International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2022)Volume 10, Issue 5
Context: Neuromuscular electrical stimulation is a rehabilitation method currently used among patients with spinal cord injury, but its results are not well defined yet.
Objective: The purpose of this study was to clinically and radiographically evaluate comorbidities on the feet and ankles of patients with spinal cord injuries who underwent Neuro-Muscular Electrical Stimulation (NMES).
Methods: Between July 2020 and April 2021, 17 patients at the spinal cord injury ambulatory clinic who underwent NMES (group A) were submitted to a clinical and radiographic assessment of their feet and ankles and compared with a spinal cord injury group (group B) who did not undergo NMES and a group of able-bodied individuals (group C). The ANOVA test was used to compare all the three groups and Mann-Whitney test and T test were used to investigate between-groups differences (when p<0.05).
Results: The mean mobility of the subtalar and ankle joint was higher in group C than in groups A and B. Except for calcaneal- ground angle, differences in the mean measurements of hallux-valgus, intermetatarsal, talocalcaneal, talus-first metatarsal and tibial-calcaneal angles were statistically significant between groups A, B and C. Feet deformities, such as grade I ulcers on the lateral malleolus and calcaneus, were found only in group B.
Conclusion: Partial-load NMES is beneficial for patients with SCI, improving range of motion, diminishing rigidity, and may prevent complications such as pressure ulcers.
Neuromuscular electrical stimulation; Spinal cord injury; Foot; Ankle
The annual incidence of spinal cord injury is approximately 54 new cases per million populations in the USA [1]. In turn, some studies estimate 16 to 26 new cases per million populations in Brazil [2]. In the USA, around 80% of individuals with spinal cord injury are male and the mean age of the injury increased from 29 years to 42 years [1]. Furthermore, the main etiology corresponds to car accidents, followed by falls, violent acts (weapon wound) and recreational activities (shallow water diving) [1], and this epidemiological pattern is also observed in brazilian scenario [3,4].
Among complications of spinal cord injury, there are those related to the nervous and osteoarticular systems, such as spasticity, contractures, loss of joint range of motion, and osteoporosis, the result of neurological damage and disuse of the affected limbs. Partial load electrical stimulation of the quadriceps and tibial muscles is a strategy used to reduce these complications [5], which allows individuals to remain in the orthostatic position,also enabling lower limb walking motion with a walker. There is an improvement in energy efficiency, which increases self-performance aiming to execute activities of daily living contributing to improve muscle strength, quality of life [6], range of motion and reduce spasticity [7,8]. The purpose of this study was to clinically and radiographically analyze range of motion on the feet and ankles of patients with spinal cord injuries who underwent neuromuscular electrical stimulation.
Retrospective longitudinal study carried out From July 2020 to April 2021, approved by the research ethics committee of the School of Medical Sciences of UNICAMP (CAAE 26667819.7.0000.5404). All individuals gave written consent following the Helsinki declaration. The research participants have the guarantee of anonymity preserved (Resolution CNS 466/2012). All experiments were performed in accordance with relevant guidelines and regulations. Participants have given their informed consent for participation in the research study.
17 patients at the spinal cord injury outpatient clinic at the University Hospital-UNICAMP (group A) were submitted to a clinical and radiographic assessment of their feet and ankles and were compared with a spinal cord injury group that did not undergo NMES (group B) and with a group of able-bodied individuals (group C). The epidemiological characteristics of groups A and B are, respectively, shown in Tables 1 and 2.
| Patient | Age (years) | Gender | Paraplegic or tetraplegic | Mechanism of trauma | Level of injury | ASIA | Lesion time (years) | Laboratory start (years) | Profession |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 35 | M | Tetraplegic | Gunshot wound | C6 | C6B | 17 | 13 | Athlete |
| 2 | 40 | F | Tetraplegic | Traffic accident | C5 | C5A | 11 | 3 | Retired |
| 3 | 36 | M | Paraplegic | Traffic accident | T9 | T8A | 19 | 18 | Retired |
| 4 | 35 | M | Tetraplegic | Shallow diving | C6 | C5A | 3 | 2 | Retired |
| 5 | 42 | M | Paraplegic | Fall | T9 | T7A | 4 | 1 | Retired |
| 6 | 45 | M | Paraplegic | Traffic accident | T6-T7 | T7A | 5 | 1 | Retired |
| 7 | 41 | M | Tetraplegic | Fall | C3 | C3A | 1 | 1 | Retired |
| 8 | 68 | M | Paraplegic | Fall | T12 | T7A | 25 | 10 | Retired |
| 9 | 52 | M | Tetraplegic | Shallow diving | C5 | C6B | 17 | 16 | Retired |
| 10 | 28 | M | Paraplegic | Traffic accident | T12 | T12A | 3 | 2 | Retired |
| 11 | 21 | M | Paraplegic | Traffic accident | T5 | T4A | 2 | 1 | Student |
| 12 | 55 | M | Paraplegic | Traffic accident | T4-T5 | T4A | 25 | 19 | Retired |
| 13 | 50 | M | Tetraplegic | Traffic accident | C5 | C4A | 19 | 17 | Salesman |
| 14 | 29 | M | Paraplegic | Stab wound | T4 | T4B | 12 | 12 | Retired |
| 15 | 58 | F | Tetraplegic | Traffic accident | C5-C6 | C4B | 11 | 8 | Retired |
| 16 | 61 | F | Paraplegic | Work-related accident | T9-10 | T8D | 19 | 19 | Retired |
| 17 | 43 | M | Paraplegic | Traffic accident | T7-T9 | T7A | 10 | 3 | Retired |
Table 1: The epidemiological characteristics of group A.
| Patient | Age (years) | Gender | Paraplegic or tetraplegic | Mechanism of trauma | Level of injury | Lesion time (years) | Profession |
|---|---|---|---|---|---|---|---|
| 1 | 20 | M | Paraplegic | Gunshot wound | T11 | 2 | Student |
| 2 | 39 | M | Tetraplegic | Diving accident | C5 | 11 | Retired |
| 3 | 30 | M | Tetraplegic | Bike accident | T1 | 2 | Retired |
| 4 | 25 | M | Paraplegic | Car accident | T4 | 5 | Retired |
| 5 | 27 | M | Paraplegic | Gunshot wound | T7 | 5 | Computer technician |
| 6 | 23 | M | Tetraplegic | Car accident | C4 | 2 | Student |
| 7 | 20 | M | Tetraplegic | Diving accident | C6 | 1 | Retired |
| 8 | 59 | M | Tetraplegic | Bike accident | C4 | 1 | Businessman |
| 9 | 25 | M | Paraplegic | Car accident | T7 | 2 | Administrator |
| 10 | 32 | F | Tetraplegic | Car accident | C7 | 7 | Mathematician |
Table 2: The epidemiological characteristics of group B.
The inclusion criteria for group A were spinal cord injured individuals with intact lower motor neurons and from 1 to 19 years of follow-up in the rehabilitation program with NMES. The exclusion criteria were previous clinical and orthopedic pathologies.
The treatment used in group A consisted of maintaining the individual in an erect position with a walker or a support and suspension equipment (tetraplegic) to allow free hip and knee movements, while the feet and ankles were in a neutral position with the aid of a rigid orthosis [9]. A four-channel electrical stimulator, which emits a 25 Hz signal with monophasic rectangular pulses at 300 microseconds duration and maximum intensity of 200 V, stimulated the femoral quadriceps muscles and tibialis anterior muscles are stimulated towards gait for walking motion. Each session was 20 to 30 minutes long and performed twice a week for a minimum of 1 year. The clinical assessment of the feet and ankle included possible deformities and callosities, joint mobility, ulcers, mycosis, and onychocryptosis.
The mobility of subtalar and ankle joints and the radiographic assessment were evaluated by three examiners. The results corresponded to the mean of nine measurements carried out by three examiners. A manual goniometer was used to measure mobility based on American Orthopaedic Foot and Ankle Society’s criteria [10].
The radiographic assessment used standard radiographs with dorsoplantar and profile incidences of support. Professionals measured the hallux-valgus angle, the intermetatarsal angle, talocalcaneal angle (in anterior-posterior and lateral positions), calcaneal-ground angle, talus-first metatarsal angle and tibial- calcaneal angle with a manual goniometer following Smith’s criteria (Figures 1 and 2) [11].
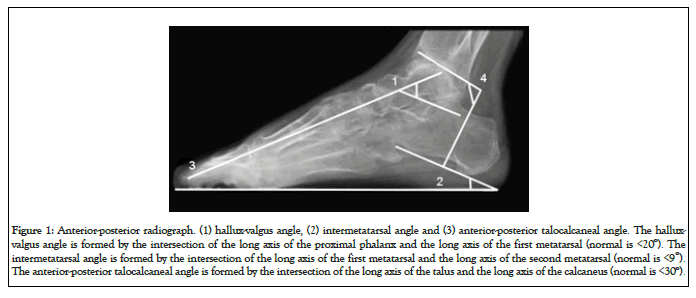
Figure 1: Anterior-posterior radiograph. (1) hallux-valgus angle, (2) intermetatarsal angle and (3) anterior-posterior talocalcaneal angle. The hallux-valgus angle is formed by the intersection of the long axis of the proximal phalanx and the long axis of the first metatarsal (normal is <20º). The intermetatarsal angle is formed by the intersection of the long axis of the first metatarsal and the long axis of the second metatarsal (normal is <9º). The anterior-posterior talocalcaneal angle is formed by the intersection of the long axis of the talus and the long axis of the calcaneus (normal is <30º).
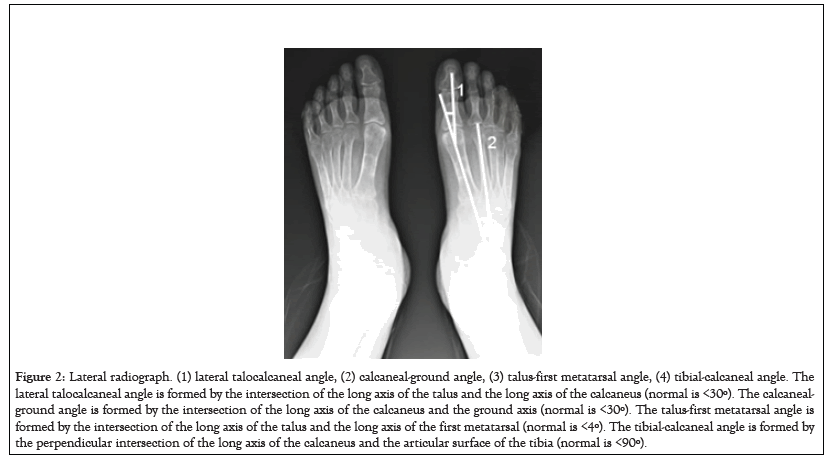
Figure 2: Lateral radiograph. (1) lateral talocalcaneal angle, (2) calcaneal-ground angle, (3) talus-first metatarsal angle, (4) tibial-calcaneal angle. The lateral talocalcaneal angle is formed by the intersection of the long axis of the talus and the long axis of the calcaneus (normal is <30º). The calcaneal- ground angle is formed by the intersection of the long axis of the calcaneus and the ground axis (normal is <30º). The talus-first metatarsal angle is formed by the intersection of the long axis of the talus and the long axis of the first metatarsal (normal is <4º). The tibial-calcaneal angle is formed by the perpendicular intersection of the long axis of the calcaneus and the articular surface of the tibia (normal is <90º).
The results of the clinical and radiographic assessments of the feet and ankles of group A were compared with those of groups B and C according to the same measurement criteria established for group A.
Group A was composed of 17 patients with spinal cord injury who underwent Neuro-Muscular Electrical Stimulation (NMES) as a rehabilitation method. This group consisted of 14 men and three women and the mean age was 43.5 years (range, 21- 68 years). In all, 10 patients were paraplegic and 7 were tetraplegic; causes included traffic accident (9), fall (3), shallow diving (2), gunshot wound (1), stab wound (1) and work-related accident (1). The mean lesion time was 11.9 years (range, 1-25 years), with a mean NMES rehabilitation time of 8.6 years (range,1-19 years).
Group B was composed of 10 patients with spinal cord injury who did not undergo NMES as a rehabilitation method or any other intervention that can influence the main outcome measure through the same period then group A (1 year or more). This group consisted of nine men and one woman, and the mean age was 30 years (range, 20–59 years). Four patients were paraplegic and six were tetraplegic; causes included car accident (4), bicycle accident (2), diving accident (2), and gunshot wound (2). The mean lesion time was 3.8 years (range, 1–11 years).
Group C consisted of 11 able-bodied patients, without spinal cord injury, five men and six women, with a mean age of 29.5 years (range, 18–40 years) who did not undergo NMES as a rehabilitation method or any other intervention that can influence the main outcome measure through the same period then group A (1 year or more).
The ANOVA test was used to compare all three groups. If a significant difference was found (p<0.05), the Mann-Whitney test and T-test were used to investigate between- groups comparisons.
Group A didn’t present deformities, callosities, ulcers, mycosis or onychocryptosis, whereas group B deformities’ included grade I ulcers on the lateral malleolus and calcaneus.
The mean joint mobility in the subtalar mobility comparison was 18.1° in group A, 13.5° in group B and 28.86° in group C. Significant differences were found between groups A and B (p=0.0112), groups A and C (p=0.0021) and groups B and C (p=0.0001) (Table 3).
| Measurement | Injured undergoing electro (group A) | Injured not undergoing electro (group B) | Normal patients (group C) | Comparis on of the three groups | Injured underg oing x not underg oing electro | Injured underg oing electro x normal | Injured not underg oing electro x normal | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Median | Mean | Standard deviation | Median | Mean | Standard deviation | Median | P-value | P-value | P-value | P-value | |
| Subtalar joint | 18.1 | 7.6 | 18.5 | 13.5 | 5.8 | 10 | 28.86 | 9.4 | 30 | <0.0001* | 0.0112* | 0.0021* | 0.0001* |
| Ankle joint | 40.4 | 13.1 | 40 | 34.3 | 10.7 | 35 | 63.6 | 3.9 | 65 | <0.0001* | 0.0353* | <0.0001* | <0.0001* |
| Hallux- valgus angle | 19.3 | 4.5 | 20 | 14.75 | 5.1 | 14 | 15.6 | 7 | 12 | 0.0429* | 0.0004* | 0.0716 | 0.3412 |
| Intermetatarsal angle | 8.7 | 1.8 | 9 | 8.12 | 2.6 | 9.5 | 10.1 | 2 | 10 | 0.0231* | 0.4122 | 0.0804 | 0.0423* |
| Anterior-posterior talocalcaneal angle | 16.3 | 4.8 | 16 | 18.81 | 2.8 | 20 | 24 | 5.5 | 24 | 0.0003* | 0.0232* | 0.0006* | 0.0054* |
| Lateral talocalcaneal angle | 35.5 | 15.9 | 30 | 31.12 | 6.4 | 31.3 | 44.7 | 5 | 44.5 | 0.0302* | 0.4122* | 0.0016* | <0.0001* |
| Calcaneal-ground angle | 24.2 | 4 | 24 | 25.31 | 6 | 26.3 | 26.8 | 6 | 26 | 0.309 | 0.1435 | 0.1241 | 0.2254 |
| Talus-first metatarsal | 15.8 | 4.7 | 16 | 19.31 | 9.7 | 20 | 4 | 4.7 | 5 | <0.0001* | 0.0034* | <0.0001* | <0.0001* |
| Tibial-calcaneal angle | 82 | 8.4 | 85 | 69.37 | 14.1 | 85 | 81.8 | 12.8 | 90 | 0.0020* | <0.0001* | 0.1669 | 0.0716 |
Note:*Statistically significant measurements
Table 3: Significant differences between groups A, B and C.
In the ankle joint, mean mobility was 40.4° in group A, 34.3° in group B and 63.6° in group C. Significant differences were found between groups A and B (p=0.0353), groups A and C (p<0.0001), and groups B and C (p<0.0001) (Table 3).
The mean hallux-valgus angle was 19.3° for group A, 14.75º for group B and 15.6° for group C. Significant differences were found between groups A and B (p=0.0004) (Table 3).
The mean intermetatarsal angle was 8.7º for group A, 8.12° for group B and 10.1° for group C. Significant differences were found between groups B and C (p=0.0423) (Table 3).
The mean talocalcaneal angle, in the anterior-posterior position, was 16.3° for group A, 18.81° for group B and 24° for group C. Significant differences were found between groups A and B (p=0.0232), groups A and C (p=0.0006) and groups B and C (p=0.0054) (Table 3).
The mean talocalcaneal angle, in the lateral position, was 35.5° for group A, 31.12° for group B and 44.7° for group C. Significant differences were found between groups A and C (p=0.0016) and groups B and C (p<0.0001) (Table 3).
The mean calcaneal-ground angle was 24.2° for group A, 25.31° for group B and 26.8° for group C. There were no significant differences found between groups A and B, groups A and C and groups B and C (p>0.05) (Table 3).
The mean talus-first metatarsal angle was 15.8° for group A, 19.31° for group B and 4° for group C. Significant differences were found between groups A and B (p=0.0034), groups A and C (p<0.0001) and groups B and C (p<0.0001) (Table 3).
The mean tibial-calcaneal angle was 82° for group A, 69.37° for group B and 81.8° for group C. Significant differences were found between groups A and B (p<0.0001) (Table 3).
Group A population had a mean age of 43.5 years, slightly higher than the epidemiology expected (42 years). The majority of the lesions in groups A and B are due to traffic-related trauma and are in accordance with National Spinal Cord Injury Statistical Center [1].
Foot deformities found in group B were grade I ulcers on the lateral malleolus and calcaneus, which can be prevented with daily skin inspections, use of adequate shoes and use of pressure redistribution support surfaces [12]. The absence of foot deformities, such as ulcers, callosities, mycosis and onychocryptosis, in group A may be due to individuals’ high level of education and better access to health service with rehabilitation treatment for spinal cord injury.
Concerning joints’ mobility, the mean subtalar and ankle joint values for group C (able-bodied individuals) were higher than values for groups A and B. Moreover, the mobility in group B (did not undergo NMES) was lower than that in group A (underwent NMES). This diminished range of motion occurred predominantly because of contracture caused by shortening and stiffening of connective tissue and loss of sarcomeres and muscle fibers [13]. The mobility difference between groups A and B may be due to neuromuscular electrical stimulation that is used to improve the range of motion and muscle spasticity [7].
Radiographic assessments for groups A and C showed normal mean hallux–valgus angles, intermetatarsal angles, calcaneal– ground angles, tibial–calcaneal angles and talocalcaneal angles in profile position.
The radiographic assessments of group A when compared with able-bodied patients (group C) the difference was statistically significant. However, group A did not present clinical repercussions in the feet, which remained planted and in an adequate position for walking with a load. This suggests that treatment with partial- load and neuromuscular electrical stimulation keeps the feet and ankles in an adequate walking position in patients with spinal cord injury.
Moreover, the radiographic alterations and diminished mobility observed in group B patients, when compared with group C, indicates that group B patients’ feet were more rigid than group A patients’. This stiffness must be considered because group A patients realize NMES, which is a beneficial treatment because it can improve range of motion, muscle spasticity and muscle strength, and control balance and posture, promoting better mobility [7].
Some limitations of this study include the manual method used to measure the angles and mobility of patients’ feet and ankles. The measures were carried out by three professionals and the mean values were obtained by combining measurements for each radiographic angle and each joint mobility. The manual method was used due to the lack of a digital goniometer.
Few studies were found in the literature regarding the foot and ankle patterns of patients with spinal cord injuries. Neuromuscular electrical stimulation can provide an effective rehabilitation strategy in managing spasticity. However, a recommendation of the stimulation parameters cannot be accurately assumed because of high variability in the methodology, design, and heterogeneity of the studies. The lack of research on this topic indicates the necessity of further studies to define standards that allow comparison of the feet and ankles patterns found in different treatments for this group of patients, who attempt to regain the ability to walk.
It is possible to conclude that the partial-load NMES maintains the feet and ankles of patients with spinal cord injury in an adequate walking position. It also has beneficial effects for these patients, with a significant reduction of muscle and connective tissue stiffness, an increase in range of motion and prevention of complications, such as pressure ulcers, contributing to a better quality of life.
The authors declare that they have no conflict of interest.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
Citation: Bianchi LP, Bittar CK, e Silva RC, Silvestre O, Cliquet Jr A (2022) Effects of Neuromuscular Electrical Stimulation on the Feet and Ankles of the Spinal Cord Injured. Int J Phys Med Rehabil.10:638.
Received: 09-Jun-2022, Manuscript No. JPMR-22-17877; Editor assigned: 14-Jun-2022, Pre QC No. JPMR-22-17877 (PQ); Reviewed: 28-Jun-2022, QC No. JPMR-22-17877; Revised: 06-Jul-2022, Manuscript No. JPMR-22-17877 (R); Published: 15-Jul-2022 , DOI: 10.35248/2329-9096-22.10.638
Copyright: © 2022 Bianchi LP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.