Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2020)Volume 9, Issue 4
Background: Pregnancy is one of the most essential experiences in a woman’s life, with unprecedented and crucial biological and emotional changes; 13% of all women’s psychiatric clinic admissions take place during this period. The risk for suicide is increased by 70 times.
Objective: To investigate the psychological changes observed in multiparas, during the postnatal period, that coincided with the pandemic of Coronavirus disease 2019 (COVID-19).
Research Methodology: Our sample constituted 219 low risk multiparous women, who went through the early postnatal period (1st - 3rd day following birth) and used maternity services at central maternity hospitals in Athens, Greece. After 40–60 days, the same questionnaires were redistributed electronically or by post, to investigate the postnatal psychological changes. We used the STAI, EPDS, and a demographic questionnaire. Statistical analysis was performed using the SPSS software.
Results: The mean value of the STAI scale and in particular the S dimension of anxiety state, was estimated at 36.09, with a standard deviation of 8.36. The range of values of the STAI scale, is smaller. The average values of the EPDS scale, for different ages, range between 5 and 8.33, with little variation for ages under 25 years. There is a statistically significant correlation, between the two scales with a Pearson index value of R = 0.700. Finally, there was no statistically significant effect at 95% of any of the demographic characteristics, in both the STAI and EPDS scales.
Conclusion and Recommendations: Our sample’s emotions, are not adversely affected during the postpartum period and rarely experienced, or manifested, self-destructive thoughts or actions, respectively, even when facing a nationwide, COVID-19-related lockdown. For future research, it is recommended to use a larger sample of women, who gave birth during a crisis, for a safer generalization of the findings
Postpartum depression; Postnatal period; Psychological changes; COVID-19 pandemic
Pregnancy is one of the most essential experiences, in a woman's life, involving unprecedented and crucial biological and emotional alterations. Conversely, the post-partum period is characterized by significant mood disorders, with relevant research showing about 13% of all admissions to psychiatric clinics taking place at that point; moreover, women are 70 times more likely to commit suicide during this time [1]. The most common mental disorders that occur during childbirth are postpartum sadness (baby blues), postnatal depression (PND), and postpartum psychosis (PP). Postpartum depression in general, is a type of clinical depression that affects 10%–15% of women, with only one in four cases being diagnosed and treated. PND is one of the most common causes of maternal distress, representing a considerable public health problem that affects the mother, her baby, and her family [2]. Reviews showed that PND prevalence ranged widely, between 0% and 60% globally, with Asian countries showing prevalence between 3.5% and 63.3%. [3,4].
PP is an extremely rare disorder, with an incidence rate of 0.1%– 0.2%, usually occurring between two days and two weeks after delivery. Differentiating between “baby blues,” severe depression, and psychosis is vital. The Diagnostic and Statistical Manual of Mental Disorders, fifth edition, categorizes PND under “depressive disorder with peripartum onset,” which is defined as any time in pregnancy or the first four weeks following delivery [5]. All aforementioned disorders constitute both a substantial and a direct impact, not only on the child, regardless of her/his age, but on family cohesion as well [6].
Research, regarding the perinatal mental disorder field has recently attracted attention. According to Greece’s existing epidemiological data, 50%–85%, 10%–15%, and 0.1%–0.2% of new mothers develop a mild and transient form of postpartum sadness (baby blues), PND, and PP, respectively [7]; these data are consistent with the existing literature.
Research shows, that increased rates of postpartum depression (PND), occur when the new mother does not receive expected domestic and social support [8-11]. In some women, social support, the relationship with their partner, and self-esteem during pregnancy and childbirth, are variables closely related to postpartum depression [12,13]; moreover, low self-esteem, is another sensitive factor regarding the manifestation of depressive symptoms, even in women with no such history [12].
Individual and family psychiatric history [8], routine stress deriving from unemployment or vocational insecurity [14,15], and stressful and anxiety-triggering life-events [14,16], additionally contribute to the development of childbirth-related mental disorders. Research has also shown, that the new mother's mental health, is affected by stress during pregnancy [10], postpartum sadness [14], multiparity and unplanned or unwanted pregnancy [15], the birth of a difficult infant (infant temperament), and/or an infant with neonatal complications [8,10]. Moreover, birth complications and a low degree of satisfaction, regarding health services during childbirth [17], a bad childhood relationship, between the postpartum woman and her mother [8,9,15], the absence of the mother due to death or a dysfunctional parental context [8], and intimate partner abuse before and/or during pregnancy [16,18] are additional factors, that affect the new mother during the postpartum period. Conversely, the mother's age, profession, previous miscarriages or abortions, the type of birth, and the baby's sex, do not significantly contribute to the occurrence of mental disorders, during the postpartum period [8,11].
This research aimed to (a) investigate the psychological changes observed in multiparous women during the postnatal period, especially during the Coronavirus disease outbreak (COVID-19), and (b) raise the health professionals' awareness regarding the difficulties that occur during this period.
The sample constituted 219 low risk, multiparous women, who were extremely fluent in reading and writing Greek during the early stage of the postnatal period (between the 1st and 3rd day postpartum), gave birth to full term, healthy neonates and were using maternal services of central maternity hospitals of Athens, Greece. All questionnaires were personally administered by the researcher and data were collected between December 2019 and February 2020. The participants were informed regarding the research and provided written informed consent; furthermore, all questionnaires were anonymously completed.
Between 40 and 60 days later, the same participants were readministered the same questionnaires, either electronically or by traditional mail, due to the COVID-19 lockdown situation. They were informed of the re-administration either by phone or by electronic mail.
The questionnaires constituted three parts; the first part pertained to the demographics of each participant; the second part comprised 20 STAI scale questions [19,20], namely the scale assessing the anxiety state; and the third part included 10 EPDS scale questions[21,22], namely the scale assessing depression. Statistical analysis was carried out using the SPSS software (Armonk, NY, USA) following an appropriate questionnaire codification, which was developed specifically to this end. The Pearson correlation coefficient was used to correlate the STAI and EPDS scales, while an analysis of variance and a T-test for independent samples were employed to assess the effect of the individual STAI and EPDS characteristics. Finally, we calculated Cronbach's α index for the STAI and EPDS scales to measure internal consistency, with an acceptable rate of 0.882 and 0.833, respectively.
The sample's descriptive statistical measures, including family income, age, marital status, number of children, educational level, and the participants' and husbands' profession are all illustrated in Table 1.
| Variables | Category | Frequency (f) | Total percentage (%) | Response percentage (Valid percent) |
|---|---|---|---|---|
| Family income | €500–€1000 | 4 | 1,40 | 4,60 |
| €1000–€2000 | 36 | 12,30 | 41,40 | |
| €2000–€3000 | 25 | 8,60 | 28,70 | |
| >€3000 | 22 | 7,50 | 25,30 | |
| Age | <25 years old | 7 | 2,40 | 2,90 |
| 26-30 years old | 36 | 12,30 | 14,80 | |
| 31-35 years old | 109 | 37,30 | 44,90 | |
| 36-40 years old | 68 | 23,30 | 28,00 | |
| >40 years old | 23 | 7,90 | 9,50 | |
| Marital Status | Married | 100 | 34,20 | 84,70 |
| Divorced | 8 | 2,70 | 6,80 | |
| Civil Partnership | 5 | 1,70 | 4,20 | |
| Single | 5 | 1,70 | 4,20 | |
| Children | 1 Child | 54 | 18,50 | 45,80 |
| 2 Children | 55 | 18,80 | 46,60 | |
| 3 Children | 9 | 3,10 | 7,60 | |
| Educational level | Junior high school | 3 | 1,00 | 2,50 |
| High school | 20 | 6,80 | 16,90 | |
| University/College | 66 | 22,60 | 55,90 | |
| Postgraduate degree | 23 | 7,90 | 19,50 | |
| PhD | 6 | 2,10 | 5,10 | |
| Profession | Private sector | 43 | 14,70 | 36,40 |
| Public Sector | 22 | 7,50 | 18,60 | |
| Freelance | 30 | 10,30 | 25,40 | |
| Unemployed | 12 | 4,10 | 10,20 | |
| Other | 11 | 3,80 | 9,30 | |
| Husband's profession | Private sector | 44 | 15,10 | 37,30 |
| Public sector | 30 | 10,30 | 25,40 | |
| Freelance | 40 | 13,70 | 33,90 | |
| Unemployed | 4 | 1,40 | 3,40 | |
| Husband's educational level | Junior high school | 2 | 0,70 | 2,30 |
| High school | 23 | 7,90 | 26,40 | |
| University/College | 42 | 14,40 | 48,30 | |
| Postgraduate degree | 18 | 6,20 | 20,70 | |
| PhD | 2 | 0,70 | 2,30 |
Table 1: Absolute and relative frequencies for the sample's demographic characteristics.
The S dimension of the STAI scale levels (Table 2), which pertains to the state of anxiety derived by the status quo and not by a personality trait, the average values, and standard deviations were calculated, both for several age groups and the whole sample.
| Means, Standard Deviations, and Alpha Coefficients for Working Adults in Three Age Groups | ||||||
| Variables | Ages 19-39 | Ages 40-49 | Ages 50-69 | |||
| M | F | M | F | M | F | |
| 446 | 210 | 559 | 135 | 382 | 382 | |
| S-Anxiety | ||||||
| Mean | 36.54 | 36.17 | 35.88 | 36.03 | 34.51 | 32.2 |
| SD | 10.22 | 10.96 | 10.52 | 11.07 | 10.34 | 8.67 |
| Alpha | 0.92 | 0.93 | 0.93 | 0.94 | 0.92 | 0.9 |
| T-Anxiety | ||||||
| Mean | 35.55 | 36.15 | 35.06 | 35.03 | 33.86 | 31.79 |
| SD | 9.76 | 9.53 | 8.88 | 9.31 | 8.86 | 7.78 |
| Alpha | 0.92 | 0.92 | 0.91 | 0.92 | 0.96 | 0.89 |
Table 2: Spielberger et al.'s indicative values of the STAI scale for the state dimension.
The identified variation pertains to the fluctuation noted in this study's sample. Specifically, based on Spielberg's research, the variations range between 8 and 11, while the present research's variations range between 3 and 9; therefore, the range in which the STAI scale's values are placed is smaller for our research, while the stress levels for participants under 25 years of age, show a significantly lower variation. Assessing the sample's overall stress levels showed that, on average, they have the values of the normal population, in line with Spielberger et al's, research (Table 3 and Figure 1).
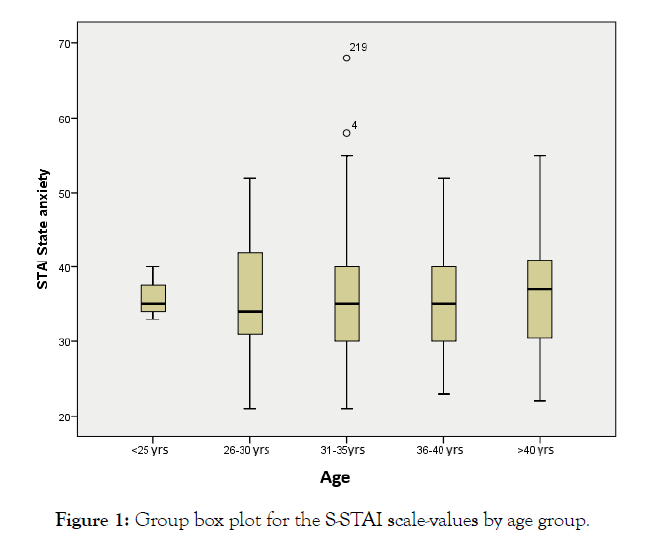
Figure 1: Group box plot for the S-STAI scale-values by age group.
| Age group | N | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| <25 years old | 3 | 36,00 | 3,61 | 33,00 | 40,00 |
| 26-30 years old | 25 | 35,48 | 8,35 | 21,00 | 52,00 |
| 31-35 years old | 81 | 36,22 | 8,84 | 21,00 | 68,00 |
| 36-40 years old | 43 | 36,02 | 7,61 | 23,00 | 52,00 |
| >40 years old | 19 | 36,53 | 9,09 | 22,00 | 55,00 |
| Total | 171 | 36,09 | 8,36 | 21,00 | 68,00 |
Table 3: Mean values and standard deviations of the S-STAI scale by age group for the women in the sample.
Regarding the average values of the EPDS scale for several ages, they vary between 5 and 8.33, with a small scale-fluctuation for ages <25 years, which was also identified as a characteristic for the STAI scale; a significant deviation of the EPDS scale for larger age-groups, with a peak for ages >40 years, was also identified. The EPDS-interpretation variable was identified as well, namely a categorization of the sample regarding the EPDS-scale values, exactly as it is recommended by the EPDS scoring guide (2015).
Applying this directive to the sample, 70.3% is classified in the "unlikely occurrence of depression" category; 14.2% in the "depression possible" category (i.e., there is a possibility of depression); 6.4% in the "fairly high possibility of depression" category (i.e., in the rather high probability of depression); and 9.1% in the “most likely to be depressed” category. All classifications’ results are shown in Table 4 and Figure 2; moreover, always according to the directives, the suicide risk index showed that 95.89% of the sample has no probability or no risk for suicide; however, 4.11% note either a small or large chance of suicide (Tables 5 and 6 and Figures 3 and 4).
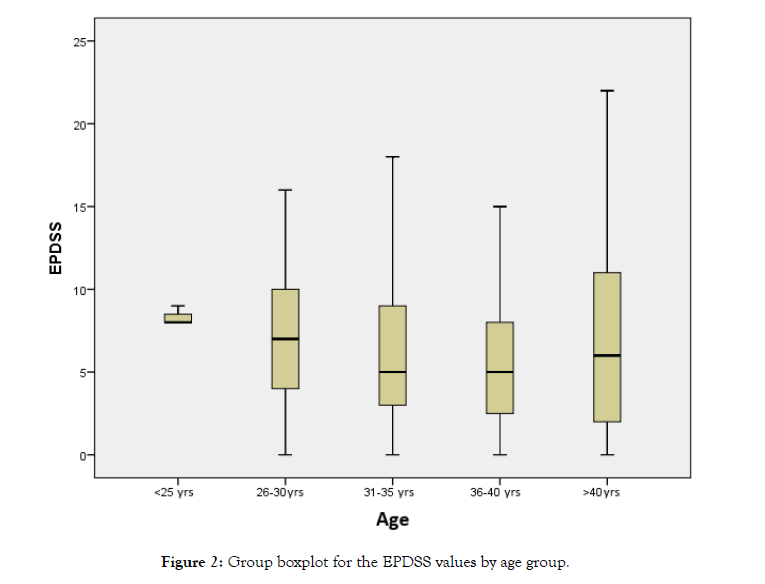
Figure 2: Group boxplot for the EPDSS values by age group.
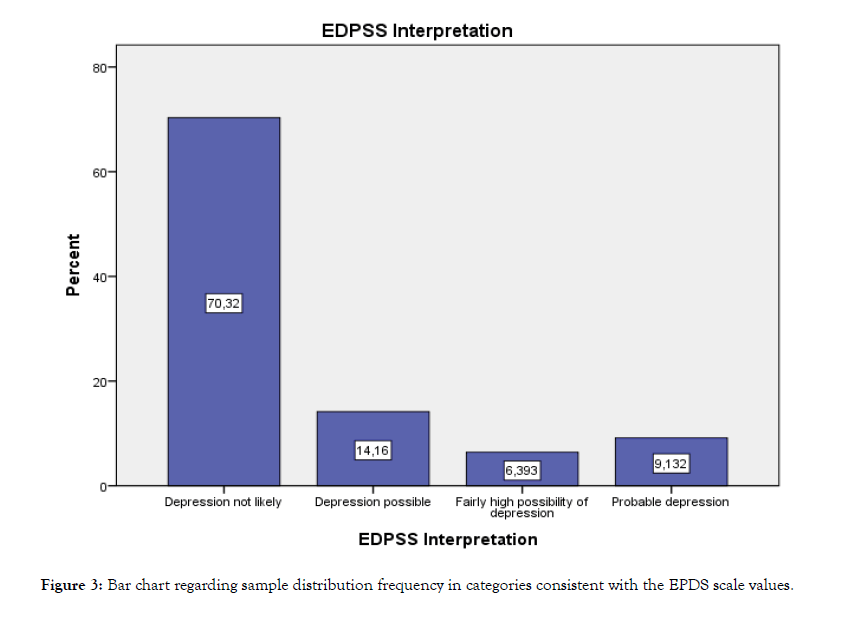
Figure 3: Bar chart regarding sample distribution frequency in categories consistent with the EPDS scale values.
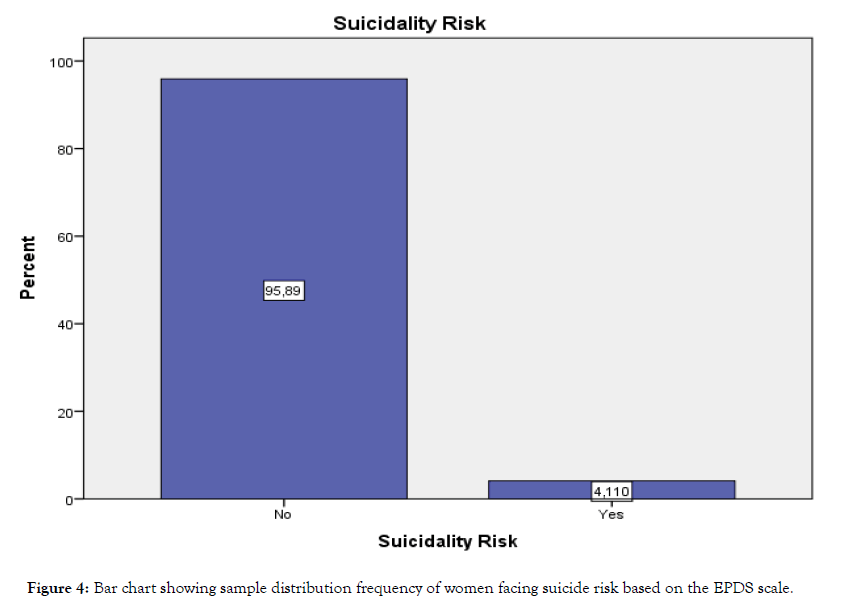
Figure 4: Bar chart showing sample distribution frequency of women facing suicide risk based on the EPDS scale.
| Age group | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|
| <25 years old | 8,33 | 0,58 | 8,00 | 9,00 |
| 26-30 years old | 6,84 | 4,38 | 0,00 | 16,00 |
| 31-35 years old | 6,32 | 4,59 | 0,00 | 18,00 |
| 36-40 years old | 5,49 | 3,80 | 0,00 | 15,00 |
| >40 years old | 7,16 | 6,34 | 0,00 | 22,00 |
| Total | 6,32 | 4,56 | 0,00 | 22,00 |
Table 4: Mean values and standard deviations of the S-STAI scale by age group of the sample.
| Variables | Frequency | Percentage |
|---|---|---|
| Depression not likely | 154 | 70.3 |
| Depression possible | 31 | 14.2 |
| Fairly high possibility of depression | 14 | 6.4 |
| Probable depression | 20 | 9.1 |
| Total | 219 | 100.0 |
Table 5: Absolute and relative frequencies regarding sample distribution in categories consistent with EPDS scale-values.
| Suicide Risk | ||
|---|---|---|
| Variables | Frequency | Percentage |
| No | 210 | 95.9 |
| Yes | 9 | 4.1 |
| Total | 219 | 100.0 |
Table 6: Absolute and relative frequencies regarding the sample distribution of women facing suicide risk based on the EPDS scale.
We used the Pearson correlation coefficient to calculate the
association between the EPDS and STAI scales, producing a
statistically significant p-value of 0.01, with an R=0.700 Pearson
value; its correlational value is shown in Table 7 and Figure 5. 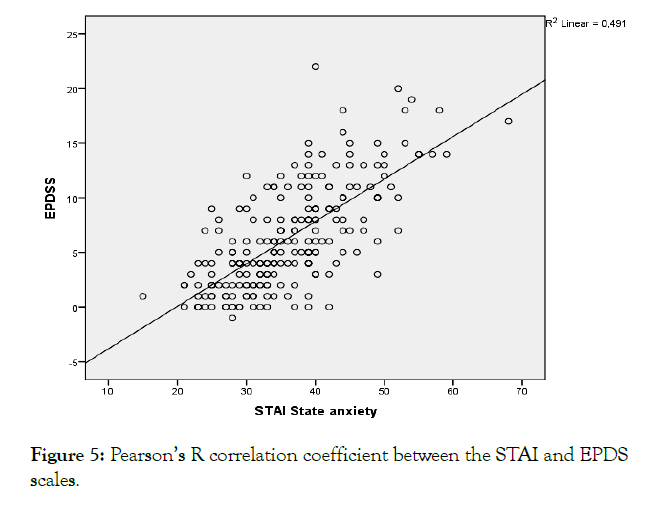
Figure 5: Pearson’s R correlation coefficient between the STAI and EPDS scales.
| Correlations | STAI State anxiety | |
|---|---|---|
| EPDSS | Pearson Correlation | 0.700** |
| Sig. (2-tailed) | 0.000 | |
| N | 219 | |
**. Correlation is significant at the 0.01 level (2-tailed).
Table 7: Pearson’s R-correlation coefficient between the STAI and EPDS scales.
This potentially translates as a positive and statistically significant correlation, indicating that high values can lead to high depression scores and vice-versa.As shown in the scatter plot, there is good fitting around the points in the correlational line's area, with a 0.49 R2 linear indicator value.
The R2 is the index of the regression model's good fit, which is executed to alternately calculate the two variables' correlation. In conclusion, the literature findings are confirmed, with a positive correlation between the scales of stress and depression.
Finally, no statistically significant effect was found at 95% of any of the demographic characteristics regarding the STAI and EPDS scales, meaning that the sample behaves consistently, regardless of the individual or family characteristics, examined in this study.
The transition to parenthood represents a major life change, with a considerable socioemotional and physical, daily functioning impact [23]. The incidence of mental health problems rises substantially in child-rearing years, particularly for females, but it is unclear whether the number of children, is important.
Our results showed, that a large percentage of the sample's feelings, are not negatively influenced, during the post-partum period. Most of the participants responded well, to various hardships, did not illustrate any fear or panic, and did not face any problems, related to their increased duties, due to motherhood. An important finding is, that they rarely developed or expressed, self-harming thoughts or behaviors, respectively. The fact that the majority of the sample, were already mothers, or were about to give birth for the second or third time, could justify their smooth transition to the motherly role, despite the unprecedented nature of the pandemic and related home restrictions. Previous cross-sectional research, has linked multiparity with an elevated risk of maternal mental health problems with, however, inconsistent evidence [24,25]. It is also unclear, whether this risk is due to the characteristics of mothers, who have multiple children, or an increased mental health risk, as a consequence, of having multiple children. Even though our participants, were not feeling entirely rested, calm, relaxed, and/ or focused, they did not characterize their everyday hardships, as insurmountable. If any risk, is associated with the life-changing impact of parenthood per se, the number of children might not be influential and the risk will be manifested, when both women and men, make the transition from non-parenthood, to parenthood.
According to a previous Greek study, with a sample of women during the prenatal period, their emotional wellbeing, influences the prevalence of postpartum depression [26]. Moreover, the Greek pregnant women's concerns, refer to the child's health, birth, and general financial problems. The prevalence of anxiety and depressive symptoms during pregnancy, render the aspect of early detection, as significantly critical [27].
The COVID-19 outbreak, which was first reported in China, has turned into a global-scale, health-threatening pandemic, thereby prompting the concentration of future studies and clinical trials, on treating and preventing the disease. So far, research data that illustrate the psychological effects of the pandemic, especially, the levels of depression and anxiety of pregnant women, is lacking. Current research focuses on treating and preventing COVID-19, given its mortality rate, and only three studies, have investigated its psychological effects, on the general population [28], pregnant women [29], and health workers [30].
To enable a safer generalization of the conclusions, for women going through the postnatal period, it is proposed to extend related research to other Greek maternity clinics, both private and public, as well as to a larger population of primiparas, especially amid a crisis, such as the COVID-19 pandemic. Our research, points to an urgent need to provide evidence-based data, on psychosocial support, to this vulnerable population, during and after the COVID-19 pandemic; otherwise, adverse events may occur, during such this crucial and life-changing period.
The quantitative data, used to support the findings of this study, are included within the article. All data, used to support the findings of this research, are restricted by the IASO Scientific Board & Uni.W.A. Ethics Committee, in order to protect patient privacy. Data are available from Antigoni Sarantaki, [email address: esarantaki@uniwa.gr], for researchers who meet the criteria for access, to confidential data.
The authors declare no conflict of interest.
The publication charges of this article were funded by the University of West Attica.
We would like to thank Dimitris Karonis for assisting with the translating and formatting process of this manuscript.
Citation: Sarantaki A, Tsouskala E, Gourountu K, Varnakioti D, Lykeriduo-Avramioti A (2020) Emotional Changes of Postpartum Women in Greece - A Preliminary Study during the COVID-19 Pandemic. J Depress Anxiety. 9:371. doi: 10.35248/2167-1044.20.9.371
Received: 12-Aug-2020 Accepted: 08-Sep-2020 Published: 15-Sep-2020 , DOI: 10.35248/2167-1044.20.9.371
Copyright: © 2020 Sarantaki A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : The publication charges of this article were funded by the University of West Attica.