
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Mini Review - (2023)Volume 14, Issue 5
With the advances in medical and surgical fields, with the evolution of surgeries for more complex situations, more frail patients, often elderly with multiple comorbidities with advanced stages of incidental diseases, are more often presenting for surgeries.
Many of these patients with varying systemic comorbidities require preoperative cardiology and echocardiography evaluation as a component of preoperative assessment, risk stratification, and optimization before choosing the appropriate anaesthetic management plan and surgical approach. Frequent cardiology referrals for this task often prove to be a time-consuming and expensive process, increasing the delay in time from hospital admission to surgery and the total duration of hospital stay. Such preoperative delays indirectly increase perioperative morbidity, mortality, and patient anesthesia dissatisfaction.
To confront these hurdles, Perioperative Transthoracic Echocardiography (PTTE) services by trained anesthesiologists have gained prominence. Not only do these services offer a cost-efficient alternative, but they also expedite decisionmaking in urgent scenarios. Recent ESC guidelines also suggested Focused Cardiac Ultrasound (FoCUS) performed by trained specialists to be considered as an alternative to comprehensive echocardiography for pre-operative triage to avoid delaying surgery.
This article emphasizes the pivotal role of PTTE in perioperative care, highlighting its utility in managing hemodynamic instability, preoperative optimization, efficient utilization of health care resources and enhancing patient outcomes. It also addresses non-cardiac anesthesiologists' reluctance to embrace PTTE, primarily due to the absence of standardised training and certification.
Certification and formal PTTE training empower non-cardiac anaesthesiologists and help to incorporate echocardiography into their perioperative practices. Moreover, integrating PTTE into residency training curricula and establishing dedicated PTTE teams are essential steps in promoting its routine use. Adherence to quality assurance measures and enhancing operator performance in PTTE services significantly improve patient care and perioperative outcomes.
Transthoracic echocardiography; Cardiovascular disease; Anaesthesia; Perioperative transthoracic echocardiography; Electrocardiogram
The ability to face the challenges invites more challenging situations. This is the routine in the process of development of any system. Anaesthesiologists as perioperative physicians are evolving, keeping themselves in pace with the evolving science, technology, and the resulting gadgets to produce safer outcomes in challenging clinical scenarios.
The landscape of patients requiring surgery has evolved significantly over time. Advancements in surgical and medical fields, coupled with a rise in sedentary lifestyles, have led to a significant shift in the demographics of surgical patients. Elderly patients, patients with multiple comorbidities or advanced diseases, those undergoing daycare surgeries, and patients presenting for minimally invasive procedures now constitute a substantial portion of the surgical patient population. There has been a growing tendency towards minimizing preoperative testing, driven by the goals of controlling surgery costs, avoiding unnecessary referrals, and enhancing patient satisfaction. This approach aimed to optimize the utilization of healthcare resources while ensuring that patients receive the appropriate perioperative care they need. Cardiac complications are frequent following major non-cardiac surgery, and Major Adverse Cardiac Events (MACE) represent a major cause of post-operative mortality [1].
Transthoracic Echocardiography (TTE) plays a significant role in identifying major cardiac pathologies before surgery, which are the common predictors of MACE. The American College of Cardiology (ACC) /American Heart Association (AHA) in 2014 and more recently in 2022. The European Society of Cardiology (ESC), have published guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery [2,3]. According to the 2022 ESC guidelines, preoperative echocardiography is recommended in patients with poor functional capacity (Metabolic Equivalents (METs) <4), or elevated NT-proBNP/BNP, or presence of murmur, abnormal Electrocardiogram (ECG), or suspected new or significant Cardiovascular Disease (CVD) within the last 90 days, unexplained dyspnoea, or coexisting clinical risk factors as appropriate indications for TTE before intermediate and high-risk surgeries (Table 1) [3].
| S. No. | Risk Factors |
|---|---|
| 1. | Signs and symptoms of CVD: chest pain, dyspnoea, crepitations, dependant or peripheral oedema, murmur, abnormal heart sounds, poor functional capacity (METS<4 (inability to climb two flights of stairs) or unable to assess METS), syncope |
| 2. | Risk factors for CVD: age>65 years, diabetes mellitus, hypertension, dyslipidaemia, smoking, obesity |
| 3. | Unreliable medical history: emergencies, dementia, intoxicated patients, |
| 4. | Family history suggesting a high risk of CAD or cardiomyopathies |
| 5. | Cardiac Biomarkers: NT-proBNP/BNP, High-sensitive cardiac troponin (hs-cTn) T/I |
| 6. | Moderate or high-risk non-cardiac surgery |
| 7. | Cerebrovascular disease or peripheral vascular disease |
| 8. | Aneurysms |
| 9. | Serum creatinine level ≥ 2 mg/dL or abnormal GFR or renal failure |
| 10. | Arrhythmias or history of arrhythmias |
| 11. | History of cardiac surgery or intervention |
| 12. | Pulmonary embolism or deep vein thrombosis (DVT) |
Table 1: Risk factors associated with cardiovascular diseases.
Compliance to cardiology referral recommendations
Hoehmann et al., reviewed 412 patients admitted with geriatric hip fracture for compliance of the AHA/ACC guidelines for preoperative TTE and cardiac consultations [4]. They found that out of 44.4% of patients who received cardiology consultation, only 17.7% of patients met the criteria. These consultations are expensive and delay surgery, which can increase morbidity and mortality.
Unnecessary cardiology referrals, the growing workload on echocardiography laboratories, and shortage of cardiologists are all significant factors that can lead to delays time to surgery. Efforts to address these issues may include improving adherence to clinical practice guidelines regarding cardiology referrals and initiating Perioperative Transthoracic Echocardiography (PTTE) services by trained anaesthesiologists in major healthcare facilities especially in emergency settings. Training and certification of present-day anaesthesiologists in echocardiography is more practical, as they are already familiar with ultrasound-guided regional anaesthesia and vascular access procedures and cardiovascular anatomy in various pathological situations.
Role of perioperative transthoracic echocardiography
The ESC 2022 guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery also recommended Focused Cardiac Ultrasound (FoCUS) performed by trained specialists to be considered as an alternative to comprehensive echocardiography for pre-operative triage to avoid delaying surgery (class IIb indication). This means that based on the FoCUS findings, anaesthesiologists can decide to send the patient for further evaluation by the cardiologist, or else the patient can be accepted for surgery without further evaluation. Figures 1 and 2 illustrate the simplified triage process for cardiology evaluation before non-cardiac surgery (Figures 1 and 2).
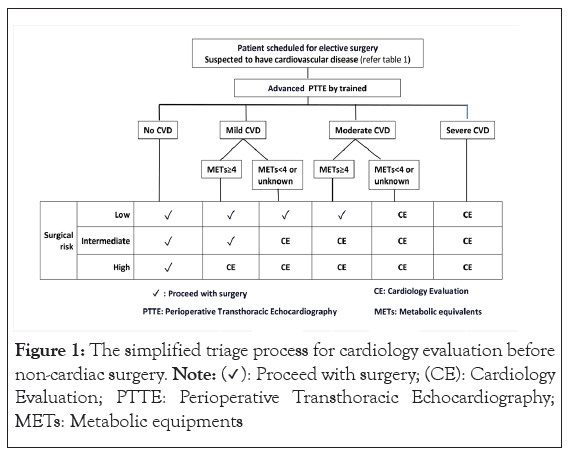
Figure 1: The simplified triage process for cardiology evaluation before non-cardiac surgery. Note: (✓): Proceed with surgery; (CE): Cardiology Evaluation; PTTE: Perioperative Transthoracic Echocardiography; METs: Metabolic equipments.
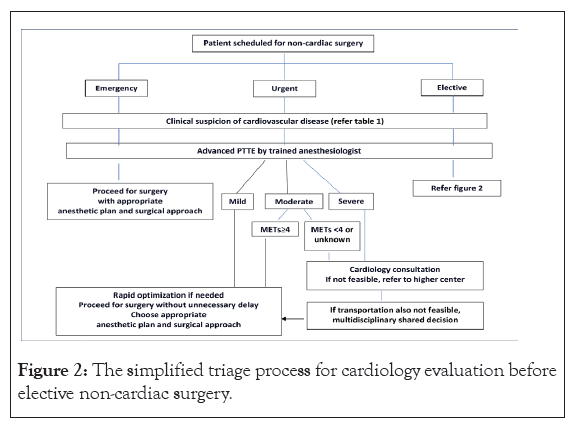
Figure 2: The simplified triage process for cardiology evaluation before elective non-cardiac surgery.
In addition to the pre-anaesthetic assessment, TTE plays a crucial role in perioperative hemodynamic instability and hypoxemic states to improve diagnostic rapidity and accuracy and to choose the appropriate anaesthetic plan, monitoring, surgical approach and strategy for postoperative pain management. TTE also helps optimize patient care during the perioperative critical periods by offering real-time insights into cardiac function and relevant parameters. Due to its versatility and efficiency, ultrasound has become a standard of care in various medical specialties such as cardiac surgery, liver transplant, critical care, and emergency medicine. It's also a routine tool for procedures like peripheral nerve blocks and vascular cannulations.
Reluctance among non-cardiac anaesthesiologists to incorporate TTE into their practice
Despite its wider availability and proven utility, many non-cardiac anaesthesiologists have not fully embraced TTE as a routine diagnostic tool for cardiovascular and respiratory evaluation in their day-to-day perioperative practice.
This reluctance can be attributed to a lack of training, certification and fear of overlooking pathologies. Currently, there are no prescribed standardised guidelines or recommendations for PTTE training, certification, or practice for anesthesiologists. The absence of such guidelines may also delay training the non-cardiac anaesthesiologists in this field.
Categories of PTTE
Subramaniam et al. made a commendable and sincere effort to bridge this gap by comprehensively describing the training requirements, scope of practice, and organized approach to performing PTTE [5]. Their work serves as a valuable resource in establishing much-needed standards and guidelines in this field. They broadly categorized PTTE into 3 levels: basic PTTE, advanced PTTE, and Comprehensive Transthoracic Echocardiography (CTTE) levels. Anaesthesiologists can perform basic and advanced levels of PTTE, whereas CTTE is mostly reserved for cardiologists and physicians after completion of level 2 echocardiography.
The basic level of PTTE covers the qualitative assessment of cardiovascular and respiratory evaluation in emergency situations by utilizing the 2-dimensional echocardiography and color doppler. Various rescue echocardiography protocols like Point of care Cardiac Ultrasound (POCUS), FoCUS, Focused Assessment with Sonography in Trauma (FAST), Extended FAST (e-FAST) and Focus-assessed Transthoracic Echocardiography (FATE) can be considered under the basic level of echocardiography. This basic PTTE examination is very useful as a diagnostic tool in perioperative emergencies like hypotension and hypoxia. To become competent in basic PTTE, according to Subramanian et al., one needs to perform and interpret twenty-five basic PTTE scans [5].
Information from the basic qualitative echocardiography guides the anaesthesiologist in the selection of invasive monitoring, risk stratification, need for post-op ventilation and reserving the bed in the intensive care unit. This valuable information is more important in surgical emergencies when the patient’s cardiac status is unknown due to difficulties obtaining the patient's medical history, in intoxicated and unconscious patients in the absence of close relatives etc. The scope and training guidelines for basic PTTE have been issued by various medical societies under different titles like cardiac POCUS, FoCUS, Basic CCE, Critical Care Echocardiography (CCE), FATE, etc.
Unlike basic echocardiographic examinations, there are no recommendations or guidelines for anaesthesiologists for advanced PTTE. Subramaniam et al. described 13 transthoracic views through the 3 imaging windows [5]. This examination includes spectral doppler along with 2D echo and colour doppler. Advanced PTTE examination includes quantitative evaluation of myocardial function (ejection fraction), valvular and ventricular outflow tract gradients, severity of valvular regurgitations, left and right ventricular filling pressures, and pulmonary artery pressures. This examination also covers the assessment of the degree of myocardial hypertrophy, and structural abnormalities like congenital heart diseases, chamber enlargement, aortic or pulmonary artery dilatation, etc. Critical care physicians, non-cardiac anaesthesiologists, and cardiac anaesthesiologists may take part in this program after completing basic PTTE. According to Subramaniam et al., the minimum training requirements should be 150 individually performed and interpreted advanced PTTE tests [5].
Scope of advanced PTTE
Advanced PTTE may be considered in patients with clinical signs of cardiac diseases (chest pain, dyspnoea, dependent or peripheral oedema, basal crepitations, palpitations, murmur, syncope, clubbing, cyanosis, ECG or Chest X-ray abnormalities, before high-risk non-cardiac surgeries and in patients at risk of developing perioperative cardiac complications like obesity, Hypertrophic Obstructive Cardiomyopathy (HOCM), pulmonary hypertension, etc.
The findings of advanced PTTE are very useful for preoperative triage, risk stratification, accurate assessment of clinical condition, preoperative optimization, choosing appropriate therapeutic intervention, designing an anaesthetic plan (general anaesthesia with cardio-stable induction (etomidate/high dose opioid), graded epidural, peripheral nerve block, etc.), modification of surgical technique (open or laparoscopic approach), postoperative analgesia plan, need for invasive monitoring, and optimal utilisation of resources (intensive care services).
Serial PTTE plays a critical role in evaluating the efficacy of the therapeutic intervention and dynamic evaluation of the patient's cardiovascular status. Several studies have demonstrated its role in rare perioperative period complications like air embolism, unexplained tachycardia, pulmonary oedema, aortic dissection, cardiac arrest, pulmonary embolism, and cardiac tamponade [6,7]. Due to its versatile role, timely utilisation of PTTE has been shown to improve perioperative risk-adjusted all-cause mortality at one year after surgery [8].
Role of PTTE services offered by the trained anaesthesiologist
Certification and widespread training play a pivotal role in promoting the routine use of PTTE by anaesthesiologists. By incorporating PTTE into the residency training curriculum, future anaesthesiologists can develop the necessary skills and confidence to perform and interpret echocardiography effectively. Establishing dedicated teams to initiate PTTE services is the critical step for training and practice. Cardiac anaesthesiologists or critical care physicians who are trained in TTE should take the initiative to start the PTTE services in major healthcare facilities to train non-cardiac anaesthesiologists. Once the non-cardiac anaesthesiologists are trained, they can lead the PTTE services by themselves.
Several echocardiography societies, the National Board of Echocardiography (NBE), the Indian Association of Cardiovascular Thoracic Anaesthesiologists (IACTA), etc., offer certification courses in trans esophageal echocardiography. However, none of these societies offers certification in the field of PTTE to the best of the authors' knowledge. Medical universities with established PTTE services or echocardiography societies should take the initiative in establishing training standards for different levels of PTTE and certification.
Certification not only ensures competence but also boosts confidence among non-cardiac anaesthesiologists. This increased confidence can be instrumental in their willingness to incorporate echocardiography into their perioperative practices. Patients and healthcare institutions are often willing to pay for specialized services that enhance patient care, improve outcomes, and potentially reduce costs by minimizing unnecessary referrals and additional testing.
Quality assurance and quality improvement
Striving for excellence and continuously improving quality is a fundamental principle in delivering effective and reliable services. The American Society of Echocardiography (ASE) has issued recommendations for assessing and enhancing echocardiographic quality for average echocardiography practitioners [9]. Even though these recommendations are primarily focused on adult comprehensive echocardiography, quality indicator measures like patient selection, image acquisition, image interpretation, documentation of physician-to-physician communication of the critical values, and incorporation of results into care can serve as a valuable reference for ensuring and enhancing the quality of PTTE services. Periodic reviews of the completeness and timeliness of PTTE reports can help identify areas for improvement and ensure that all necessary information is documented. Adherence to established quality improvement standards not only benefits patient care but also contributes to the ongoing professional development of PTTE operators, ultimately enhancing their performance.
Establishing dedicated PTTE services provided by trained anaesthesiologists is very much needed in major healthcare facilities to reduce the delay to surgery, reduce the volume of referrals, and improve patient satisfaction and outcomes. Competence in PTTE is becoming increasingly essential for perioperative physicians to deliver the highest standard of care to surgical patients. By integrating PTTE training and education into the curriculum, future anaesthesiologists can develop the skills necessary to perform and interpret echocardiography effectively.
The suggestions and flowcharts outlined in this article represent the authors' personal opinions and expert perspectives. It is essential to acknowledge that insufficient evidence supports these recommendations. Decisions related to perioperative triage should be made by practicing anaesthesiologists based on a thorough consideration of individual patient circumstances. Factors such as the patient's financial capabilities, accessibility to prompt cardiology services, transportation resources, healthcare infrastructure, and available health resources in a particular region or institution can significantly influence decision-making in the perioperative setting. Consequently, clinicians are encouraged to exercise their best judgment and adapt their approach to their practice environment's unique conditions and resources.
PTTE services require an increased number of trained anaesthesiologists, which can place additional demands on healthcare staffing. Additionally, the need for sophisticated equipment adds to the cost and resource requirements. It is crucial that PTTE is conducted within its defined scope of practice. Misinterpretation or inappropriate use of PTTE outside its intended field can lead to inaccurate assessments and potentially harm patient care.
The authors of this article declare that they have no conflicts of interest related to the research, content, or publication of this manuscript. This declaration encompasses any financial interests, affiliations, or relationships that could potentially influence the objectivity, integrity, or interpretation of the research findings presented herein.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Sundar AS, Bethi R, Ramachandran G (2023) Enhancing Anaesthesia Care: The Vital Role of Perioperative Transthoracic Echocardiography Services. J Anesth Clin Res. 14:1112
Received: 07-Sep-2023, Manuscript No. JACR-23-26651; Editor assigned: 11-Sep-2023, Pre QC No. JACR-23-26651 (PQ); Reviewed: 27-Sep-2023, QC No. JACR-23-26651; Revised: 04-Oct-2023, Manuscript No. JACR-23-26651 (R); Published: 11-Oct-2023 , DOI: 10.35248/2155-6148.23.14.1112
Copyright: © 2023 Sundar AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.