile duct malignancy | Intrahepatic bile duct |
| 10 | Pancreatic malignancy | Pancreas |
| 11 | Gastric malignancy Secondary malignant tumor of the lung |
Left lung |
| 12 | Breast malignancy | Right mammary gland |
| 13 | Lung malignancy tumor | Right lung |
| 14 | Bile duct malignancy secondary malignant tumor of the lung | Right lung |
| 15 | Malignant tumor of the lung | Right lung |
| 16 | Malignant tumor of the colon Secondary malignant tumor of the lung |
Left lung |
| 17 | Malignant tumor of the lung | Left lung |
| 18 | Cervical malignancy Secondary malignant tumor of the lung |
Right lung |
| 19 | Pancreatic malignancy | Pancreas |
| 20 | Malignant tumor of the liver Secondary malignant tumor of the lung |
Left lung |
Table 1: Characteristics of patients.
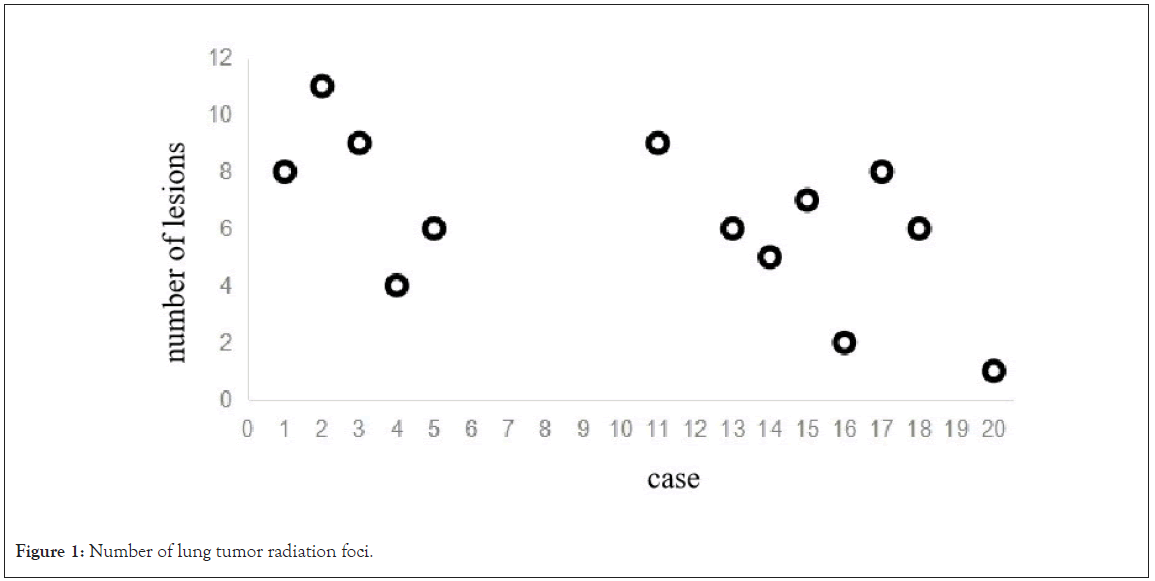
Figure 1: Number of lung tumor radiation foci.
Analysis of monitoring parameters during the treatment period
Analysis of monitoring parameters during the treatment period indicated that there was no statistically significant difference (P>0.05) in heart rate, blood pressure, or blood oxygen saturation before, during, or after treatment. Additionally, there was no statistically significant difference (P>0.05) in tcpCO2 values before, during or after treatment. However, tcpO2 values during treatment were significantly higher than those before and after treatment (P<0.001), as detailed in Table 2.
| Parameters | Baseline | After Intubation | Location 10 min | Location 30 min | Target volume delineation | 10 mins after heavy ion therapy | 30 mins After heavy ion therapy | After extubation | P value |
|---|---|---|---|---|---|---|---|---|---|
| P(次/分) | 77.00 ± 10.10 | 75.30 ± 9.16 | 75.15 ± 8.07 | 76.60 ± 7.46 | 77.15 ± 8.49 | 76.15 ± 10.03 | 77.80 ± 8.99 | 76.55 ± 8.26 | 0.983 |
| MAP(mmHg) | 80.75 ± 9.51 | 80.60 ± 9.33 | 80.60 ± 9.13 | 80.75 ± 9.51 | 81.60 ± 7.51 | 82.10 ± 10.37 | 82.55 ± 7.97 | 81.05 ± 7.06 | 0.994 |
| SO2(%) | 96.35 ± 1.69 | 96.65 ± 1.53 | 97.35 ± 2.91 | 97.15 ± 2.74 | 96.55 ± 1.47 | 96.75 ± 1.55 | 96.75 ± 1.68 | 96.45 ± 1.57 | 0.752 |
| tcpO2(mmHg) | 88.90 ± 5.88 | 97.65 ± 3.53*# | 97.55 ± 3.75*# | 96.55 ± 4.43*# | 96.20 ± 4.70*# | 97.05 ± 5.51*# | 96.95 ± 3.68*# | 92.65 ± 5.51 | 0 |
| tcpCO2(mmHg) | 44.10 ± 4.18 | 45.15 ± 2.94 | 44.85 ± 2.87 | 45.95 ± 3.44 | 45.60 ± 3.62 | 46.25 ± 5.29 | 47.15 ± 8.57 | 43.80 ± 5.01 | 0.379 |
Note: Compared with baseline, *P<0.05; compared with extubation, #P<0.05.
Table 2: Parameters during treatment.
Comparison of patient respiratory motion
All 20 patients underwent 4-D CT scans in both spontaneous breathing and respiratory control states. Lung respiratory motion was assessed at the most pronounced respiratory activity site in both states. It was observed that during respiratory control, lung respiratory motion was 1.42 ± 0.41 mm, which was significantly lower than that during spontaneous breathing (P<0.001), as depicted in Table 3. There was no "off-target" movement during radiation therapy in the 20 patients.
| Diaphragm movement during spontaneous breath (mm) | Diaphragm movement during HFOV(mm) | P值 |
|---|---|---|
| 19.02.42 ± 4.84 | 1.42 ± 0.41 | 0.000 |
Table 3: Diaphragm movement during spontaneous breathing and HFOV.
Side effects during and after heavy ion therapy under high- frequency oscillatory ventilation control
During the treatment process of the 20 patients, one patient experienced hypertension, which was successfully managed with medication to normalize blood pressure. Another patient developed hypercapnia; however, this was primarily influenced by oscillation amplitude and frequency. After adjusting the parameters of the high- frequency oscillatory ventilator (increasing amplitude and decreasing frequency to increase tidal volume), the carbon dioxide partial pressure gradually returned to normal. Two patients experienced nausea and vomiting after extubation, likely due to insufficient fasting time before treatment or the effects of analgesics and sedatives. Symptomatic treatment was administered and led to improvement.
Follow-up of all 20 patients revealed no cases of radiation pneumonitis, and reexamination by CT scans indicated that Partial Remission (PR) was achieved in all cases. The average length of hospital stay was 25.40 ± 11.05 days. For patients with pancreatic malignancies and intrahepatic bile duct malignancies, routine heavy ion therapy was followed by additional high-frequency oscillatory ventilation-controlled heavy ion therapy, which resulted in longer hospital stays.
Respiratory motion is a major factor affecting the positioning of thoracoabdominal tumors during radiation therapy. The relationship between tumor motion and respiratory motion is closely intertwined, with their cycles and amplitudes being fundamentally synchronized. Therefore, in the absence of other interfering factors, tumor motion can be attributed mainly to respiratory motion [8]. Due to the influence of motion on the diaphragm during respiration, tumors located in the lower lung and upper abdomen are more prone to moving "off-target", with research suggesting that tumors can move up to 50 mm off target [9]. Such off-target movement can result in under dosing of the target area and overdosing of normal tissues, significantly impacting treatment efficacy and prognosis.
Previous studies have shown that the displacement of the geometric center of the target area due to respiratory motion in the left-right, anterior-posterior, and cranio-caudal directions is 0.34 ± 0.21, 0.21 ± 0.27, and 0.84 ± 0.42 cm, respectively [10,11]. These studies collectively highlight the significance of organ movement caused by respiratory motion, especially of thoracoabdominal tumors. The impact of respiratory motion during tumor radiotherapy cannot be underestimated, and precise radiation therapy can only be achieved by minimizing the effects of respiratory motion.
Therefore, numerous researchers have explored methods to mitigate the impact of tumor movement due to respiratory motion. The methods for reducing the influence of respiratory motion can be broadly categorized into five groups: motion-encompassing techniques, breath- holding techniques, forced shallow breathing techniques, respiratory gating techniques, and real-time motion tracking techniques, each with its own advantages and disadvantages.
To control respiratory motion during heavy ion therapy, we introduced high-frequency oscillatory ventilation technology from abroad and combined it with heavy ion therapy. This pioneering approach was applied to the treatment of thoracoabdominal tumors. Analysis of the data from 20 patients showed that most of the patients had primary or secondary lung malignancies, followed by pancreatic malignancies (Table 1). All patients had undergone systemic antitumor treatment at external facilities. Multiple lung tumors were irradiated simultaneously in a single session (Figure 1), while other thoracoabdominal tumors received conventional heavy ion therapy followed by localized consolidation irradiation.
Heart rate, blood pressure, blood oxygen saturation, and tcpCO2 values showed no significant differences before, during, and after treatment (Table 2). However, high-frequency oscillatory ventilation significantly increased tcpO2 values during treatment (P<0.001) (Table 2). Respiratory motion under high-frequency oscillatory ventilation was 1.42 ± 0.41 mm, which was significantly less than that during spontaneous breathing (P<0.001) (Figure 2 and Table 3), and there was no "off-target" movement during radiation therapy.
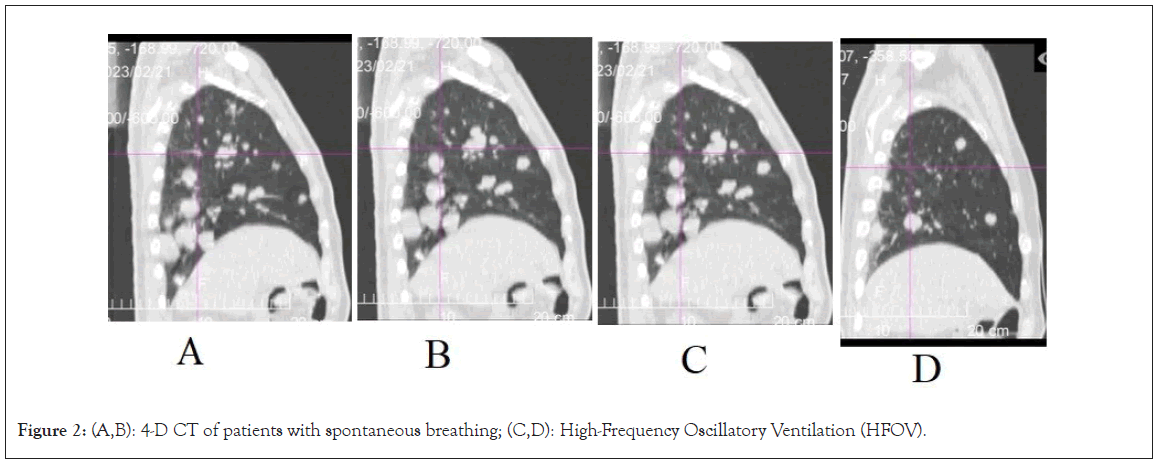
Figure 2: (A,B): 4-D CT of patients with spontaneous breathing; (C,D): High-Frequency Oscillatory Ventilation (HFOV).
During the treatment process, one patient experienced hypertension, while another developed hypercapnia. For the latter, carbon dioxide elimination was primarily influenced by oscillation amplitude and frequency. Adjusting the parameters of the high-frequency oscillatory ventilator (increasing amplitude and decreasing frequency to increase tidal volume) gradually normalized the carbon dioxide partial pressure. After extubation, two patients experienced nausea and vomiting, likely due to insufficient fasting time before treatment or the effects of analgesics and sedatives. Symptomatic treatment led to improvement.
High-frequency oscillatory ventilation technology, when applied to thoracoabdominal tumor heavy ion therapy, is safe and precise. It allows precise tumor targeting, even during heavy ion therapy and high-dose irradiation of tumors, while minimizing irradiation of normal tissues and ensuring patient comfort and safety. Moreover, it allows for simultaneous irradiation of multiple lesions in a single session, thereby reducing the patients’ hospitalization duration and economic burden. This approach enhances the patients' and their families' understanding of the disease, promotes better recovery, and facilitates the patients' return to society.
The heavy ion therapy has two major advantages compared to traditional photon therapy. One is the advantage of the Bragg peak physics, and the other is the relative radiation biological effect. The Bragg peak's occurrence in the depth of the biological body is highly sensitive to the entry of carbon ions, meaning that once a certain amount of carbon ion energy enters the body, the location where the Bragg peak occurs remains fixed at a specific depth. Therefore, when the tumor's position shifts due to respiratory movement, it can cause an accumulation of radiation dose from carbon ions at the wrong location, leading to a dual loss in treatment-where the treatment fails to reach the intended area while causing harmful radiation dose to unintended areas. Hence, the use of high-frequency oscillatory breathing control in carbon ion therapy for areas with high relative radiation biological effects achieves the requirement for high precision, efficiency, and dose accumulation at the tumor site.
In summary, the use of high-frequency oscillatory breathing control in thoracic and abdominal tumor heavy ion therapy ensures high safety. This technology enables patients to receive precise heavy ion treatment with accurate positioning, high tumor dosage, minimal exposure to normal tissues, increased comfort, and high safety. However, our current study has only involved 20 cases, which presents a limited sample size. Therefore, the results have certain constraints, and more questions and solutions need exploration and summarization in future treatments.
This study was conducted in accordance with ethical guidelines, the study protocol was approved by the Wuwei Tumor Hospital Medical Ethics Committee (2023-31).All participants provided informed consent to participate in this study.
Consent for publication have be obtained from every participate.
Data are not publicly available due to its sensitive nature (including protected health information of participants.) De-identified data may be made available upon reasonable request to the corresponding author for the purposes of replication of study results.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
No funding
Conception and design: YW, YZW, WXZ, YSZ. Collection and assembly of data: YW, YZW, WXZ, YTT. Data analysis and interpretation: YW, YZW, WXZ, YTT, FW. Manuscript writing: All authors. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Wang Y, Zhao W, Tang Y, Wang F, Ye Y, Zhang Y, et al (2024) Effects of High-Frequency Oscillatory Ventilation on the Management of Thoracoabdominal Tumors during Heavy Ion Therapy J Clin Trials. 14:547.
Received: 10-Jan-2024, Manuscript No. JCTR-24-29116; Editor assigned: 12-Jan-2024, Pre QC No. JCTR-24-29116(PQ); Reviewed: 26-Jan-2024, QC No. JCTR-24-29116; Revised: 02-Feb-2024, Manuscript No. JCTR-24-29116(R); Published: 09-Feb-2024 , DOI: 10.35248/2167-0870.24.14.547
Copyright: © 2024 Wang Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.