Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2024)Volume 12, Issue 9
Background: Stroke physicians often encounter a treatment dilemma when caring for patients with premorbid disabilities, who are typically excluded from randomized controlled trials focusing on Endovascular Treatment (EVT) for Large Vessel Occlusion (LVO). This study aims to compare the effectiveness and safety of EVT versus Medical Management (MM) in these particular patients.
Methods: We systematically searched PubMed, Embase, and the Cochrane Library for articles related to EVT in LVO patients with a prestroke modified Rankin Scale (mRS) score>1. The search spanned from the inception of these databases until July 19, 2023. The primary outcome measure was functional recovery, defined as a return to at least the prestroke mRS score within 90 days. Secondary outcomes included symptomatic intracranial hemorrhage and mortality rates at 90 days. Meta-analyses were conducted using random-effects models.
Results: The meta-analysis included six cohort studies comprising 2106 patients. In comparison to patients undergoing MM, those treated with EVT exhibited a greater likelihood of achieving functional recovery (4 studies; 1560 patients; risk ratio: 2.21; 95% confidence interval, 1.36 to 3.61; p=0.001; I2=69%) and lower mortality rates (6 studies, 2106 patients, risk ratio: 0.76; 95% confidence interval, 0.67 to 0.86, p=0.0001, I2= 13%) at the 90-day mark. Both sets of results were extremely statistically significant. Significant difference was also observed in terms of symptomatic intracranial hemorrhage between the two groups (5 studies, 1791 patients, risk ratio: 2.28, 95% confidence interval, 1.03 to 5.01, p=0.04, I2=29%).
Conclusion: For patients with LVO and a prestroke mRS score>1, although EVT results in a higher risk of bleeding, it improves the chance of a good functional outcome and reduces the risk of death. The practice of denying EVT solely on the basis of premorbid disability may not be justified.
Ischemic stroke; Disabled persons; Thrombectomy; Outcome; Meta-analysis
AIS: Acute Ischemic Stroke; LVO: Large Vessel Occlusion; EVT: Endovascular Therapy; BMM: Best Medical Management; mRS: modified Rankin Scale; sICH: symptomatic Intracranial Hemorrhage; CI: Confidence Interval; RR: Risk Ratio; NIHSS: National Institutes of Health Stroke Scale
Large Vessel Occlusion (LVO) is a leading cause of Acute Ischemic Stroke (AIS), significantly contributing to global disability [1- 6]. The introduction of Endovascular Thrombectomy (EVT) has set a new standard, proving to be the definitive treatment for reducing disability in LVO-induced AIS (LVO-AIS) [7]. The modified Rankin Scale (mRS) score is the benchmark for evaluating functional recovery in stroke survivors [8]. A notable segment of the LVO-AIS patient population presents with pre- existing conditions, termed pre-stroke disabilities [9,10]. Research shows that about one-third of patients undergoing EVT in standard clinical settings have baseline pre-stroke disabilities [10]. The inclusion of these patients in Randomized Controlled Trials (RCTs) is infrequent, as their pre-stroke mRS scores of ≥ 2 complicate the conventional outcome measures, which are largely binary in clinical studies [11]. As a result, these patients are often deemed to have a poor prognosis and may be less likely to seek treatment, leading to their exclusion from thrombectomy trials [12,13]. Current guidelines for managing patients with an mRS score of ≥ 2 are not well-defined, and an international survey has uncovered variability in EVT practices for patients with pre-stroke mRS scores of ≥ 2, with clinical judgment playing a significant role in the decision-making process [14,15]. This situation presents a therapeutic challenge for clinicians in choosing the most effective treatment to ensure timely and successful vascular reperfusion, aiming to improve clinical outcomes for this subgroup. Despite the insights from a prior systematic review, its exclusion of a control group receiving Medical Management (MM) limited the ability to discern the differential outcomes attributable to EVT [3]. This study seeks to compare the safety and efficacy of EVT against MM in patients with pre-stroke disabilities and to assess the safety and benefits of successful EVT reperfusion for these individuals [16]. The objective is to furnish comprehensive recommendations to support clinicians in selecting acute stroke treatment strategies for this specific patient demographic, with a focus on ensuring the best possible clinical outcomes.
This systematic review and meta-analysis was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [7].
Selection criteria
Comparative studies with English text that met the following PICO (Patient, Intervention, Comparator, and Outcome) criteria were considered eligible for inclusion [17].
Patients: Individuals aged ≥ 18 years with pre-LVO-AIS disability who had a pre-stroke 4 ≥ mRS ≥ 2.
Outcomes: The primary outcome was functional recovery, defined as return to at least the prestroke mRS at 90 days. Secondary outcomes including symptomatic Intracranial Hemorrhage (sICH) and mortality at 90 days.
Search strategy
Our search was last updated on 19 July 2023 to ensure there were no new studies meeting the eligibility criteria. Complete searching keywords were “prestroke” or “pre-stroke” or “stroke” and “premorbid” or “premorbid” or “preexisting” or “preexisting” or “previous” or “baseline” and “morbidity” or “mobility impairment” or “disability” or “disabilities” or “dependence” or “dependent” or “dependency” and “reperfusion therapies” or “reperfusion treatments” or “endovascular therapy” or “endovascular treatment” or “intra-arterial therapy” or “intraarterial treatment” or “endovascular thrombectomy” or “mechanical thrombectomy” or “intra-arterial thrombectomy” or “MT” or “EVT” or “IAT”.
Data extraction: The authors Tian-Yi Zhang and Dian Li independently extracted the information on study characteristics (first author, year of publication, study period, country, study design, number of institutions, population included, and number of patients), patient characteristics (age, sex, national institutes of health stroke scale), and clinical outcomes were collected. When duplicate reports of the same study were found, data were analyzed from the most complete data set. Objections were adjudicated by the senior author Heng-Zhu Zhang.
Risk of bias assessment
The quality of the included studies was assessed using the Newcastle-Ottawa Scale (NOS) research checklist [18]. These tools assess the selection, comparability, and outcome of both casecontrol and cohort studies. All studies were reviewed and scored based on the following aspects: Selection of study groups (0-4 points), comparability (0-2 points), and assessment of outcomes (0-3 points). The highest possible score is 9 points. A score of ≥ 8 indicates a low risk of bias, 6-7 indicates a moderate risk of bias, and ≤ 5 indicates a high risk of bias [3]. See Table 1, for details. Potential discrepancies were resolved through discussions with the senior author Heng-Zhu Zhang. Both reviewers Tian-Yi Zhang and Dian Li independently assessed the quality of all included studies, and any discrepancies were discussed until a consensus was reached.
| Study | Selection | Comparability control on the basis of the design or analysis | Outcomes | Scores | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representative of the exposed cohort | Selection of the non- exposed cohort | Ascertainment of the exposure | Demonstration that outcome of interest was not present at start of study | Assessment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow up of cohorts | |||
| Kastrup et al. [1] | * | * | * | * | * | * | - | * | 7 |
| Siegler et al. [2] | * | * | * | * | ** | * | * | * | 9 |
| Sprügel et al. [3] | * | * | * | * | ** | * | * | * | 9 |
| Tanaka et al. [4] | * | * | * | * | ** | * | * | * | 9 |
| Miyake et al. [5] | * | * | * | * | * | * | * | * | 8 |
| Sykora et al. [6] | * | * | * | * | * | * | * | * | 8 |
Note: *Indicates statistical significance at the level p ≤ 0.05; **Indicates a higher level of statistical significance at p ≤ 0.01.
Table 1: Newcastle-Ottawa scale for assessing the quality of studies in meta-analysis.
Statistical analysis
To derive the Risk Ratio (RR) from reported binary outcomes comparing EVT and BMM, we conducted a meta-analysis using the Mantel-Haenszel method without continuity correction. Our study results were presented as relative risks with corresponding 95% Confidence Intervals (CI). To appropriately account for variability within and between studies, we employed a random-effects model for the primary endpoint meta-analysis. Heterogeneity among studies was assessed using Cochran's Q statistic and the I2 statistic. For qualitative interpretation of heterogeneity, I2 values exceeding 50% were considered as significant heterogeneity, while values exceeding 75% were considered as considerable heterogeneity. All statistical analyses were performed using Review Manager (RevMan) version 5.3, developed by the Cochrane Collaboration in 2014, located at the Nordic Cochrane Centre in Copenhagen.
The initial search yielded 1495 records, with 357 duplicates. After reviewing titles and abstracts, 1120 records were excluded. Following a thorough examination of the remaining 18 full-text articles, a total of 6 publications were ultimately included in this systematic review and meta-analysis, involving 2106 AIS stroke patients comparing BMM and direct EVT (Figure 1).
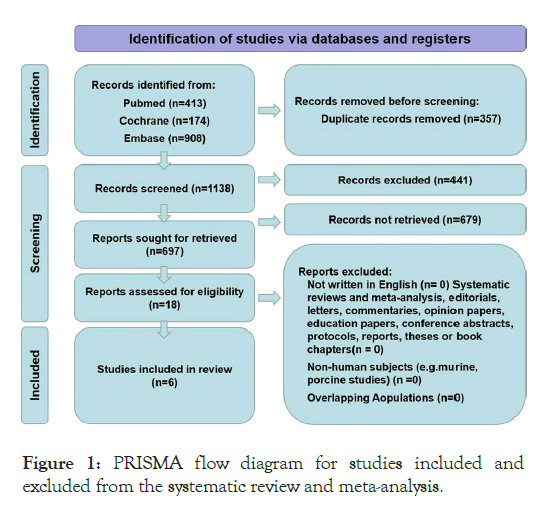
Figure 1: PRISMA flow diagram for studies included and excluded from the systematic review and meta-analysis.
All included studies were non-randomized multicenter retrospective cohort studies, gathering data from high-volume neurointerventional centers in five countries: Germany, Japan, Austria, Switzerland, and United States of America. Bias risk was assessed using the Newcastle-Ottawa Scale, and all six studies scored 7 or higher, reflecting an overall good quality of these studies (Table 1).
Study characteristics and patient demographics
The study participants consisted of 2106 acute stroke patients aged 18 years or older, all of whom had received treatment for prior proximal large vessel occlusion. This included occlusions in the intracranial proximal internal carotid artery and/or the M1 and/or M2 segments of the middle cerebral artery, along with associated disabling symptoms. Among these patients, 1300 received medical treatment, while 806 received drug treatment. Table 2, provides detailed elucidation of the distinct baseline characteristics of these patients. Each patient was managed according to the international ischemic stroke management guidelines. The control group comprised patients who did not undergo thrombectomy during hospitalization and received only medical treatment. Conversely, the intervention group encompassed patients who underwent routine thrombectomy during their hospital stay. (Table 2)
| Author | Year | Definition of pre-morbid disability and control groups | Number of patients (n) | Age (median) | %women | Return to baseline mRS, n (%) | sICH, n (%) | 90-days mortality, n (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Kastrup et al. [1] | 2021 | EVT | 3-4 | 142 | 83 ± 8 | - | - | 12 (8) | 31 (22) |
| BMM | 2-3 | 89 | 86 ± 7 | 7 (8) | 22 (25) | ||||
| Siegler et al. [2] | 2022 | EVT | 2-4 | 448 | 82 | 66.3 | 118 (26) | 31 (7) | 170 (38) |
| BMM | 2-4 | 106 | 8 (8) | 0 (0) | 48 (45) | ||||
| Sprügel et al. [3] | 2022 | EVT | 3 | 82 | 82 | 72.5 | 20 (20) | 6 (6) | 54 (53) |
| 4 | 20 | ||||||||
| BMM | 3 | 80 | 81 | 72.8 | 58 (8) | 1 (1) | 76 (74) | ||
| 4 | 23 | ||||||||
| Tanaka et al. [4] | 2021 | EVT | 2 | 70 | 82 | 65.1 | 49 (28) | 6 (3) | 31 (18) |
| 3 | 54 | ||||||||
| 4 | 51 | ||||||||
| BMM | 2 | 42 | 87 | 75 | 11 (18) | 2 (1) | 44 (27) | ||
| 3 | 54 | ||||||||
| 4 | 68 | ||||||||
| Miyake et al. [5] | 2023 | EVT | 2-3 | 258 | 82.2 ± 0.7 | 60.1 | - | - | 55 (21.3) |
| BMM | 2-3 | 57 | 83.4 ± 1.4 | 68.4 | 9 (15.8) | ||||
| Sykora et al. [6] | 2022 | EVT | 3 | 136 | 79.4 ± 12.2 | 62.3 | 47 (27) | 7 (4) | 76 (43) |
| 4 | 33 | ||||||||
| 5 | 6 | ||||||||
| BMM | 3 | 185 | 85.2 ± 8.8 | 65.2 | 58 (20) | 6 (2) | 180 (63) | ||
| 4 | 83 | ||||||||
| 5 | 19 | ||||||||
Note: EVT: Endovascular Therapy; BMM: Best Medical Management; mRS: modified Rankin Scale; sICH: symptomatic Intracerebral Haemorrhage.
Table 2: Baseline characteristics of included patients.
Primary outcomes (mRS no accumulation) at 90 days
Among the six studies, five reported favorable functional outcomes, involving 1560 pre-stroke disabled patients (with 900 receiving EVT treatment and 660 receiving BMM treatment). The primary endpoint was defined as a mRS score of 0-2 at 90 days. The study by Miyake et al., in 2023 defined the endpoint as a mRS score of 0-3 and was therefore not included in this analysis. The pooled analysis for this group of AIS patients confirmed that EVT improved the primary outcome of mRS scores of 0-2 at 90 days (Figure 2A) (RR=2.21; 95% CI=36-3.61; p=0.001), with a significant level of study heterogeneity and statistical significance (I2=69%, p=0.02).
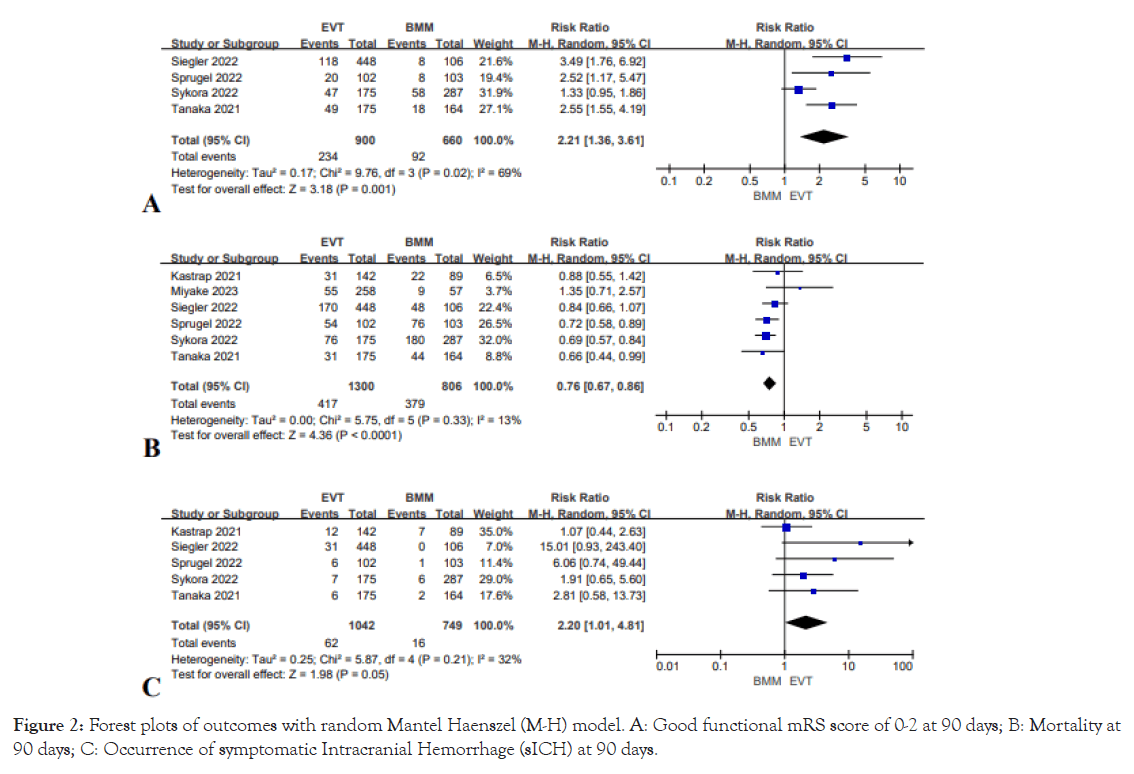
Figure 2: Forest plots of outcomes with random Mantel Haenszel (M-H) model. A: Good functional mRS score of 0-2 at 90 days; B: Mortality at 90 days; C: Occurrence of symptomatic Intracranial Hemorrhage (sICH) at 90 days.
Secondary outcomes 90-day mortality and sICH
All six studies, comprising a total of 2106 patients (1300 receiving EVT treatment and 806 receiving BMM treatment), provided data on the 90-day mortality rate for pre-stroke disabled patients. Specifically, the EVT group exhibited a lower 90-day mortality rate (RR=0.76; 95% CI=0.67-0.86; p<0.0001), as shown in Figure 2B. It is noteworthy that there was minimal heterogeneity and relatively significant statistical significance between the studies (I2=13%, p=0.33).
Among the five studies involving 1791 pre-stroke disabled patients (with 1042 receiving EVT treatment and 749 receiving BMM treatment), data were available to assess the occurrence of sICH. In terms of the rate of sICH occurrence, the EVT group demonstrated a higher risk compared to the medical treatment group (RR=2.28; 95% CI 1.03-5.01; p=0.04), as illustrated in Figure 2C. In this case, heterogeneity was also relatively low (I2= 29%; p=0.23) (Figure 2).
In the study of current treatment modalities for stroke patients, we've identified a notable limitation in stroke trial inclusions, primarily due to pre-existing disability factors. Given that a certain portion of the stroke patient population comprises individuals with pre-existing disabilities, the applicability of stroke trial outcomes to this subgroup is restricted. To address this gap, we embarked on a meta-analysis specifically targeting clinical trials that enrolled patients with disabilities prior to their stroke, drawing data from an extensive database search. Our objective was to support the treatment of patients already burdened with disabilities before their stroke occurrence.
Our comprehensive search culminated in the review of six studies, encompassing a total of 2106 participants. The findings from these controlled studies revealed that for AIS-LVO, recipients of EVT demonstrated a more favorable prognosis in regaining baseline functionality than those treated with BMM. Notably, EVT was found to be more effective in reducing mRS scores among pre-stroke disabled patients within a 90-day frame when juxtaposed with conventional medication therapy, subsequently leading to a decreased mortality rate. However, the EVT cohort also showed an increased likelihood of experiencing intracranial hemorrhage within the same period. Prior research, such as the observational study by Ganesh A et al., supports the potential for significant recovery to pre-stroke conditions in pre-stroke disabled patients undergoing surgery, without a heightened risk of treatment-related complications or the need for their routine exclusion from thrombectomy procedures. Similarly, Bala et al., aligned with these outcomes, but our analysis benefits from a larger sample size and a more systematic review and data analysis of EVT versus MM, thus strengthening the credibility of our findings.
The representation of pre-stroke disabled patients within the broader stroke patient demographic remains minimal, posing challenges to focused research endeavors. Considering the elevated risk of disability and stroke in already disabled patients, targeted research in this area is essential. We anticipate that further investigations will yield a refined understanding of endovascular treatment impacts on this specific patient group, facilitating the development of more precise treatment protocols [7,10]
Our meta-analysis, however, is not without limitations. The nature of the included studies-predominantly retrospective and observational-introduces inherent biases. Variabilities in baseline group characteristics limited the scope for deeper subgroup analyses and matched studies. Pre-EVT medication therapy, important or maintaining vascular patency, lacked detailed reporting on medication types and dosages, potentially influencing our findings. Moreover, the stringent inclusion criteria resulted in a moderate overall sample size, with the absence of primary outcome data in one study slightly skewing the results. The limited sample size also precluded further analyses on confounding factors, such as meta-regression and subgroup analyses, affecting the study's reliability and generalizability.
Looking forward, stroke treatment research, encompassing both endovascular and medication interventions, is poised for expansion. This study proposes a novel approach to researching stroke treatment in distinct patient populations, paving the way for more personalized and nuanced interventions. As healthcare professionals incorporate insights from clinical guidelines and recent research, treatment strategies are expected to evolve, enhancing patient outcomes. We also advocate for increased clinician awareness of such special patient groups, anticipating that through rigorous research and precise interventions, treatment outcomes for pre-stroke disabled patients will significantly improve.
The core aim of our investigation was to ascertain the most suitable treatment modality for AIS patients who have experienced poststroke disability. To this end, we meticulously searched various literature databases, including PubMed, Embase, Cochrane, and others, for pertinent studies. Following a thorough review process, six studies that aligned with our predetermined inclusion criteria were chosen. These studies specifically examined adult patients with pre-existing disabilities, all of whom had a mRS score greater than 2 and were deemed candidates for therapeutic intervention.
Our comprehensive analysis of the data from these studies revealed that thrombectomy, with a focus on EVT, yielded positive outcomes in the treatment of disabled AIS patients. More precisely, EVT was associated with improvements in mRS scores at 90 days post-treatment and led to a decreased mortality rate compared to traditional medical therapies. Despite the increased bleeding risk associated with EVT, the procedure significantly enhances the likelihood of achieving a favorable functional outcome and decreases the risk of mortality. The exclusion of EVT as a treatment option based solely on a patient's premorbid disability status appears to be unjustifiable.
A notable limitation of our study is that it includes only six cohort studies, encompassing a total of 2106 patients, which limits the ability to draw definitive conclusions. Additionally, the observational nature of the included studies introduces a potential for confounding bias, a common issue in the limited research available on this topic.
Given these findings, we conclude that EVT stands out as the treatment of choice for AIS patients with disabilities, a recommendation that holds true regardless of a patient's preexisting disability status. This conclusion underscores the need for the medical community to focus greater attention on stroke patients with disabilities and advocates for the publication of more high-quality clinical trials. Such research is essential to enhance the precision of future analyses and to ensure that treatment decisions are based on robust evidence, ultimately improving outcomes for this underserved patient population.
This study was supported by grants from the National Natural Science Foundation of China (No. 82172603), the Natural Science Foundation of Jiangsu Province (No. BK20190241), the Scientific Research Project of Jiangsu Provincial Health Commission (H2018064) and the Cross Cooperation Project of Northern Jiangsu People's Hospital (SBIC21009).
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhang TY, Li D, Hu YQ, Zhang HZ (2024). Endovascular Treatment versus Medical Management in Patients with Large Vessel Occlusion and Prestroke Disability. Angiol Open Access. 12:496.
Received: 20-Sep-2024, Manuscript No. AOA-24-34155; Editor assigned: 23-Sep-2024, Pre QC No. AOA-24-34155 (PQ); Reviewed: 07-Oct-2024, QC No. AOA-24-34155; Revised: 14-Oct-2024, Manuscript No. AOA-24-34155 (R); Published: 21-Oct-2024 , DOI: 10.35841/2329-9495.24.12.496
Copyright: © 2024 Zhang TY. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.