Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2011) Volume 1, Issue 1
Introduction: Preterm labor is the leading cause of prenatal and neonatal mortality morbidity and long term neurodevelopmental problems.so that different treatments have been employed in order to suppress preterm labor from several years ago. Magnesium sulfate is often used as first line in suppressing of preterm labor. Side effect of this : thirst, hyperthermia, headache, diplopia, respiratory depression and rare cases respiratory paralysis and arrest.In later pregnancy progesterone may be important in maintaining uterine quiescence by limiting the production of stimulatory prostaglandins and inhibiting the expression of contraction – associated protein genes with in the myometrium natural progesterone administrated vaginally is considered is effective in suppression of preterm birth and safe for both mother and fetus. We take a decision that compare the ability of magnesium sulfate with progesterone in suppression of preterm labor.
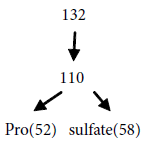
Methods: In this randomized clinical trial 132 cases were chosen form pregnant women between the 26-34 weeks of pregnancy who were suffering from preterm contractions of uterus with intact amniotic sac and cervical dilatation of less than 4cm.these women had referred to obstetric ward of Ali – Ebne – Abitalib hospital, Zahedan, during the years of 2008-9 and randomly were `divided into two equal groups (66 cases in each group). The results were analyzed by chi square and T test with spss software.
Results: In first group primarily 4 grams of magnesium sulfate infused. And then 10 grams (2grams per hours) was continued.in second group progesterone used 200 mg vaginal suppository as single dose.in first group delivery during 48 hour was failure of treatment and second group if no controlled contraction of uterus after 1 hour, changed to magnesium sulfate and this case was failured. From 66 women in magnesium sulfate group in 58 case (89%) suppressed delivery at least for 48 hours.In second group from 66 women 52 case (79%) suppressed delivery at least for 48 hours.in this study differentiation was no significant (p value=0.161) in two group. 95 percent women in first group (magnesium sulfate) had side effects and 5 percent women progesterone group had involved with side effects.
Conclusion: This finding show the ability of progesterone in suppression of preterm labor is similar to magnesium sulfate however maternal side effect of magnesium sulfate was 95% while it was no for progesterone.
Labor happens when some mechanisms drive the uterus to deliver the gestation product. If it happens between the 20 and 37 pregnancy weeks, it is called premature labor. Theoretically, this happens as a consequency of pathologic activation of the labor process [1].
Premature labor, which occurs in 7.23% of deliveries [2], is associated with prenatal morbidity and mortality [2,3] American Academy of Pediatrics and American College of Obstetricians and Gynecologists have suggested below criteria for diagnosis of preterm labor:
1- Presence of 4 uterine contractions in 20 minutes or 8 contractions in one hour accompanied by progressive cervical changes,
2- Cervical dilatation greater than one centimeter,
3- Cervical effacement equal or greater than 80% [4].
Prevention of delivery is still a great challenge when dealing with preterm labor. Currently, there is no evidence based proven treatment for this struggle. Different tocolytic regimens (e.g., beta blockers, magnesium sulfate, anti-prostaglandins and calcium channel blockers) have been used to suppress uterine activity in order to improve neonatal outcome [1].
Magnesium ion in high concentrations is able to alter the contractility of the myometrium through antagonizing calcium ion. Clinical evidences show that magnesium in pharmacologic doses is able to suppress the labor. But Grimes et al, showed that magnesium sulfate is ineffective as a tocolytic [4].
Progesterone is a steroidal hormone which plays important roles throughout pregnancy. Early in pregnancy, it is secreted by corpus luteum until the placenta takes over in weeks 7 to 9 and its main role is to maintain the product of gestation. In the second half of the pregnancy, role of progesterone is less clear. It is possible that it plays a role in suppressing the myometrial contraction by inhibiting the stimulatory prostaglandins and related protein genes [5]. In a meta-analysis of three randomized controlled trials, effectiveness of progesterone in treating preterm labor was shown [6]. Systematic review of 9 clinical trials also showed the efficacy of these products [7].
Many studies have shown that tocolytic agents are effective for 2-7 days, a golden time to administer corticosteroids to mature the fetal lungs. Tocolytic agents are contraindicated in placenta abruption, intrauterine infection, fetal anomalies and placenta previa [8].
When plasma level of magnesium reaches 10 mEq/L, patellar reflex disappears and respiration depression happens. This is a sign of imminent magnesium toxicity [4]. Medroxyprogesterone has been effective in suppressing preterm labor and anti-inflammatory effects in animal models. Defonseca et al. (2003) reported the effect of vaginal progesterone in decreasing premature delivery in high risk groups [4].
Looking at the side effects of magnesium sulfate in one hand (maternal respiratory depression, diplopia, muscle paralysis and rarely cardiac arrest) and progesterone which is relatively safe in the other hand [3], this study was designed to compare the efficacy and safety of these two drugs in management of premature labor.
This is a randomized controlled trial. This study after of ethics board approval Participants were mothers with the diagnosis of preterm delivery between weeks 26 to 34 referred to the Ali-Ebne- Abitaleb hospital in Zahedan, Iran from September 2008 to December 2009. Patients were assigned to the groups alternately (66 patients in each group).
Inclusion criteria: being between 26 to 34 weeks of pregnancy, having 4 uterine contractions in 20 minutes or 8 in one hour, cervical dilatation less than 1 centimeter, intact amniotic sac and single fetus.
Exclusion criteria: placenta abruption and bleeding, hypotonic uterus, amniotic fluid leakage, fetal anomalies, signs of chorioamnionitis.
In one group, magnesium sulfate was administrated intravenously as 4 grams loading dose and then maintenance dose of 10 grams (2 grams) per hour to suppress contraction. During treatment (48hr), vital signs, patellar reflex and urine output volume were checked and documented hourly in order to be aware of early signs of toxicity.
In the intervention group, 200 mg of vaginal progesterone (Abureihan pharmaceuticals) was administrated as a single dose. Uterine contraction and fetal heart rate were assessed by frequent examinations for those patients whom the uterine contractions continued after one hour, it was considered as failure of treatment and magnesium sulfate was administrated for rothin hospital methods.
Of 132 patients 110 were considered eligible. Paper case report files were transcribed to SPSS version 17 analyzed by Chi Square test. Out of 132 participants, tocolysis was successful in 110 (83%) for 48 hours. 52 of these patients were from the progesterone group and 57 from the magnesium sulfate group (Table 1). There was no significant difference between the groups (p= 0.16).
| suppress labor | Unsuppressed labor | p Value | |||
|---|---|---|---|---|---|
| Medication | Number | Percent | Number | Percent | |
| Progesterone | 52 | 79 | 14 | 21 | 0.16 |
| Magnesium Sulfate | 58 | 89 | 8 | 12 | |
| sum | 110 | 83 | 22 | 17 | |
Table 1: Efficacy of progesterone versus magnesium sulfate in managing preterm labor.
In the progesterone group, side effects were observed in 5% of patients (headache, nausea and restlessness, each in one patient), however, tocolysis was effective in these patients and completely disappeared after 48 hours. None of the 63 patients showed treatment adverse effects. In magnesium sulfate, 95% of patients experienced side effects (most common was thirst in 32% followed by hyperthermia 24%) (Table 2).
| Hyperthermia | Vomiting | Nausea | Thirst | Vertigo | restlessness | Headache | |
|---|---|---|---|---|---|---|---|
| Progesterone | - | - | %1 | - | %1 | %1 | |
| Magnesium Sulfate | %24 | %1 | %12 | %30 | %18 | - | %11 |
Table 2: Prevalence and types of side effects observed in the study.
Findings of this study shows that the efficacy of magnesium sulfate and progesterone in management of preterm labor are similar, however, maternal side effects of magnesium sulfate in 95% patients, and in the progesterone group 3% were observed.
To suppress the premature labor, vaginal progesterone was effective in 79%, when compared to 89% of patients in magnesium sulfate group.
Defonseca et al. [9] administrated vaginal progesterone (200 mg/day) between 24 and 34 weeks in patients with short cervix. As a result, risk of premature labor was decreased from 34% to 19%.
In this study, severity of the side effects observed in the progesterone group were mild to moderate and were completely resolved after 48 hours. On the other hand, despite of frequent control of the vital signs, severity of side effects of magnesium sulfate was more severe and irksome.
Different studies have not shown any maternal or fetal side effects related to progesterone. (7) The most common adverse effect of magnesium sulfate is thirst (30%) and hyperthermia (24%) which occurs simultaneously in 87% of cases which results in irritability and restlessness.
Sakhavar et al performed a study in 2004 to 2006 to compare the efficacy of magnesium sulfate and hCG in management of preterm labor. In that study, the most common side effects of magnesium sulfate were hyperthermia and thirst (observed in 53% and 48% of patients respectively). All patients in the magnesium sulfate group experienced some kind of adverse effects [10].
Despite the advantages of progesterone, it should be noted that the final purpose for tocolysis is improving fetal outcome. Therefore, it is suggested for future studies to use the data of this research along with other information to evaluate the efficacy of progesterone in decreasing mortality, morbidity and need to neonatal intensive care. We hope that future studies will introduce safer and more effective tocolytic regimens.
This study was supported by a dissertation grant from School of Medicine, Zahedan University of Medical Sciences, the authors would like to thank the subjects who willingly participated in the study.