Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research Article - (2024)Volume 13, Issue 2
Objective: To systematically evaluate the clinical efficacy and safety of traditional Chinese medicine in the treatment of Post-Stroke Depression (PSD), thereby providing a solid evidence-based foundation for its clinical application.
Materials and methods: Rational inclusion and exclusion criteria were established. A comprehensive search was conducted through databases such as China National Knowledge Infrastructure (CNKI), Virus Protein (VIP), Chinese Biomedical (CBM) database, Wan Fang and PubMed, complemented by manual searches of relevant references, to collect all Randomized Controlled Trials (RCTs) on traditional Chinese medicine for treating PSD. The literature search was concluded in August 2023. Two researchers independently screened the literature, extracted data using Excel and assessed the quality of included studies using the Cochrane Handbook for Systematic Reviews. Review Manager (RevMan) 5.4 was used for assessing overall effectiveness, changes in depression scale scores (Hamilton Depression (HAMD) rating scale), changes in neurological deficit scores (Modified Edinburgh-Scandinavian Stroke Scale (MESSS), National Institutes of Health Stroke Scale (NIHSS), China clinical neurological deficit of Stroke patients Standard for evaluation (CSS)), changes in the Barthel Index (BI) for daily living activities, changes in Traditional Chinese Medicine (TCM) symptom scores and incidence rates of adverse events. Heterogeneity testing, combined effect size analysis, sensitivity analysis, hypothesis testing, forest plot construction and analysis and publication bias assessment using funnel plots were conducted to systematically evaluate the clinical efficacy and safety of traditional Chinese medicine in treating PSD.
Conclusion: Traditional Chinese medicine has been proven to be effective in treating PSD with a low risk of adverse reactions, making it worthy of widespread clinical application. However, the overall quality of the included studies is relatively low, with certain biases present, which affects the reliability of the conclusions of this meta-analysis. Future high-quality, large-sample, multi-center and rigorously scientific randomized controlled trials are anticipated to continually refine and update the systematic reviews to validate the clinical efficacy of traditional Chinese medicine in treating PSD.
Traditional Chinese medicine therapy; Post-stroke depression; Randomized controlled trial; Meta-analysis
RCT: Randomized Controlled Trial; PSD: Post-Stroke Depression; RR: Risk Ratio; OR: Odds Ratio; RD: Risk Difference; MD: Mean Difference; SMD: Standardized Mean Difference; CI: Confidence Interval; DSM-III: Diagnosis and Statistical Manual of Mental Disorders-Third Edition; ICD-10: International Classification of Diseases-Tenth Edition; CCMD-3: Chinese Classification of Mental Disorders-Third Edition; 5-HT: 5-Hydroxytryptamine; BDNF: Brain Derived Neurotrophic Factor; HAMD: Hamilton Depression scale; MESSS: Modified Improved Edinburgh-Scandinavia Score; NIHSS: National Institutes of Health Stroke Scale; CSS: China clinical neurological deficit of Stroke patients Standard for evaluation; BI: Barthel Index; ADL: Activity of Daily Living scale; SDS: Self-rating Depression Scale; NE: Norepinephrine; DA: Dopamine
Post-Stroke Depression (PSD) is a condition caused by permanent tissue damage due to thrombotic or hemorrhagic events and is one of the most common and serious complications following a stroke. It is also the most prevalent mental disorder among stroke survivors, with about one-third of patients experiencing PSD at some stage after a stroke [1]. Studies indicate that approximately 30% of stroke patients develop PSD, with a prevalence rate of about 29%-35% in the first five years [2,3]. PSD not only delays the recovery of neurological functions and significantly reduces the quality of life but also increases the recurrence, disability and mortality rates of stroke. Moreover, it causes considerable psychological distress and financial burden to the patients, their families and even society [4,5].
Currently, western medicine primarily relies on antidepressants, such as tetracyclic and tricyclic antidepressants, which remain the most popular choices for treating PSD [6]. However, these medications require at least 3-4 weeks to elicit a clinical response and only 50% of patient’s experience relief [7]. The use of various antidepressants not only increases the risk of stroke recurrence but also presents contraindications when combined with certain stroke medications [8]. Moreover, poor long-term medication adherence in some patients may lead to more severe consequences. When the response to Western medication is insufficient, Traditional Chinese Medicine (TCM) may serve as a complementary or alternative treatment.
The primary TCM treatments for PSD include Fan et al., Yawen et al., Qingli et al., and Zhiqiang et al., [9-12]. Based on precise syndrome differentiation, these Chinese herbal formulas exhibit a faster onset of action than conventional medications, offer comprehensive treatment targeting both the cause and symptoms, affect multiple targets and have milder side effects [13]. The clinical application of TCM in treating PSD has demonstrated minimal side effects and high safety, with a high acceptance among patients. Animal studies have shown that TCM can significantly improve depressive-like behaviors and neurological functions in animals with PSD, suggesting that TCM deserves more extensive application and research in treating PSD to explore more effective treatment methods [14].
In reviewing past randomized controlled studies on post-stroke depression, we found that systematic reviews on the treatment of PSD with TCM are outdated. Updating such literature can help us better assist patients with PSD in formulating the latest treatment strategies. Therefore, it is necessary to re-examine the literature and conduct a systematic review and meta-analysis of the research on TCM treatment for PSD.
Inclusion and exclusion criteria
Inclusion criteria: It includes study type, study subjects, intervention measures and outcome indicators.
(a): Study type: Randomized control trial.
(b): Study subjects: Patients with PSD, no restrictions on age or region. Stroke must meet the diagnostic criteria established by the national cerebrovascular disease academic conference and be confirmed by head Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) results or comply with other cerebrovascular disease diagnostic guidelines. The diagnostic criteria for depression must confirm to one of the following such as the International Classification of Diseases-Tenth edition (ICD-10), the third edition of the Chinese Classification of Mental Disorders (CCMD-3) or the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) or its subsequent versions.
(c): Intervention measures: In addition to routine stroke treatment, the test group uses traditional Chinese medicine therapy or a combination of traditional Chinese medicine and another therapy. Traditional Chinese medicine treatments include oral administration and fumigation therapy. Other measures include, but are not limited to, western medicine treatment (no restrictions on the formulation, dosage or course of treatment of traditional Chinese medicine). The control group is given the same basic stroke treatment as the experimental group and only the same additional therapy as the experimental group.
(d): Outcome indicators: Should include at least one of the following: clinical efficacy rate based on Hamilton Depression scale (HAMD) scores, HAMD scores, Modified Edinburgh-Scandinavian Stroke Scale (MESSS) scores, National Institutes of Health Stroke Scale (NIHSS) scores, Barthel Index (BI) scores, Activities of Daily Living (ADL) scores, traditional Chinese medicine syndrome scores, clinical efficacy rate based on traditional Chinese medicine syndrome scores, 5-Hydroxytryptamine (5-HT) levels or the incidence rate of adverse events.
Exclusion criteria: It includes studies with evident flaws in design, duplicate publications, studies in which the experimental group received other major traditional Chinese medicine treatments such as acupuncture, music therapy, auriculotherapy, etc., and studies from which effective outcome indicators could not be obtained.
Search strategy
Search the electronic databases for literature published up to August 18, 2023 such as PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), Wanfang Medical Network and China Biology Medicine disc. The English search keywords are traditional Chinese medicine or Chinese herbal medicine or traditional Chinese medicine treatment or traditional Chinese medicine preparations or traditional Chinese medicine decoction or herbal oral administration or herbal fumigation and post-stroke depression or post cerebral infarction depression or PSD and RCT or clinical experiment or clinical observation. Also, unpublished studies registered on the International Prospective Register of Systematic Reviews (PROPEROS) website were searched.
Data collection and analysis
Literature screening: First, duplicate articles were removed using the deduplication feature of EndNote X9, followed by a recheck. Next, titles and abstracts of the remaining studies were reviewed to exclude those not meeting the inclusion criteria. Subsequently, the full text of the remaining articles was thoroughly read to decide on their inclusion. This process involved documenting the number and reasons for excluding articles. Two authors independently carried out the above tasks and any disagreements were resolved through consultation with a third author.
Data extraction and management: Data were extracted using a pre-designed data extraction form, which included the first author's name, publication year, type of study, diagnostic criteria, sample sizes of the experimental and control groups, intervention measures and outcome indicators. This task was also independently carried out by two authors, with any disagreements resolved through discussion with a third author.
Risk of bias assessment for included studies: The risk of bias in RCTs was assessed using the tool recommended by the Cochrane Handbook, focusing on six domains such as selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting of results) and other bias.
Two authors independently evaluated the risk of bias in each domain, categorized as low risk of bias, high risk of bias or unclear risk of bias. A third author resolved any discrepancies. A high risk of bias significantly affects the credibility of the results, a low risk of bias is unlikely to have a major impact even if present and unclear risk of bias indicates that the existing bias may affect the credibility of the outcomes.
Meta-analysis: Review Manager 5.4 software was utilized for data analysis. Dichotomous variables were analyzed using the Mantel-Haenszel (M-H) method, Odds Ratios (ORs) and their 95% Confidence Intervals (CIs). Continuous data were analyzed using the inverse variance method, Mean Differences (MDs) and their 95% CIs. Heterogeneity among the included studies was assessed using the P-value from the Q test and the I² statistic. If p>0.1 and I² ≤ 50%, indicating low heterogeneity, a fixed-effect model was used for the meta-analysis. If p ≤ 0.1 and I²>50%, indicating high heterogeneity, a random-effects model was used. The combined effect size was determined using the Z test, with p<0.05 indicating statistical significance.
Publication bias analysis: Publication bias was assessed using funnel plots in Review Manager (RevMan) 5.4. This method involves creating a scatter plot with treatment effect on the X-axis and sample size on the Y-axis and visually inspecting the symmetry of the scatter points to identify publication bias. If the funnel plot shows most studies at the top or middle with fewer studies at the base and the plot is approximately symmetrical, it suggests minimal publication bias. Conversely, asymmetry indicates significant publication bias. This study only assessed publication bias using the funnel plot method for analyses with more than ten included studies.
Search results
The search results yielded 39 articles from Web of Science, 227 from Cochrane, 261 from VIP, 559 from Wanfang Database, 60 from CNKI, 36 from PubMed, 6 from Embase and 159 from CBM, with 0 obtained through other sources. After removing duplicates using Endnote, 1118 articles remained [15-25]. Upon reviewing titles and abstracts, 1084 articles were excluded. After full-text review, 22 articles were included in the meta-analysis [26-36]. Figure 1 shows the flow diagram (Figure 1).
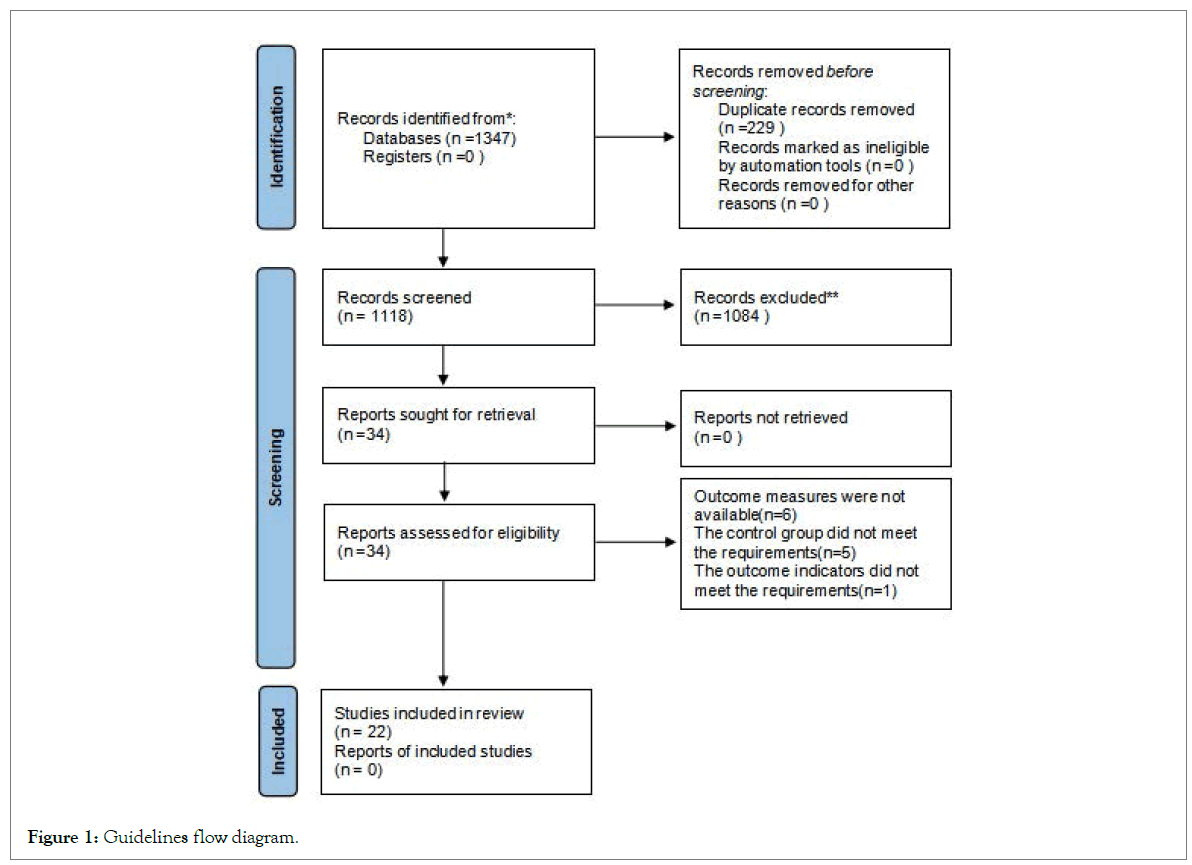
Figure 1: Guidelines flow diagram.
Characteristics of included studies and risk of bias assessment
The basic characteristics of the included studies are detailed in Table 1. The 22 RCTs encompassed 1659 participants. The risk of bias in the RCTs was assessed independently by two researchers using the Risk of Bias (ROB2) tool, with any discrepancies resolved by a third researcher. Figures 2 and 3, shows the specific risk of bias assessment results (Table 1, Figures 2 and 3).
| S. No. | First author | Year | Region | Sample size | Age | Intervention method | Outcome | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Control arm (M/F) | Intervention arm (M/F) | Control arm | Intervention arm | Control arm | Intervention arm | |||||
| 1 | Xu Lijuan | 2021 | Jiangsu | 30 | 30 | 55.4 ± 0.9 | 54.4 ± 0.7 | Escitalopram oxalate tablets | Escitalopram oxalate tablets+Traditional Chinese medicine decoction 'puzzle Jieyu decoction' | [1-4] |
| 2 | Bai Yu | 2021 | Xinjiang | 52 | 52 | 65.27 ± 8.78 | 65.78 ± 8.92 | Antidepressive therapy | Antidepressive therapy+Chaishu sijun decoction | [1,2,5-11] |
| 3 | Bai Yun | 2020 | Hebei | 30 | 30 | 56.70 ± 9.527 | 56.60 ± 9.432 | Flupentixol and Melitracen tablets | Flupentixol and Melitracen tablets+Added Huangqi Chifeng Tang granules | [1,5,12,13,15] |
| 4 | Gan Qin | 2022 | Jiangxi | 36 | 30 | 66.04 ± 8.81 | 65.00 ± 9.52 | Flupentixol and Melitracen tablets | Flupentixol and Melitracen tablets+Flavored peach four things soup | [1,2,14,15] |
| 5 | Jian Ming | 2020 | Shanxi province | 44 | 44 | 18-70 | 18-70 | Basic therapy+Flupentixol and Melitracen tablets | Basic therapy+Ganmai Jianpi decoction | [2,4,15,16] |
| 6 | Li Qiang | 2021 | Xi’an city | 36 | 35 | 63.74 ± 7.54 | 60.29 ± 11.51 | Cerebrovascular drugs Citicoline Sodium tablets, Acupuncture and rehabilitation therapy (Basic treatment of stroke)+Oral flupethixene melitracen tablets | Cerebrovascular drugs Citicoline Sodium tablets, Acupuncture and rehabilitation therapy+Oral Chinese medicine Anao pill | [1,17-19] |
| 7 | Li Zhi | 2022 | Henan | 39 | 39 | 65.56 ± 4.32 | 66.12 ± 4.41 | Flupentixol and Melitracen tablets | Flupentixol and Melitracen tablets+Depression-calming Chinese medicine | [1,2,4,5,20-23] |
| 8 | Lin Yong | 2021 | Chengdu city | 31 | 32 | <50, >75 | <50, >75 | Basic treatment of stroke+Oral treatment with current specialist antidepressant medications | Basic stroke treatment protocol+Oral antidepressant medication currently administered by a specialist+Chinese medicine preparation added flavor buyang Huanwu decoction no decoction granules | [1,2,4,15,16] |
| 9 | Lu Kesheng | 2019 | Henan | 42 | 42 | 64.10 ± 5.11 | 62.51 ± 5.66 | Flupentixol and Melitracen tablets | Flupentixol and Melitracen tablets+Depression-calming Chinese medicine | [1,2,16,20] |
| 10 | Ren Yankun | 2019 | Hebei province | 100 | 100 | ≥ 60 | ≥ 60 | Paroxetine Hydrochloride anti-depressive therapy | Paroxetine Hydrochloride anti-depressive therapy+Write your own prescription | [1,4,25,27] |
| 11 | Shen Si | 2019 | Gansu province | 30 | 30 | 64.23 ± 5.18 | 65.51 ± 6.32 | Flupentixol and Melitracen tablets | Flupentixol and Melitracen tablets+Self-designed Chinese medicine Jieyu Quyu decoction | [2,20] |
| 12 | Shen Si | 2020 | Gansu province | 30 | 30 | 64.23 ± 5.18 | 65.51 ± 6.32 | Routine treatment in internal medicine | Routine treatment in internal medicine+Add self-made traditional Chinese medicine Jieyu Quyu Tang | [1,2] |
| 13 | Su Guang | 2021 | Guangdong province | 59 | 58 | 18-70 | 18-70 | Conventional medication and rehabilitation nursing treatment | Conventional medication and rehabilitation nursing treatment+Intervention of horticultural therapy with aromatherapy and Chinese Herbal medicine | [2,4,25,26,28] |
| 14 | Wang Yunna | 2021 | Inner mongolia autonomous region | 26 | 26 | 50 ~ 70 | 50 ~ 70 | Oxygen therapy, nutritional brain nerve drug therapy (basic treatment) | Basic treatment+Chai Gui Wen Dan Ding Zhifang | [16,25,26,29,33] |
| 15 | Wang Zongke | 2021 | Guangxi | 29 | 29 | 59.00 ± 15.00 | 58.50 ± 13.50 | Fluose fine hydrochloride | Fluose fine hydrochloride+Chaihu Shugan Tang | [2,24,34] |
| 16 | Ye Changjun | 2019 | Liaoning province | 30 | 30 | 57.2 ± 16.1 | 56.7 ± 15.8 | Fluoxetine hydrochloride | Treatment of Acacia flowers combined with Ya Long Anti Shuan Pill | [2,5] |
| 17 | Zhang Junru | 2022 | Shandong province | 36 | 36 | 60 -80 | 60 -80 | Oral sertraline hydrochloride | Sertraline Hydrochloride+Oral traditional Chinese medicine formula granules with modified Jiaotai pills | [1,2,5,15,16,24,25] |
| 18 | Zhao Yawei | 2018 | Hebei province | 30 | 30 | 62.42 ± 9.83 | 61.23 ± 10.5 | Oral sertraline hydrochloride | Oral Yiqi Tongluo granules | [2,24,,30] |
| 19 | Zhou Yangyang | 2019 | Shandong province | 32 | 32 | 45-75 | 45-75 | Basic treatment of stroke+Oral Duloxetine hydrochloride enteric capsule | Basic treatment of stroke+Oral Duloxetine hydrochloride enteric capsule+Ding Xin Tang Jia Wei Fang | [1,2,5,15,16,24] |
| 20 | Tan Qianqian | 2021 | Guangdong province | 48 | 48 | 67.98 ± 6.82 | 68.22 ± 7.14 | Oral Paroxetine hydrochloride tablets | Oral Paroxetine hydrochloride tablets+Traditional Chinese medicine prescription | [1,2,4,9,31,32] |
| 21 | Wanhaitong | 2023 | Zhejiang province | 52 | 52 | 63.2 ± 12.5 | 63.9 ± 13.2 | Stroke treatment+Oral Fluoxetie Hydrochloride Caule | Stroke treatment+Oral Fluoxetie Hydrochloride Caule+Treatment with the agreement formula of supplementing qi, promoting blood circulation and relieving depression; Single use of Qi tonifying, blood activating anddepression relieving protocol | [1,2,15] |
| 22 | Wang Ru | 2019 | Jiangsu province | 30 | 30 | 55.4 ± 0.9 | 54.4 ± 0.7 | Flupentixol/Melitracen | Flupentixol/Melitracen + Implementing modified traditional Chinese medicine prescriptions (Chaihu Shugan San) for treatment | [2,5] |
Note: M: Male; F: Female.
Table 1: Characteristics of included studies.
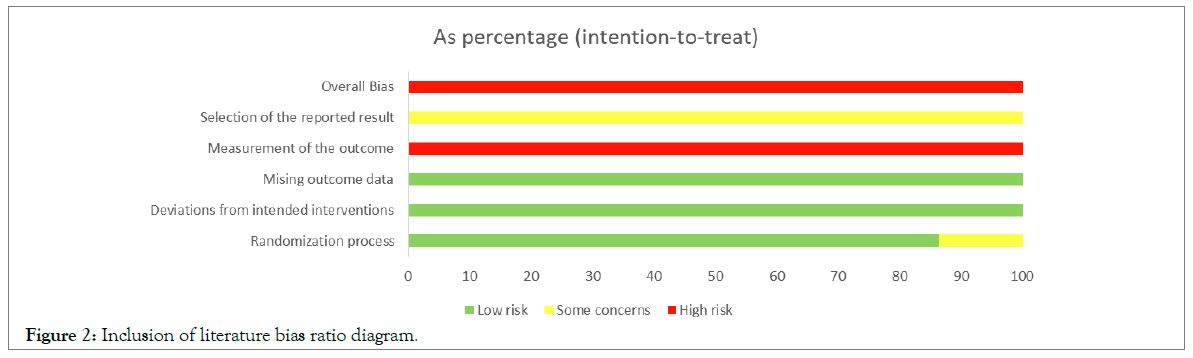
Figure 2: Inclusion of literature bias ratio diagram.
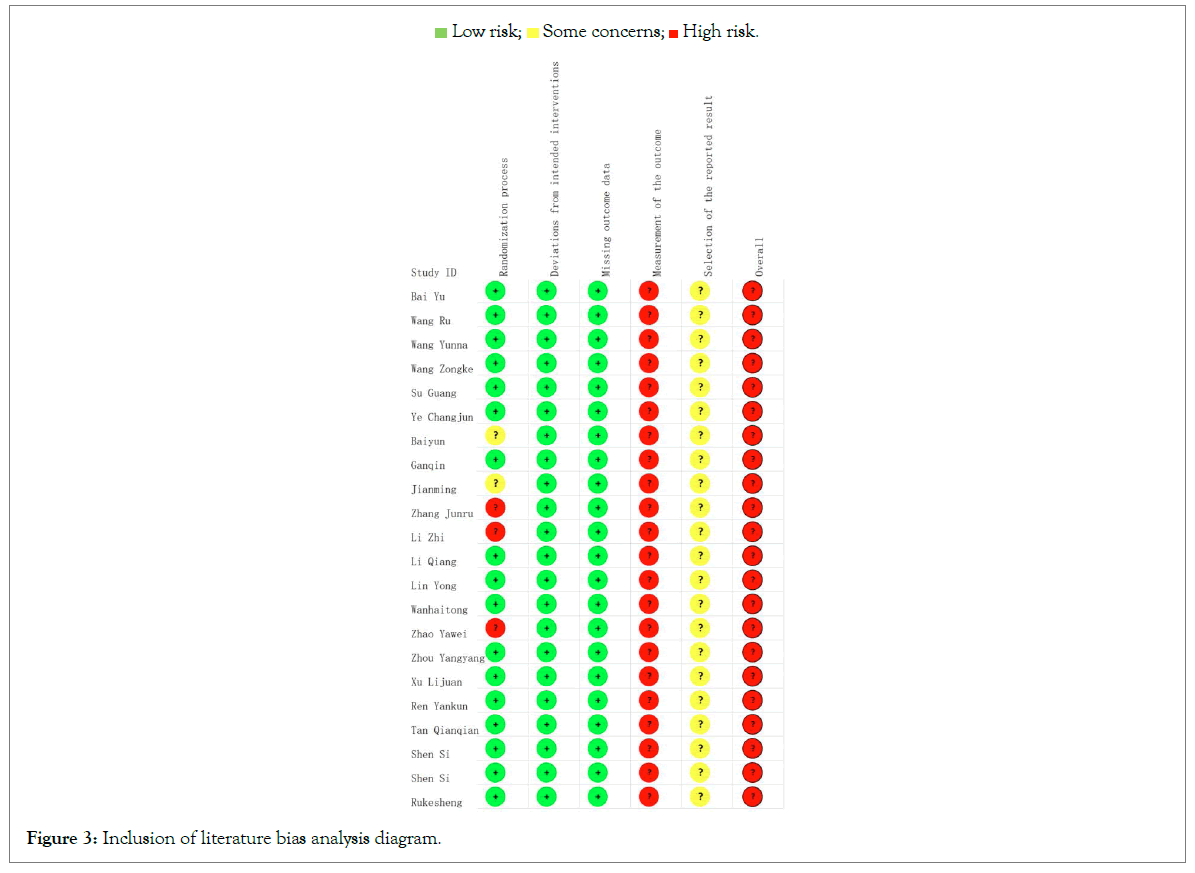
Figure 3: Inclusion of literature bias analysis diagram.
Meta-analysis results
Hamilton Depression (HAMD) rating scale score analysis: A total of 18 studies involving 1368 participants analyzed the HAMD scores for treating Post-Stroke Depression (PSD). Among them, four studies compared the effects of Traditional Chinese Medicine (TCM) treatment versus Western medicine, showing significant heterogeneity (I²=78%, P=0.004). A random-effects model was employed. Figure 4, shows the meta-analysis results indicates the TCM treatment is more effective than Western medicine in treating PSD (OR=-1.94, 95% CI: -3.17 to -0.71).
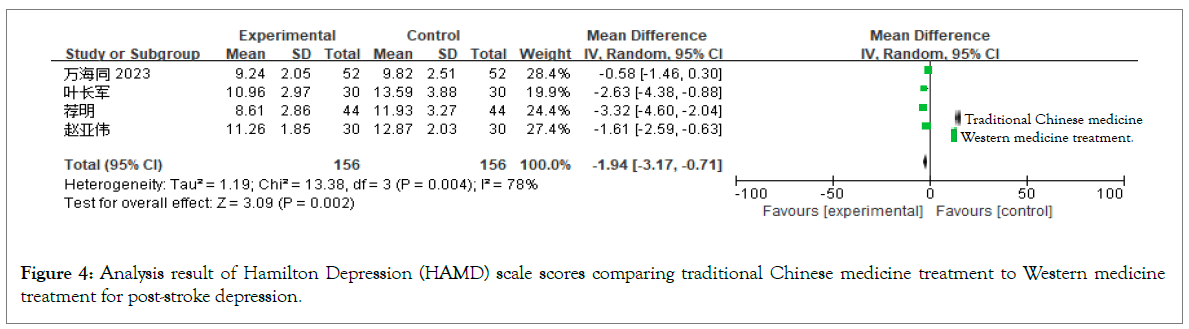
Figure 4: Analysis result of Hamilton Depression (HAMD) scale scores comparing traditional Chinese medicine treatment to Western medicine treatment for post-stroke depression.
Two studies compared the effects of basic treatment versus basic treatment plus TCM, with no significant heterogeneity observed (I²=0%, P=0.48). A fixed-effects model was applied. Figure 5, shows the meta-analysis results demonstrate that basic treatment combined with TCM is more effective than basic treatment alone in treating PSD (OR=-3.35, 95% CI: -4.23 to -2.47).
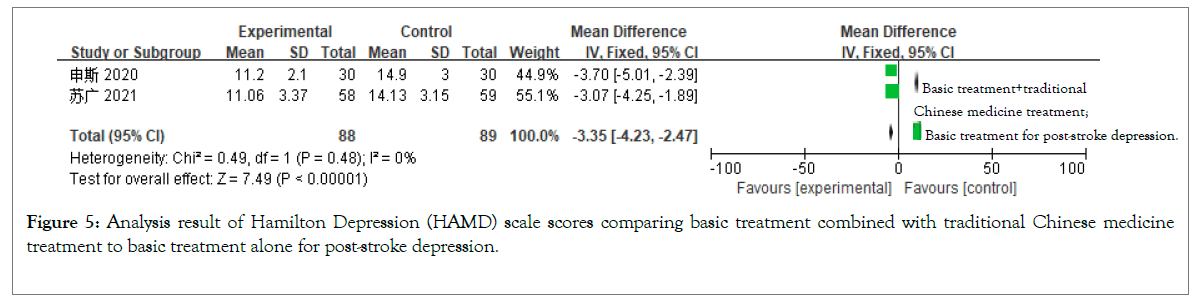
Figure 5: Analysis result of Hamilton Depression (HAMD) scale scores comparing basic treatment combined with traditional Chinese medicine treatment to basic treatment alone for post-stroke depression.
Thirteen studies compared western medicine treatment alone versus combined with TCM, revealing significant heterogeneity (I²=96%, p=0.00001). A random-effects model was used. Figure 6, shows the meta-analysis results show that the combined treatment is more effective than Western medicine alone in treating PSD (OR=-3.29, 95% CI: -4.89 to -1.70).
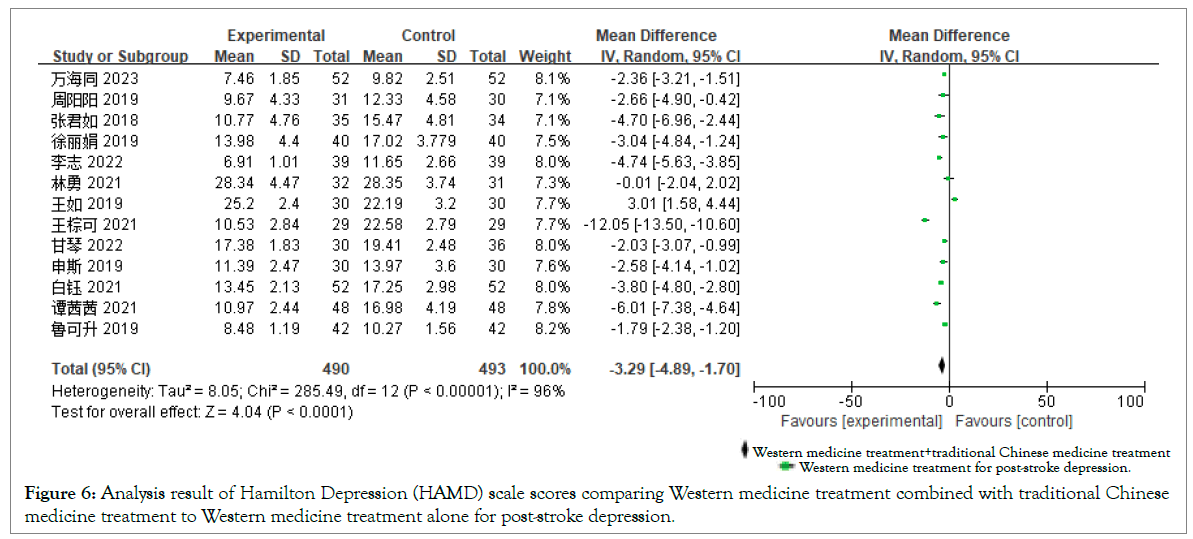
Figure 6: Analysis result of Hamilton Depression (HAMD) scale scores comparing Western medicine treatment combined with traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Self-rating Depression Scale (SDS) score analysis: Four studies with a total of 169 participants analyzed the changes in SDS scores for treating PSD. Two studies compared basic treatment versus basic treatment plus TCM, showing significant heterogeneity (I²=90%, p=0.001). A random-effects model was utilized. Figure 7, shows the meta-analysis results indicate that basic treatment combined with TCM is more effective than basic treatment alone (OR=-8.50, 95% CI: -13.93 to -3.08).
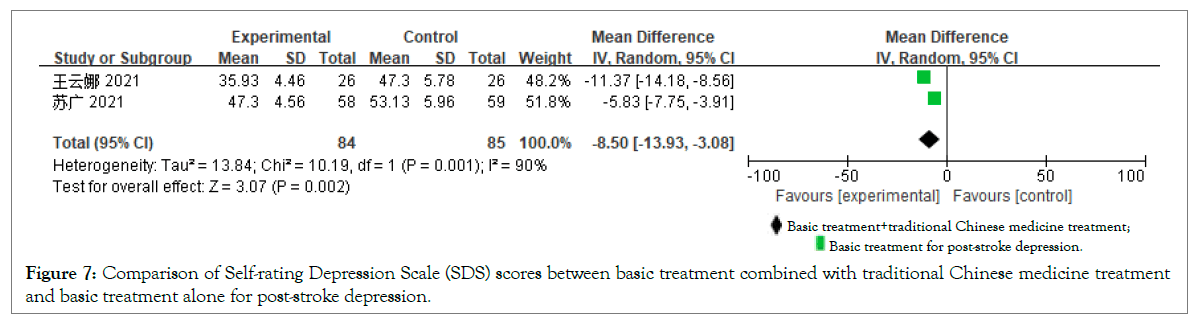
Figure 7: Comparison of Self-rating Depression Scale (SDS) scores between basic treatment combined with traditional Chinese medicine treatment and basic treatment alone for post-stroke depression.
Two studies compared the effects of Western medicine treatment alone versus combined with TCM, revealing moderate heterogeneity (I²=58%, p=0.12). A random-effects model was applied. Figure 8, shows the meta-analysis results demonstrate that the combined treatment is more effective than Western medicine alone (OR=-13.50, 95% CI: -17.16 to -9.84).
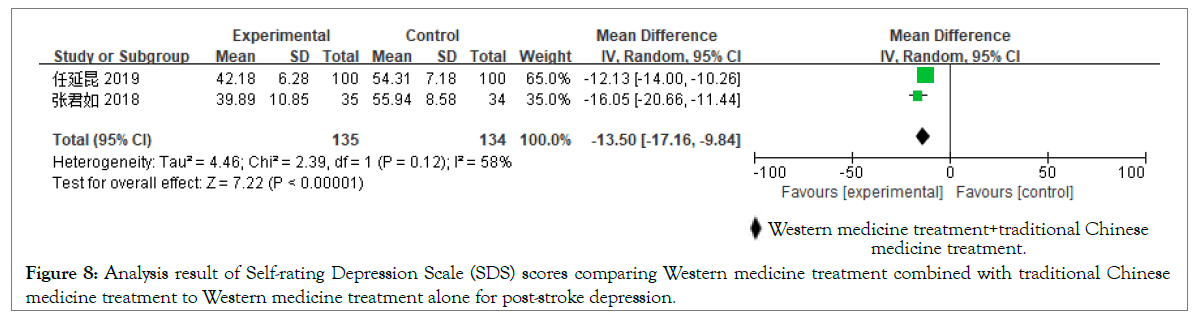
Figure 8: Analysis result of Self-rating Depression Scale (SDS) scores comparing Western medicine treatment combined with traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Clinical efficacy rate based on HAMD score analysis: Eleven studies with a total of 1005 participants analyzed the changes in clinical efficacy rate based on HAMD scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, with no significant heterogeneity observed (I²=0%, p=0.75). A fixed-effects model was employed. Figure 9 shows the meta-analysis results indicate that the combined treatment is more effective than Western medicine alone (OR=2.41, 95% CI: 1.68 to 3.45).
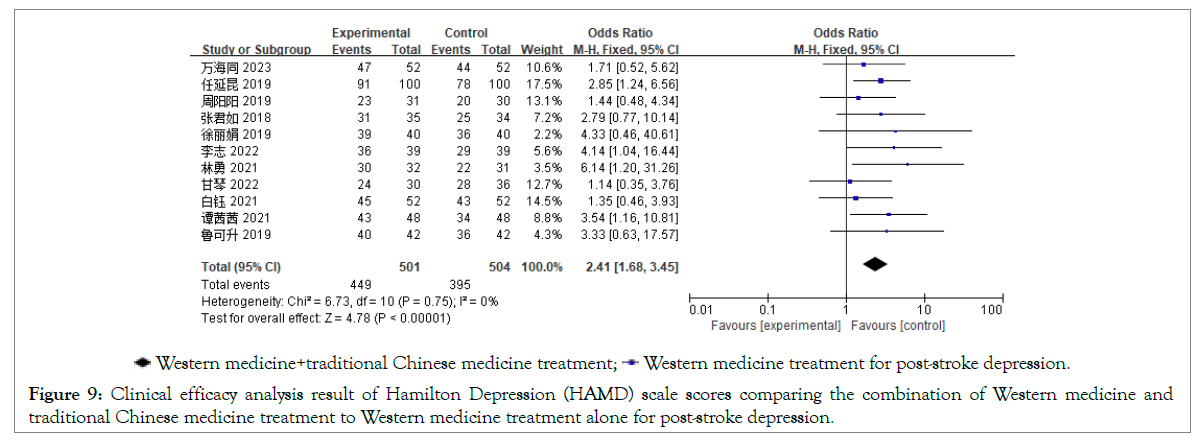
Figure 9: Clinical efficacy analysis result of Hamilton Depression (HAMD) scale scores comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Activities of Daily Living (ADL) score analysis: Five studies with a total of 518 participants analyzed the changes in ADL scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, revealing significant heterogeneity (I²=85%, p=0.0001). A random-effects model was used. Figure 10, shows the meta-analysis results demonstrate that the combined treatment is more effective than Western medicine alone (OR=8.56, 95% CI: 4.76 to 12.37).
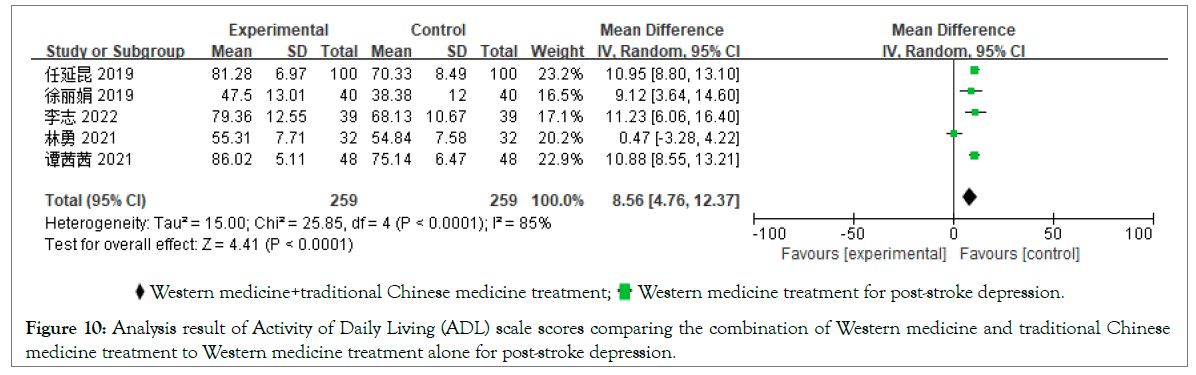
Figure 10: Analysis result of Activity of Daily Living (ADL) scale scores comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
National Institutes of Health Stroke Scale (NIHSS) score analysis: Seven studies with a total of 432 participants analyzed the changes in NIHSS scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, showing significant heterogeneity (I2=95%, p=0.00001). A random-effects model was utilized. Figure 11, shows the meta-analysis results indicate that the combined treatment is more effective than Western medicine alone (OR=-2.42, 95% CI: -3.80 to -1.04).
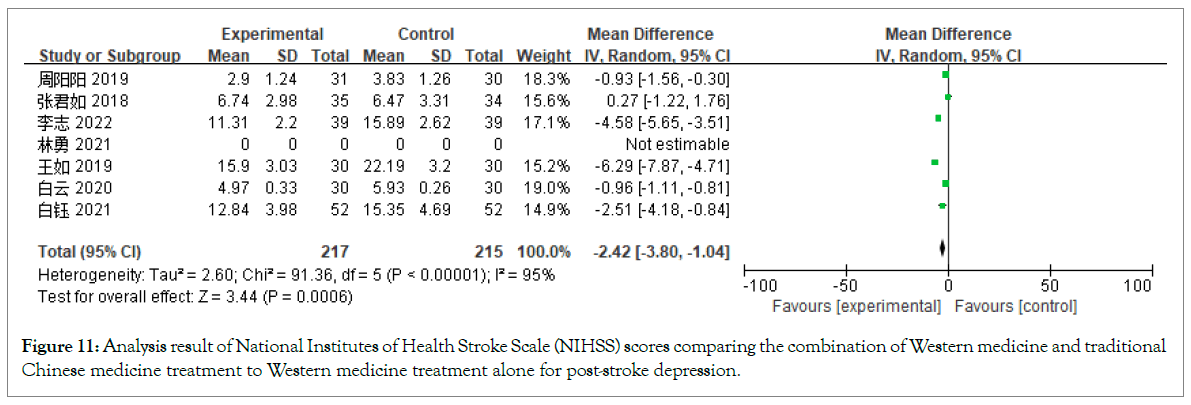
Figure 11: Analysis result of National Institutes of Health Stroke Scale (NIHSS) scores comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Clinical efficacy rate based on TCM syndrome score analysis: Six studies with a total of 424 participants analyzed the clinical efficacy rate based on TCM syndrome scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, revealing mild heterogeneity (I²=39%, p=0.22). A fixed-effects model was applied. Figure 12, shows the meta-analysis results demonstrate that the combined treatment is more effective than Western medicine alone (OR=2.65, 95% CI: 1.68 to 4.20).
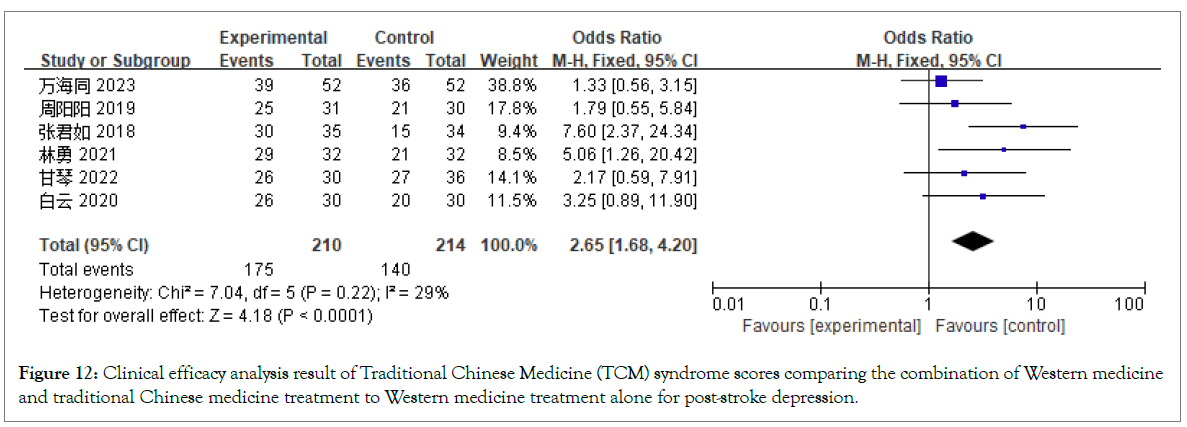
Figure 12: Clinical efficacy analysis result of Traditional Chinese Medicine (TCM) syndrome scores comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
TCM syndrome score analysis: Five studies with a total of 377 participants analyzed the TCM syndrome scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, showing significant heterogeneity (I²=96%, p=0.00001). A random-effects model was employed. Figure 13, shows the meta-analysis results indicate that the combined treatment is more effective than Western medicine alone (OR=-2.13, 95% CI: -2.61 to -1.64).
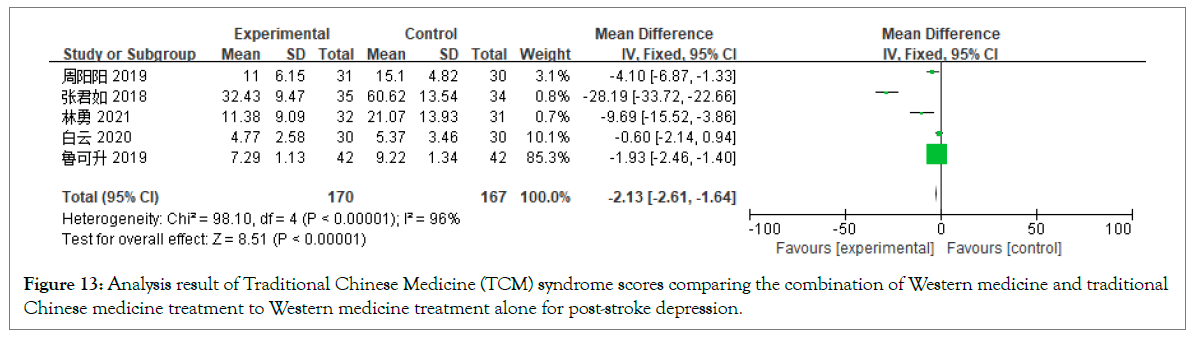
Figure 13: Analysis result of Traditional Chinese Medicine (TCM) syndrome scores comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
5-Hydroxytryptamine (5-HT) level analysis: Two studies with a total of 200 participants analyzed the 5-HT levels for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, revealing significant heterogeneity (I²=88%, p=0.004). A random-effects model was utilized. Figure 14, shows the meta-analysis results demonstrate that the combined treatment is more effective than Western medicine alone (OR=39.10, 95% CI: -5.93 to 84.12).
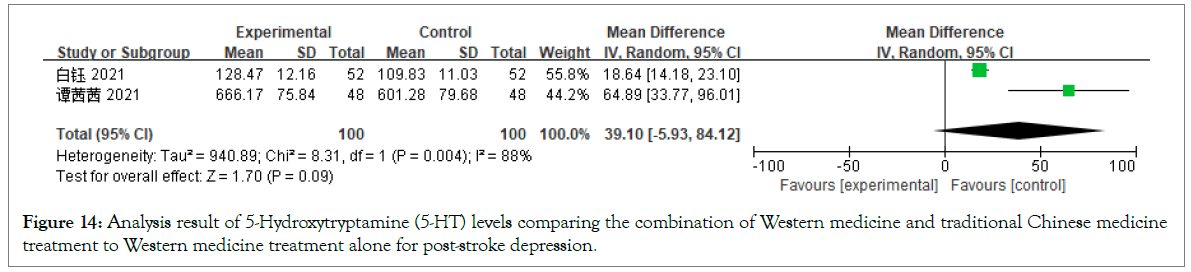
Figure 14: Analysis result of 5-Hydroxytryptamine (5-HT) levels comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Adverse reaction rate analysis: Four studies with a total of 238 participants analyzed the adverse reaction rates for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, showing mild heterogeneity (I²=24%, p=0.27). A fixed-effects model was applied. Figure 15, shows the meta-analysis results indicate that the combined treatment is more effective than Western medicine alone (OR=0.36, 95% CI: 0.15 to 0.85).
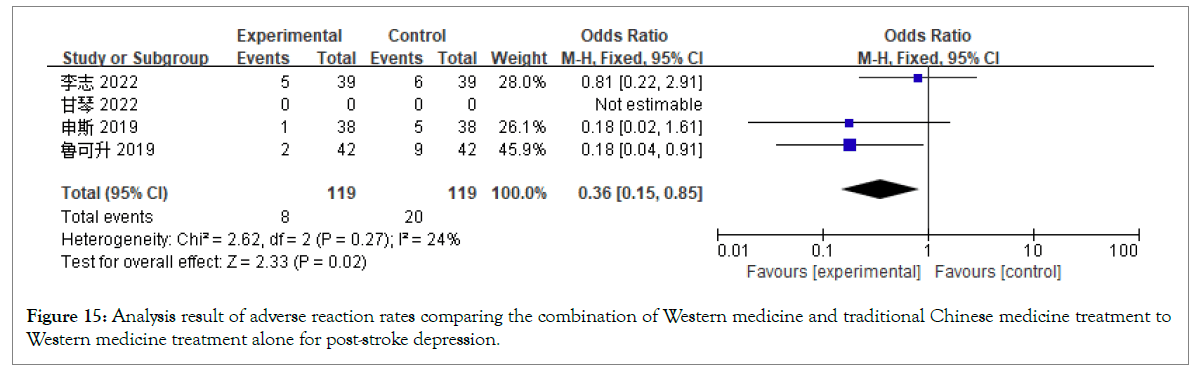
Figure 15: Analysis result of adverse reaction rates comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Barthel Index (BI) score analysis: Three studies with a total of 188 participants analyzed the BI scores for treating PSD. The studies compared Western medicine treatment alone versus combined with TCM, revealing significant heterogeneity (I²=96%, p=0.00001). A random-effects model was used. Figure 16, shows the meta-analysis results demonstrate that the combined treatment is more effective than Western medicine alone (OR=9.20, 95% CI: -3.70 to 22.10).
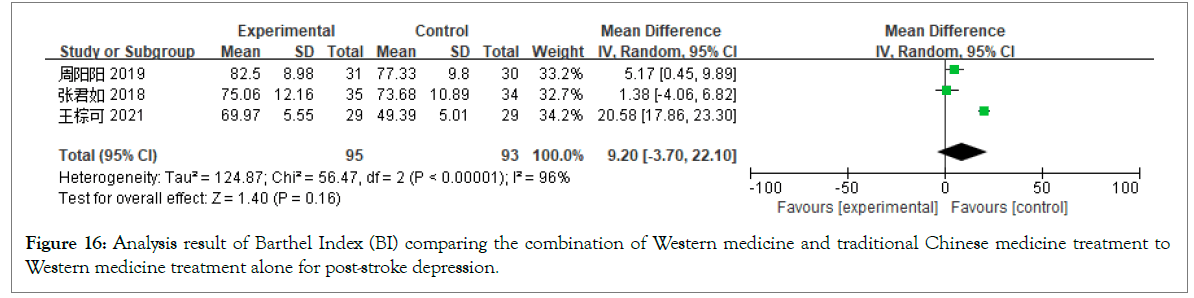
Figure 16: Analysis result of Barthel Index (BI) comparing the combination of Western medicine and traditional Chinese medicine treatment to Western medicine treatment alone for post-stroke depression.
Publication bias analysis: Publication bias analysis was conducted on 12 studies reporting the changes in clinical efficacy rate based on HAMD scores for treating PSD. A funnel plot was constructed using the Standardized Mean Difference (SMD) as the X-axis and the Standard Error (SE) of Standardized Mean Difference (SMD) as the Y-axis. The analysis revealed that most scatter points were located in the upper middle part of the plot, but the symmetry was relatively poor. This suggests potential publication bias in the meta-analysis comparing the treatment of PSD with the clinical efficacy rate changes in HAMD scores between combined TCM and Western medicine and the control group (Figure 17).
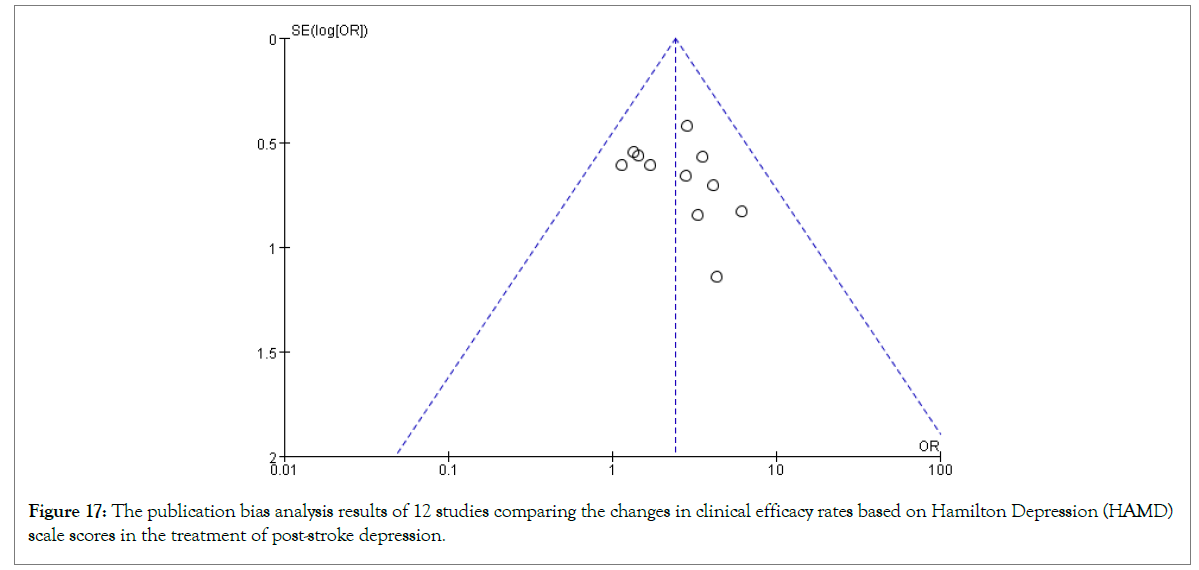
Figure 17: The publication bias analysis results of 12 studies comparing the changes in clinical efficacy rates based on Hamilton Depression (HAMD) scale scores in the treatment of post-stroke depression.
Additionally, publication bias analysis was conducted on 18 studies reporting changes in HAMD scores for treating PSD. A funnel plot was created with SMD as the X-axis and SE(SMD) as the Y-axis, showing a concentrated distribution of scatter points with reasonable symmetry. This suggests a lower likelihood of publication bias in the meta-analysis of changes in PSD HAMD scores (Figure 18).
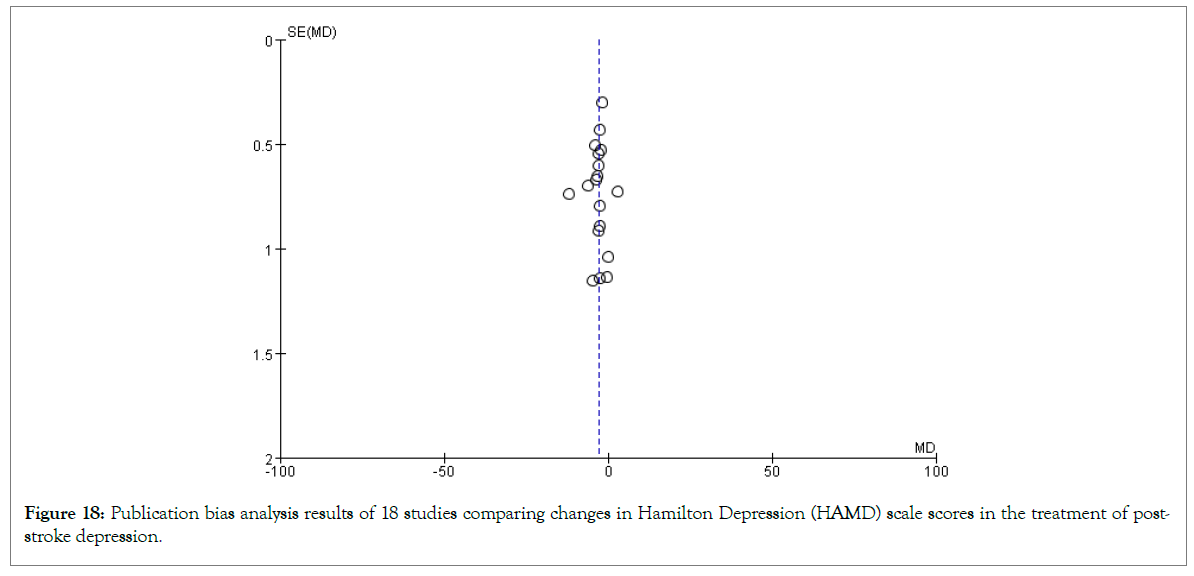
Figure 18: Publication bias analysis results of 18 studies comparing changes in Hamilton Depression (HAMD) scale scores in the treatment of poststroke depression.
Study results
This meta-analysis indicates that Traditional Chinese Medicine (TCM) or the combination of TCM and Western medicine outperforms Western medicine alone in improving HAMD scores, clinical efficacy rates of HAMD scores, TCM syndrome scores, clinical efficacy rates of TCM syndrome scores, SDS scores, ADL scores and BI index scores, with a lower rate of adverse reactions. Notably, the meta-analysis results for HAMD scores, NIHSS scores, ADL scores and TCM syndrome scores show high heterogeneity, thus a random-effects model was employed for analysis, requiring cautious interpretation of the results. Overall, TCM treatment for post-stroke depression significantly improves outcomes with fewer adverse reactions, making it highly recommendable for widespread clinical application.
Significance and prospects
Most TCM practitioners consider post-stroke depression as depression due to illness, with its pathogenesis based on yin-yang imbalance and qi-blood disorder caused by stroke, coupled with emotional disturbances, leading to liver qi stagnation, phlegm and blood stasis and consequently disturbing the heart and brain [37]. In the context of more in-depth research on TCM treatment for post-stroke depression, this study systematically evaluated the clinical efficacy of TCM in treating PSD using modern evidence-based medical methods, providing higher quality evidence for using TCM in treating PSD. The results confirm the positive clinical efficacy and high safety of TCM in treating PSD, offering significant guidance for clinical treatment. With the burgeoning development of TCM, it is increasingly demonstrating its unique advantages in treating post-stroke depression and related diseases. Studies have found that acupuncture can not only alleviate post-stroke limb spasticity by modulating brain plasticity-related signals, thus having therapeutic effects on stroke, but also relieve depressive symptoms by enhancing hippocampal and network neural plasticity and reducing brain inflammation [38,39]. Moreover, it can reduce the occurrence of post-stroke depression by improving post-stroke cognitive impairment [40]. These studies indicate the significant role of acupuncture in treating post-stroke depression and related diseases, suggesting that future research should focus on the combined effects of acupuncture and medication on post-stroke depression, thereby maximizing the unique advantages and value of TCM in treating this condition.
Incorporating the extant literature, it is preliminarily affirmed that Traditional Chinese Medicine (TCM) or the integration of TCM and Western medicine in treating post-stroke depression patients tends to yield superior outcomes compared to sole employment of Western medicinal approaches, thus rendering them potentially viable for clinical deployment. Nevertheless, the imperative remains for rigorous, large-scale randomized controlled trials to validate these findings, thereby furnishing robust theoretical underpinnings for clinical praxis. Within this odyssey towards wellness and remedy, each stride necessitates meticulous observation of nature's cadence, extracting wisdom therefrom to attain heightened levels of comprehension and application. In this realm of inquiry, our understanding of TCM and its amalgamation with Western medicine resonates akin to a panoramic vista of the natural world, demanding continual refinement, enrichment and deepening through novel strokes of insight. Hence, we advocate for increased scholarly engagement to delve further into this domain, furnishing our medical endeavours with ever more dependable support.
This study strictly adhered to meta-analysis standards, yet it possesses certain limitations.
• Only publicly published literature was included, excluding conference papers and others and some literature was omitted due to lack of key data, potentially leading to result bias.
• The quality of included RCT literature varies, with issues in randomization methods and inadequate blinding, possibly affecting result reliability.
• Intervention measures among studies were not entirely consistent, such as varying specific TCM formulations and Western medicine types, contravening clinical trial control consistency and experimental design rigor.
• The duration of included studies varied from 1 to 8 weeks, contradicting clinical trial control consistency and potentially impacting final outcomes.
• Different choices were made in the same efficacy observation across studies, such as variations in HAMD scales (HAMD-17, 20, 24 items, etc.) and specific scoring standards for TCM syndrome scores, requiring validation by further studies with larger sample sizes.
This work was supported by the National Natural Science Foundation of China (No: 82260967), Key Research and Development Plan of Ningxia Hui Autonomous Region (No: 2022BEG02040), Natural Science Foundation of Ningxia Hui Autonomous Region (No: 2022AAC05030), Key Research and Development Plan of Ningxia Hui Autonomous Region (No: 2021BEB04023).
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhou Z, Guo Z, Li M, Kudereti B, Gai X, Wang F, et al. (2024). Efficacy of Traditional Chinese Medicine in the Treatment of Post-Stroke Depression: A Systematic Review and Meta-Analysis. J Dep Anxiety. 13:537.
Received: 01-May-2024, Manuscript No. JDA-24-31305; Editor assigned: 03-May-2024, Pre QC No. JDA-24-31305 (PQ); Reviewed: 17-May-2024, QC No. JDA-24-31305; Revised: 24-May-2024, Manuscript No. JDA-24-31305 (R); Published: 03-Jun-2024 , DOI: 10.35248/2167-1044.24.13.537
Copyright: © 2024 Zhou Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.