Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Research Article - (2023)Volume 13, Issue 4
Background: Aortic dissection patients entering the hospital may suffer from chest pain and have a deviation value of lipoprotein (a) (Lp (a)). In the present study, we aimed to investigate the clinical importance of Lp (a) level among Aortic Dissection (AD) patients, healthy control.
Method: Fifty patients with acute Aortic Dissection (AD) and fifty healthy subjects were recruited in our current study. The baseline parameters of AD patients and control group were recorded, and the data were compared between the two groups. Receiver Operating Characteristic curve (ROC) was performed to assess the diagnostic ability of Lp (a), neutrophil/lymphocyte, CRP for the incidence of AD.
Results: The level of Lp (a), neutrophil/lymphocyte, CRP in AD was significantly higher than in the control group (P<0.05). ROC curve analysis showed that neutrophil, Lp (a), and neutrophil-lymphocyte ratio can distinguish AD patients from the control group.
Conclusions: This study indicates that Lp (a) can be evaluated as useful parameters in the emergency clinical approach in the evaluation of risk of acute aortic dissection. Future larger sample studies are required to confirm the results and address the role of these parameters in determining the severity of aortic dissection.
Aortic dissection; Aneurysm; Inflammation; Lipoprotein (a); Pulsatile blood flow
Aortic Dissection (AD) is a tear in the aortic wall layers and pulsatile blood flowing into the medial layer [1,2]. AD is a lifethreatening disease with a prevalence of about 6 cases per 100000 person years in a large population [3]. The accidence rate of aortic dissection is estimated to rise due to circadian and seasonal variation [4,5]. In addition, multiple risk factors were involved in AD development, including hypertension [6], male gender, and an average age of around 70 [7]. However, it is still challenging to identify the associated risk factors that underlie the pathophysiology of AD.
Lipoprotein (a) is a cholesterol rich lipoprotein consisting of Low Density Lipoprotein C (LDL-C), Apolipoprotein (a) (Apo (a)) and Oxidized Phospholipids (OxPL) [8]. Several types of research demonstrated that the effect of Lp (a) accounts for atherosclerosis, thrombosis, and pro-inflammatory mechanism. The lipoprotein (a) contributed to the development of coronary artery disease, stroke, and peripheral artery disease. The lipoprotein (a) serum level thus was implicated as an indicator of atherosclerosis. Moreover, Lp (a) caused thrombosis by inhibiting fibrinolysis and procoagulant effect, similar to plasminogen [9-11]. Moreover, a cross-sectional study on Aortic Stenosis (AS) patients revealed that Lp (a) mediates AS progression through its associated OxPL [12]. The accumulating literature drew out the controversial conclusion about the association between the plasma Lp (a) level and the incidence of AD. A population based study revealed no significant differences in lipoprotein (a) serum levels between AD patients and the control group [13]. However, our previous study concluded the reverse conclusion that patients with had significantly higher Lp (a) group compared to healthy individuals [14]. In the present study, we aimed to investigate the clinical importance of Lp (a) level among Aortic Dissection (AD) patients, and healthy control. In our study, when patients entered hospital, the neutrophil, Lp (a), neutrophil-lymphocyte ratio, platelet, monocyte, and etc. were recorded. Furthermore, our group try to explore the importance of high sensitivity for AD patients. In some ways, identifying AD patient’s earlier can save more time and rescue patients effectively.
Study population
From January 2013 to January 2019, 50 AAD patients diagnosed by clinical features and contrast-enhanced CT in Taizhou hospital within one week after the onset of AAD symptoms, and admitted in the current study.
The exclusion criteria were as follows:
• Patients with hereditary defects of connective tissue, like Marfan’s syndrome.
• Patients who had central nervous system diseases.
• Severe illnesses such as surgical operation. Meanwhile, 50 healthy controls in Taizhou hospital enrolled for comparison.
The ethics committee approved the study of the Taizhou hospital of Wenzhou medical university. After a detailed description of the research, the informed consent signed by patients or their relatives in case patients had difficulty in writing due to limb paralysis-moreover (Tables 1 and 2).
| AD group (n=50) | Normal group (n=50) | p | |
|---|---|---|---|
| Sex, N (%) | 35 (100) | 41 (82) | 0.188 |
| Age | 62.1 ± 14.6 | 50.8 ± 8.4 | / |
| SBP | 151.8 ± 29.1 | 131 ± 14.3 | P<0.05 |
| DBP | 86.4 ± 17.4 | 78.1 ± 9.8 | p<0.05 |
| Smoking | 18 (36) | 14 (28) | p<0.05 |
| Drinking | 11 (22) | 6 (12) | p<0.05 |
| Hypertension | 39 (78) | 8 (16) | p<0.05 |
| Diabetes | 5 (10) | 1 (2) | p<0.05 |
| Stroke | 4 (8) | 0 | p<0.05 |
| Artery diseases | 1 (2) | 0 | p<0.05 |
| COPD | 4 (8) | 0 | p<0.05 |
| BUN | 8.2 ± 6.2 | 5.4 ± 1.2 | p<0.05 |
| Scr (μmol) | 137.4 ± 216.2 | 74.9 ± 15.5 | p<0.05 |
| TG (mmol) | 1.2 ± 0.6 | 1.8 ± 1 | p<0.05 |
| TC (mmol) | 4.1 ± 0.9 | 4.4 ± 0.8 | p<0.05 |
| HDL-C (mmol) | 1.2 ± 0.2 | 1.3 ± 0.6 | 0.22 |
| LDL-C (mmol) | 2.3 ± 0.8 | 2.5 ± 0.6 | 0.09 |
| Apo-A1 | 1.2 ± 0.2 | 1.4 ± 0.4 | p<0.05 |
| Apo-B | 0.9 ± 0.2 | 0.9 ± 0.2 | 0.11 |
| Neutrophils/lymphocyte | 6.9 ± 5.51 | 2.56 ± 2.38 | p<0.05 |
| CRP | 59.8 ± 55.8 | 1.79 ± 1.08 | p<0.05 |
| Lp (a) | 261 ± 250 | 207 ± 189 | 0.23 |
Table 1: The baseline characteristics between AD group and normal group.
| Variable | Cut-off value | SE | 95% Cl | P value | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| Lp (a) | 138.5 | 0.057 | 0.466-0.690 | 0.179 | 0.62 | 0.5 |
| Neutrophils/ lymphocyte | 2.5 | 0.038 | 0.778-0.928 | 0 | 0.8 | 0.76 |
| CRP | 1.65 | 0.015 | 0.950-1.000 | 0 | 0.98 | 0.44 |
| Neutrophils | 6.63 | 0.037 | 0.808-0.952 | 0 | 0.58 | 0.55 |
Table 2: The factor ROC curve in AD group and normal group.
Data collection
Demographic characteristics, medical history, and laboratory variables were obtained through medical records by cardiologists.
Demographic characteristics included age, gender, and systolic blood pressure, diastolic blood pressure, smoking and drinking.
Medical history mainly included hypertension, diabetes, cerebral haemorrhage, stroke, peripheral arterial disease and Chronic Obstructive Pulmonary Disease (COPD).
The counts of total cholesterol, High Density Lipoprotein Cholesterol (HDL-C), Low Density Lipoprotein Cholesterol (LDL-C), Triglycerides (TG), Lipoprotein (a) (Lp (a)), Apolipoprotein A-I (ApoA-I), Apolipoprotein B (Apo B), creatinines, and uric acid were recorded when patients entered into the hospital. Available standardized methods analysed all blood tests.
Statistical analysis
Categorical variables presented as frequencies and percentages, and comparisons were performed by chi-square or Fisher’s exact test when appropriate. Continuous variables summarized as mean (Standard Deviation, SD) or median (Interquartile Range, IQR) according to their distribution. Student’s t-test, or Mann-Whitney U-test were applied for continuous variables. ROC curve performed. All the statistical analyses performed using SPSS statistical software, version 23.0 [15-17].
Basic characteristics of subjects
In the present study shows the clinical features of patients with AAD, healthy control in Table 1. This study enrolled 100 patients. 50 AAD patients, 50 healthy controls were included based on the according criteria in this study (Figure 1).
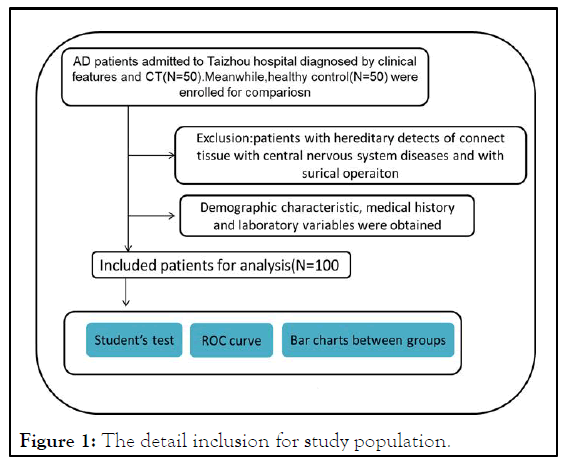
Figure 1: The detail inclusion for study population.
Smoking, drinking, hypertension, diabetes, stroke, and COPD have a significantly higher prevalence in patients with AAD than in healthy subjects.
Furthermore, SCR, BUN, Neutrophils/Lymphocyte, CRP and Lp (a) were significantly higher (p<0.05),while TG levels, TC levels, LDL-C levels and Apo-A1 levels were significantly lower in patients with AAD than healthy control (p<0.05).
The Neutrophils/lymphocyte, CRP levels and Lp (a) levels in AD patients and normal group
As is shown in Figure 2, the neutrophils/lymphocyte rate in AD patients is higher than healthy control. (6.9 ± 5.51 vs. 2.56 ± 2.38, p<0.05). The CRP level in AD patients is higher than healthy control. (59.8 ± 55.8 vs. 1.79 ± 1.08, p<0.05). The Lp (a) in AD patients is higher than healthy control. (261 ± 250 vs. 207± 189, p<0.05).
The ROC analysis
Based on the ROC curves, serum factor predictive effects for aortic dissection were listed as Table 2. Area under the summary receiver operating characteristic curve of Lp (a) is higher than 50% (cut off value: 2.5; sensitivity: 80%, specificity: 76%) [18,19]. Area under the summary receiver operating characteristic curve of CRP is higher than 50% (cut off value: 1.65; sensitivity: 98%, specificity: 44%). Area under the summary receiver operating characteristic curve of Neutrophils is higher than 50% (cut off value: 6.63; sensitivity: 58%, specificity: 55%) (Figure 2).
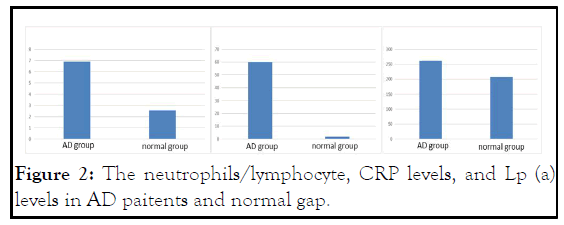
Figure 2: The neutrophils/lymphocyte, CRP levels, and Lp (a) levels in AD paitents and normal gap.
The current research provides evidence about the association between the serum lipoprotein (a) level and the incidence of AAD. Entering the outpatient and emergency clinic, AAD patients had higher Lp (a) level than healthy control. These results suggest that Lp (a) might be a factor identifying AD patients from the healthy control.
In contrast with our results, some published research pointed out a high plasma level of lp (a) in patients with atherosclerosis compared with normal control. V.W. Armstrong demonstrated that 58% of patients with stenosis had Lp (a) levels of 5 mg/dl or more significant, while in the case of those without stenosis, it was only 40%. The high Lp (a) level accelerates the formation of atherosclerotic plaques due to its high affinity for proteoglycans. However, the relationship between Lp (a) level and vessel atherosclerosis is still not known well, especially in AD patients. As mentioned earlier, the lipoprotein (a) level, an indicator of atherosclerosis, was frequently similar in AAD patients compared with healthy individuals [20,21]. Instead, Lp (a) level in non-smoking patients with AD significantly surpassed that of the smoking patients with AD. As Lp (a) frequently measured in daily clinical places or emergency services, it might serve as the indicator for AD patients among those who express a feeling of acute chest pain (Figure 1).
The pathological mechanism of lipoprotein (a) induced vessel atherosclerosis might explain the effect of high Lp (a) level on AAD. The high mortality of AD patients may be related to the low Lp (a) level, which correlated with the process of thrombosis and the process of inflammation. Previous research has indicated that the thrombus formation and the reinforcement of the aortic aneurysm wall were enhanced by the lipoprotein (a). Edelberg J, et al., and Angles-Cano E et al., demonstrated that certain levels of Lp (a) alter the physiological functions of plasminogen in the coagulation and fibrinolytic cascades. In addition to the thrombosis process, there is also an inflammation process when the aortic dissection happens. One published study found that Lp (a) was the primary lipoprotein carrier of OxPL. Then several types of research revealed a pathological role of proinflammatory OxPL in mediating anatomic cardiovascular disease, myocardial infarction, etc. AD patients with low Lp (a) level may be vulnerable to high mortality after one-month follow-up.
Low HDL-C was significantly but not independently related to in-hospital mortality in patients with type A-AAD undergoing emergent surgery. The present study also showed that HDL levels of aortic dissection patients were lower than the healthy control. At the same time, our study demonstrated that AD patients with scarce Lp (a) concentration tended to have higher in-hospital mortality compared to healthy control. One plausible explanation might be based on the concept that Lp (a) is an indicator of nutritional status. Higher Lp (a) might be associated with better nutritional status, which reflects better tolerance to acute medical stress [22].
Based on the valuable Lp (a) level in patients with AAD, we concluded that Lp (a) should be measured instantly after admission and might be used as a biomarker for the prognosis of AAD patients. Extensive prospective studies should be undertaken to evaluate the role of Lp (a) for AAD.
This study indicates that Lp (a) can be evaluated as useful parameters in the emergency clinical approach in the evaluation of risk of acute aortic dissection. Future larger sample studies are required to confirm the results and address the role of these parameters in determining the severity of aortic dissection.
Firstly, the number of enrolled patients in our present study was relatively small. Enroll more targeted patients to compare the relationship between Lp (a) and AAD is beneficial and it is worthwhile for researchers to evaluate the association between dynamic Lp (a) levels and AAD. Secondly, serum Lp (a) levels of patients recorded only once at admission. Last, more extended follow-up periods deserved to explore the effect of serum Lp (a) levels on AAD.
I would like to thank all my teachers who have helped me to develop the fundamental and essential academic competence.
Jianxiao Kong and Hongliang Zhang made contributions to data collection and drafted the manuscript. Yun-yan Zhang made contributions to the analysis and interpretation of the data. All authors read and approved the final manuscript.
This study was supported by a grant, Taizhou Municipal sci-tech bureau program (20ywa50), and Taizhou municipal sci-tech bureau program (1801ky13).
The datasets used and/or analysed during the current study are available from corresponding author on reasonable request.
This research was performed at Taizhou hospital (a tertiary hospital in Zhejiang, China) and the study was approved by the Taizhou hospital ethics committee. The research has been performed in accordance with the declaration of Helsinki. We declare that all methods were performed in accordance with relevant guidelines and regulations. The Taizhou hospital ethics committee has waived written informed consent due to retrospective nature of the study and the use of anonymous retrospective data.
Not applicable.
The authors declared no potential conflicts of interest with respect to the research, author-ship, and/or publication of this article.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhang H (2023) Effects of Lipoprotein (A) in Aortic Dissection Patients with Chest Pain and Healthy Groups: A Cross-Sectional Study. Emergency Med. 13:302 .
Received: 28-Nov-2022, Manuscript No. EGM-22-20478; Editor assigned: 30-Nov-2022, Pre QC No. EGM-22-20478 (PQ); Reviewed: 14-Dec-2022, QC No. EGM-22-20478; Revised: 13-Feb-2023, Manuscript No. EGM-22-20478 (R); Published: 28-Dec-2023 , DOI: 10.35248/2165-7548.23.13.302
Copyright: © 2023 Zhang H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.