Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2023)Volume 11, Issue 2
The aim of this study was to isolate, characterize and identify Pseudomonas aeruginosa from hospital fomites. A total of fifty samples were collected from door knobs/handles (10), stethoscopes (10), hospital rails (10), patient beddings (10) and sphygmomanometer (10) using sterile swab sticks at the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-ife, Osun-state. Samples were cultured on cetrimide agar and incubated at 37°C for 24 hrs. Pseudomonas aeruginosa were isolated and identified based on growth on cetrimide agar, gram’s reaction, and positive results for catalase, oxidase, citrate, Triple Sugar Iron (TSI), mannitol fermentation test and negative results for MRVP.
Eight Pseudomonas aeruginosa isolates were recovered out of sixteen presumptive Pseudomonads based on positive results on cetrimide agar. These comprised 3(37.5%) from door knobs/handles, 2 (25%) from stethoscopes, 2 (25%) from sphygmomanometer and 1 (12.5%) from hospital rails. Most of the Pseudomonas aeruginosa isolates were from door knobs/handles. The antibiotic susceptibility testing showed that all the 8(100%) isolates were 100% resistant to Chloramphenicol (CH), Amoxicillin (AM), Streptomycin (S) and Septrin (SXT). About 62.5% were resistant to Augmentin (AU) and 75% were resistant to Gentamycin (CN); and 62.5% susceptible to Sparfloxacin (SP) and Tarivid (OFX) and 75% susceptible to Ciprofloxacin (CPX) and Pefloxacin (PEF). Good hygiene methods are highly encouraged among health personnel to avoid cross-contamination on medical facilities.
Pseudomonas aeroginosa; Infections; Antibiotic resistant; Fomites; Antibiotics
Pseudomonas aeruginosa is a non-fermentative gram negative bacteria widely distributed in nature and can survive on a wide variety of surfaces and in hospital environment, as the wards encourage bacterial growth. The organism is able to multiply in various water sources such as seawater, rivers water and even bottled water. It is a gram-negative aerobic bacillus which belongs to the Pseudomonadaceae family. It is a small microorganism, straight or slightly curved non-fermenting glucose and not speculated. It has motility due to a single polar flagellum and twitching. An alarming increase in the prevalence of Multidrug- Resistant Pseudomonas aeruginosa (MDRPA) from 36 to 52 % was reported in an Egyptian study. In studies done in Pakistan and Iran, 29 and 30 % MDR phenotype was reported respectively. In addition to, it’s highly resistance to several antibiotics and disinfectants [1-6].
Epidemiologically, it is ranked as the fourth cause of nosocomial infections that accounts for 10% of all nosocomial infection in the United States. Overall prevalence in US hospital was approximately 4 per 1000 discharge and leading cause of high morbidity and mortality. A study developed in a hospital in Rome, Italy revealed the first case of Multidrug-Resistant Pseudomonas aeruginosa (MDRPA) infection in a haematologic patient in 1992. After that, the prevalence of MDRPA increased from 8% in 1993 to 17% in 1999, related to that hospital. Of 358 cases of bloodstream infections due to Pseudomonas aeruginosa, 14% (51 cases) were caused by strains of MDRPA. In these cases, 96% (46 infections) were nosocomial. The overall mortality rate due to P. aeruginosa infection is greater than 20%, which increases when the infection is due to MDRPA strains [7-9].
Pseudomonas aeruginosa have been isolated from adult bacterial meningitis with underlying disease in Tokyo, Japan, a tertiary care teaching hospital, India, a 5 years surveillance of wound infections in Okada, Edo State, from ear, nose and throat among patients attending Aminu Kano teaching hospital, Nigeria, a tertiary care hospital of Jhalawar district, India and sinks in the patient rooms and a retrospective case-control study in Germany. In addition, studies on the influence of hospital waste water discharge and its potential microbial hazards have been investigated in Brazil, and increasing frequency of Pseudomonas aeruginosa infections in Turkey was also investigated [10-15].
In this study, we investigated Pseudomonas aeruginosa associated with the Hospital fomite at Ile-Ife, Osun state, Nigeria and the susceptibility pattern of the isolates recovered.
Swab samples were collected from various patient wards of the Obafemi Awolowo University Teaching Hospital Complex (OAUTHC), Ile-Ife Osun state, Nigeria (Figure 1).
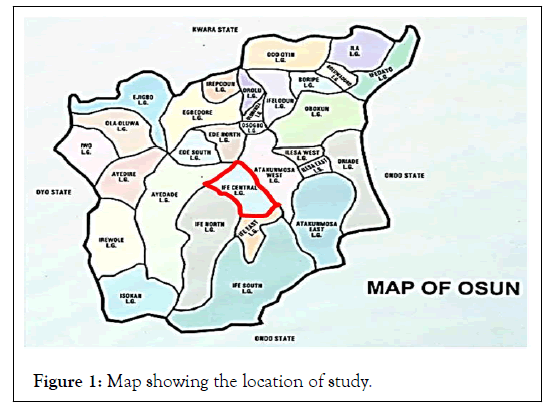
Figure 1: Map showing the location of study.
Collection of samples
Fifty (50) samples from different fomite sources were collected in the morning before commencement of work in the hospital. These were collected from patient’s bedding (10), stethoscopes (10), door knobs/handles (10), hospital rails (10) and sphygmomanometer (10), using sterile swab sticks wetted with sterile peptone water and later transported to the microbiology laboratory, Obafemi Awolowo University (OAU), Ile-Ife, Nigeria.
Isolation, identification and characterization
Each sample swab was inoculated into prepared sterile nutrient broth (Oxoid, UK) and incubated at 37°C for 24 hrs for enrichment. Loopful from the nutrient broth was streaked on freshly prepared plates of nutrient agar and incubated at 37°C for 18 hrs-24 hrs. Discrete colonies were later sub-cultured on a solid selective media; Pseudomonas cetrimide selective agar. All the plates were incubated at 37°C for 24 hrs. Gram staining; morphological identification, catalase and coagulase tests, sugar fermentation analysis and antimicrobial susceptibility trends of the isolate were conducted.
The isolates from hospital fomite: analyzed shown 16 specimens (isolate codes DH3a, DH6a, HR6a, HR10a, PB4a, PB5b, SPG1a, SPG2a, SPG5a, SPG5b, ST1a, ST1b, ST2a, ST6a and ST9a) produced green colonies on cetrimide agar, a characteristic positive result presumptive of Pseudomonas aeruginosa. Five (5) of these isolates were obtained from stethoscope while 4, 3, 2 and 2 isolates were retrieved from sphygmomanometer, door knobs, hospital rails and patients beddings respectively (Tables 1-3).
| Patient Beddings (PB) | Hospital Rails (HR) | Stethoscopes (ST) | Sphygmomanometer (SPG) | Door Knobs/Handles (DH) | Total 50 (100%) | |
|---|---|---|---|---|---|---|
| Number of swab collected | 10 | 10 | 10 | 10 | 10 | 50 |
| Occurrence of Pseudomonas aeruginosa | 0 | 1 | 2 | 2 | 3 | 8 |
| % distribution on each fomites | 0% | 2% | 4% | 4% | 6% | 16% |
Table 1: Occurrence/distribution of Pseudomonas aeruginosa in hospital fomites.
| Isolate code | Gram staining | catalase | Oxidase | Citrate | TSI | Mannitol fermentation | MR | VP | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Glucose | lactose | H2S | Gas | ||||||||
| DH1a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| DH3a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| DH6a | _ | + | + | + | _ | + | + | _ | + | + | _ |
| HR6a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| HR10a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| PB4a | _ | + | + | + | _ | + | + | _ | + | _ | _ |
| PB5b | _ | + | + | + | + | _ | + | + | + | _ | _ |
| SPG1a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| SPG2a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| SPG5a | _ | + | + | + | _ | _ | _ | _ | _ | + | + |
| SPG5b | _ | + | + | + | + | _ | + | + | + | _ | _ |
| ST1a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| ST1b | _ | + | + | + | _ | + | + | _ | + | _ | _ |
| ST2a | _ | + | + | + | _ | + | + | _ | + | + | _ |
| ST6a | _ | + | + | + | _ | _ | _ | _ | + | _ | _ |
| ST9a | _ | + | + | + | _ | _ | _ | _ | + | _ | + |
Note: DH1a: Door Handles/knobs 1a; DH3a: Door Handles/knobs 3a; DH6a: Door Handles/knobs 6a; HR6a: Hospital Rails 6a; HR10a: Hospital Rails 10a; PB4a: Patients Beddings 4a; PB5b: Patients Beddings 5b; SPG1a: Sphygmomanometers 1a; SPG2a: Sphygmomanometers 2a; SPG5a: Sphygmomanometers 5a; SPG5b: Sphygmomanometers 5b; ST1a: Stethoscopes 1a;ST1b: Stethoscopes 1b; ST2a: Stethoscopes 2a; ST6a: Stethoscopes 6a; ST9a: Stethoscopes 9a
Table 2: Biochemical characteristics of positive isolates.
| Antibiotic discs with potency | Number of isolates screened | Susceptibility S (%) | Intermediate I (%) | Resistant R (%) |
|---|---|---|---|---|
| CH (30 µg) | 8 (100%) | 0 (0%) | 0 (0%) | 8 (100%) |
| SP (10 µg) | 8 (100%) | 5 (62.5%) | 3 (37.5%) | 0 (0%) |
| CPX (10 µg) | 8 (100%) | 6 (75%) | 1 (12.5%) | 1 (12.5%) |
| AM (30 µg) | 8 (100%) | 0 (0%) | 0 (0%) | 8 (100%) |
| AU (30 µg) | 8 (100%) | 2 (25%) | 1 (12.5%) | 5 (62.5%) |
| CN (10 µg) | 8 (100%) | 1 (12.5%) | 1 (12.5%) | 6 (75%) |
| PEF (10 µg) | 8 (100%) | 6 (75%) | 0 (0%) | 2 (25%) |
| OFX (10 µg) | 8 (100%) | 5 (62.5%) | 2 (25%) | 1 (12.5%) |
| S (30 µg) | 8 (100%) | 0 (0%) | 0 (0%) | 8 (100%) |
| SXT (30 µg) | 8 (100%) | 0 (0%) | 0 (0%) | 8 (100%) |
Table 3: Percentage distribution of antibiotic susceptibility pattern among Pseudomonas aeruginosa isolates obtained from hospital fomites.
Keys
Positive (+) Negative (-)
The antibiotic susceptibility testing profile of all the 8 (100%) Pseudomonas aeuginosa isolates. There is high resistance to amoxicillin AM (30 μg), chloramphenicol CH (30 μg), streptomycin S (30 μg) septrin SXT (30 μg), Augmentin AU (30 μg) and gentamycin CN (10 μg) as follows; 8 (100%), 8 (100%), 8 (100%), 8 (100%), 5(62.5%) and 6 (75%). There is low resistance to sparfloxacin SP (10 μg), ciprofloxacin CPX (10 μg), tarivid OFX (10 μg) and pefloxacin PEF (10 μg) with 0 (0%), 1 (12.5%), 1 (12.5%) and 2 (25%) respectively.
This study has described the conventional experiments for determining the occurrence and antibiotic susceptibility pattern of Pseudomonas aeruginosa obtained from hospital fomites.
In this study, it was revealed that 16 (32.0%) of the total samples (50 (100%)) gave positive test on cetrimide agar (Cetrimide agar is a type of agar used for the selective isolation of the gramnegative bacterium, Pseudomonas aeruginosa. P. aeruginosa isolates produce either pyocyanin (blue-green) or pyoverdine (yellowgreen) colonies on centrimide agar). Of these 16 (100%) positive isolates, 5 (31.25%) were from stethoscope, 4 (25%) from sphygmomanometer, 3 (18.75%) from door knobs/handles, 2 (12.5%) from hospital rails and 2 (12.5%) from patient beddings. Inoculation into cetrimide agar is a presumptive test for the identification of Pseudomonas aeruginosa.
All the 16 (100%) suspected isolates showed gram negative origin, catalase positive, oxidase positive and citrate positive which are basic characteristics of Pseudomonas aeruginosa.
In order to support previous biochemical test, TSI (Triple Sugar Iron), D-mannitol fermentation and MR-VP test were carried out. The combination of all the biochemical tests increased the sensitivity to determine Pseudomonas aeruginosa among the bacterial isolates. Triple Sugar Iron (TSI), Methyl Red and Voges-proskauer (MR-VP) and mannitol fermentation test were carried out among the 16 cetrimide positive bacterial isolates. In mannitol fermentation test, 15 (93.75%) showed positive result. In TSI (Triple Sugar Iron) test, 8 (50%) showed positive result (i.e only 8 of the isolate showed red color at the butt (nonfermenter of glucose) and the slant (non-fermenter of lactose or sucrose), with no H2S and gas while the remaining 8 showed negative result. For MR-VP test, 3 (18.75%) isolates showed positive result for Methyl Red (MR) test and 2 (12.5%) showed for Voges-Proskauer (VP) test whereas 13 (81.25%) and 14 (87.5%) isolates were negative for each test respectively. With the combination of all the biochemical tests, 8 Pseudomonas aeruginosa isolates (amounting into 50.0% of the cetrimide agar positive bacteria and 16% of the total hospital fomites) were obtained from the experiment.
This data shows that the occurrence of Pseudomonas aeruginosa in the sampled hospital fomites is low. Most of the Pseudomonas aeruginosa obtained in this study were from the door knobs/ handles. The findings support the observation of Al-Zaidi that highest rate of P. aeruginosa which was identified from hospital environmental specimens study were from door handles (60%). This result could be explained by the fact that bacteria grow very well at sites with adequate amount of moisture and where people commonly come in contact with [16,17].
This data also show that there is zero occurrence of Pseudomonas aeruginosa among patient’s beddings. This could probably due to the fact that they are mostly kept dry.
Increasing resistance to different antibiotics especially among nosocomial pathogens has been reported worldwide and become important therapeutic challenge in the treatment of disease. This is in support of our findings where we obtain 100% resistance against chloramphenicol CH (30 μg), streptomycin S (30 μg) and septrin SXT (30 μg).
This study of Pseudomonas aeruginosa using conventional method is vital. In this study, 8 (100%) Pseudomonas aeruginosa were isolated; 3 (37.5%) from door knobs/handles, 2 h (25%) from stethoscope, 2 (25%) from sphygmomanometer, 1 (12.5%) from hospital rails. However from table 4.3 Pseudomonas aeruginosa is highly resistance to most of the antibiotic but, sparfloxacin, ciproflacin, tarivid and pefloxacin can be recommended for treating P. aeruginosa infection. Also this study can be used as a part of infection control measures in hospital environment in order to reduce the risk of occurrence and development of P. aeruginosa infection. Good hygiene practice methods are highly encouraged among health personnel to avoid crosscontamination on medical facilities.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Aso JO, Adekunle D, Aso OOO, Azeez OK (2023) Pseudomonas aeruginosa Associated with the Hospital Fomites in Ile-Ife, Osun State Nigeria. J Infect Dis Preve Med. 11:288.
Received: 27-Sep-2022, Manuscript No. JADPR-22-19376; Editor assigned: 29-Sep-2022, Pre QC No. JADPR-22-19376(PQ); Reviewed: 10-Oct-2022, QC No. JADPR-22-19376; Revised: 02-Feb-2023, Manuscript No. JADPR-22-19376(R); Published: 10-Feb-2023 , DOI: 10.35248/2329-8731.23.11.293
Copyright: © 2023 Aso JO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.