Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2020)Volume 11, Issue 2
Introduction: Symblepharon is a lesion on the ocular surface associated or not with ocular adnexa damage.
Symblepharon is characterized by the formation of an adhesion between the palpebral conjunctiva and the bulbary
conjunctiva. There are many causes of symblepharon, among which toxic epidermal necrolysis is the most well-known
and documented due to the extreme severity of ocular damage. Hence the purpose of this study is to describe the
epidemiological-clinical profile of the symbpharon during the toxic epidermal necrosis for adequate and appropriate
management.
Methodology: This was a cross-sectional study, lasting 24 months from 18 March 2018 to 17 March 2020 at CHUIOTA.
All patients who consented and had the symblepharon regardless of sex and age were compiled in a nonprobability
sample.
Results: During the 2 years, 11 patients were collected. There were 4 Men and 7 Women. The average age of our
patients was 36.81 14.60 years, the age extremes ranged from 7 years old to 65 years old. The association of
Nevirapine and Cotrimoxazole was frequently incriminated in 36.4% of our patients. More than half of the
symblepharon were anterior (55% of the cases).
Discussion: The bilaterality of ocular damage would be related on the one hand to the immunological mechanisms
of toxic epidermal necrolysis, and the association of Nevirapine with Cotrimoxazole on the other.
Conclusion: A rare disease, toxic epidermal necrolysis often leads to severe ocular complications.
Symblepharon; Toxic epidermal necrolysis; Nevirapine; Cotrimoxazole; Bamako
Toxic epidermal necrosis (TEN) is an acute necrosis of the epidermis exceeding 30% of the body area, usually of druginduced toxic origin and in the presence of several cofactors [1]. It is a dermatological emergency because it involves short-term life prognosis [2]. When its evolution is favourable, the healing takes place within two weeks but leaves the most often serious sequelae affecting especially the mucous membranes (including oculars) [3]. The most serious and disabling ophthalmological sequel is the symbpharon, which is the adhesion of the two conjunctives (palpebra and bulba) [3]. NET is a rare disease, with a low incidence of 1 to 2 cases per million inhabitants per year [4], but evolution is fatal in about 22% of cases. It mainly affects adults but can be seen at any age [5].
A few cases have been reported in Africa [6-10].
The low case report in Africa and the absence of data in Mali in particular led to the completion of this study, the purpose of which is to contribute to the epidemiological and clinical descriptions of symblepharon during the TEN in Bamako.
We carried out a descriptive cross-sectional study in the external consulting department of the IOTA-Teaching Hospital. Extending over a period of 24 months (18 March 2018 to 17 October 2020) and carried the cases of toxic epidermal necrolysis received having presented a symblehon with or without other ophthalmological manifestations. Not all cases of toxic epidermal necrosis with no symbleropharon were included in the study. The variables of our study were:
- Epidemiological characteristics including age, sex, serological status, personal pathological history, the drugs involved.
- The clinical features including the reason for the visit, the time of onset of symptoms, the time of the visit, the type of symblepharon, the associated ocular damage.
- The data were collected using a survey sheet containing the above parameters. Statistical analysis of data using SPSS software version 25.
During the study period, we collected 11 cases of bilateral symblepharon, or the annual frequency of 5.5 cases per year.
The average age of our patients was 36.81 ± 14.60 years, the age extremes ranged from 7 years old to 65 years old (Figure 1). Age group 28-38 was most common (Figure 1). There was a female predominance with an M/F sex ratio of 0.36 (Figure 1). More than half (55%) of our patients were immunocompromised by retroviral infection (Figure 2) and 36% of patients had no past history of disease (Figure 2). Anti retrovirals (ARV) associated with sulfamides was responsible for TEN in 36.4% of our patients (Table 1). The most frequent onset of ocular symptoms (54.5%) ranged from 1 to 2 weeks (Table 2). Ophthalmological consultations were too late (6 months or more) in 45.5% of cases (Table 3). The common Ocular symptoms were decreased visual acuity (100%), ocular pain (81.81%), tears flow (63.63%) and foreign body sensation (54.5%) (Table 4). The clinical feature of the symblepharon was mainly ankyloblepharon (55%). We have no observed the posterior symbleropharon in our study (Figure 3).Palpebral sequelae were the most common associated ocular damage (145.5%) and corneal lesions accounted for 100.1% followed by lacrimal lesions in 45.5% (Table 5).
| Drug name | Number (n) | Percentage (%) |
|---|---|---|
| Unknow | 1 | 9,1 |
| Cotrimoxazole | 2 | 18,2 |
| Ibuprofene | 1 | 9,1 |
| Névirapine | 2 | 18,2 |
| Paracetamole+Ibuprofène | 1 | 9,1 |
| Nevirapine+Cotrimoxazole | 4 | 36,4 |
| Total | 11 | 1 |
Table 1: Distribution of Patients by Drug in question.
| Time to Onset | Number (n) | Percentage (%) |
|---|---|---|
| Moins de 7 Jours | 1 | 9,1 |
| De 7 jours à 14 jours | 6 | 54,5 |
| 14 jours et plus | 4 | 36,4 |
| Total | 11 | 100 |
Table 2: Distribution of patients by time to onset of Symptoms.
| Delay of consultation | Number (n) | Percentage (%) |
|---|---|---|
| Less than 1 month | 3 | 27,3 |
| From 1 month to 3 months | 2 | 18,2 |
| From 4 months to 6 months | 1 | 9,1 |
| From 6 months to 12 months | 1 | 9,1 |
| 12 months and more | 4 | 36,4 |
| Total | 11 | 100 |
Table 3: Distribution of Patients by delay of ophtalmological consultation.
| Symptoms | Number (n) | Percentage (%) |
|---|---|---|
| Visual loss | 11 | 100 |
| Pain | 9 | 81,81 |
| Tears flow | 7 | 63,63 |
| Feeling of a foreign body | 6 | 54,5 |
| Redness | 5 | 45,5 |
| Total | 38 | 345,44 |
Table 4: Distribution of Patients by Ocular Symptoms.
| Ocular disease | Number (n) | Percentage (%) |
|---|---|---|
| Palpebrale Erosion | 5 | 45,5 |
| Entropion+Trichiaisis | 6 | 54,5 |
| Meat lacrymal stenosis | 5 | 45,5 |
| Superficial Keratitis | 4 | 36,4 |
| Corneal Dystrophy | 4 | 36,4 |
| Pre-perforative Staphyloma | 2 | 18,2 |
| Coreal Ulceration | 1 | 9,1 |
| Total | 27 | 245,6 |
Table 5: Distribution of Patients by Associated Ocular Disease.
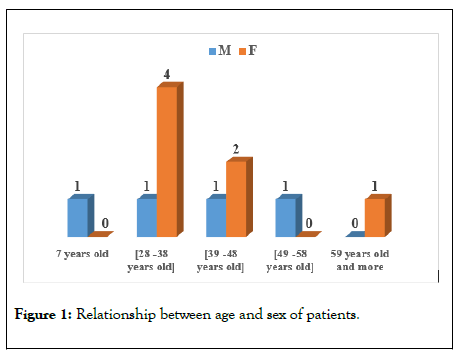
Figure 1: Relationship between age and sex of patients.
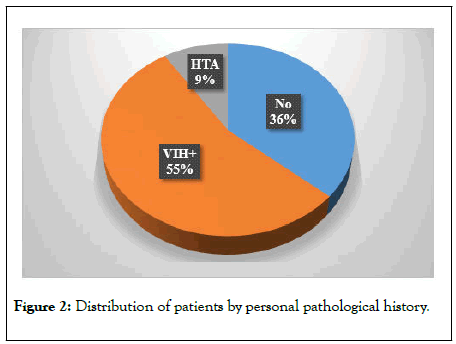
Figure 2: Distribution of patients by personal pathological history.
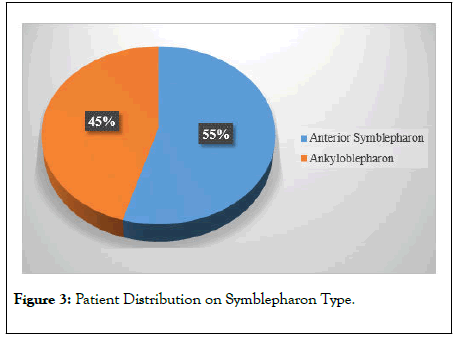
Figure 3: Patient Distribution on Symblepharon Type.
In our study, we found an annual hospital frequency of the TEN symbpharon of 5.5 cases per year. The hospital frequencies found in Africa are disparate and ranged from 1.45 cases to 12 cases per year [3,6-12]. The difference in methodology between the studies and the rarety of TEN in these different, would explain the discrepancy observed in annual frequencies.
We observed in our study a female predominance (sex-ratio M/F of 0.36) consistent with the results of Treichville [7] but contrary to the results of some authors in the sub-region, who noted a male predominance [6-9]. Demographic arguments and the diversity of our study populations would justify this observation.
The average age of our patients was 36.81 ± 14.60 years with age extremes ranging from 7 years old to 65 years old. This average age is higher than that found in Central Africa [6,8]. All youth of the African population would be the likely explanation for the high frequency of youth in our samples.
HIV infection was found in more than half of our patients. Our result is consistent with those found in the sub-region [6-12]. The emergence of the more severe clinical forms of TEN would be favoured by some co-factors, primarily HIV infection. HIV by weakening the immuno-allergic system, would promote the high frequency of TEN.
ARV associated with sulfamides was the most common cause in 36.4% of cases. This observation is consistent with those of authors in Africa [6-12]. Indeed the responsibility of Arvs and their association with sulfamides in the occurrence of TEN is widely demonstrated in the literature.
The time elapsed between the date of onset of TEN symptoms and the date of ophthalmological consultation was frequently greater than 06 months in 45.5% of cases. This result confirms the consultation of the ophthalmologist in second intention (in the sequelae phase), once the medical emergency has been overcome. It is important to emphasize to our dermatologist colleagues the multidisciplinarity of the therapeutic management of TEN, including the contribution of the ophthalmologist in case of eye symptoms from the initial phase of the disease.
The most common eye symptoms were decreased visual acuity (100%), eye pain (81.81%) and watering (63.63%). In contrast to the results of Triechville [7], where the most common symptoms were pruritus (68.75%) and decreased visual acuity (68.75%). In our study, the ocular symptoms observed reflected the presence of the ocular sequelae of the TEN.
Ankyloblepharon was the clinical characteristic of the symblehon most commonly encountered (55% of cases). These ankyloblepharon were associated with palpebral disorders of entropion and trichiasis in 54.5% of cases. As confirmed by the results found in Africa [6-12]. These ocular sequelae only allow for surgical management, thus clearly limiting the therapeutic options available for ophthalmology. Hence the need to highlight the positive contribution of the participation of the ophthalmologist in the initial phase of the TEN for the prevention of these often severe and blinding ocular sequelae.
This study confirmed that symblepharon is the common ocular and mucocutaneous sequelae in TEN survivors. These gravisimous ocular sequelae are unfortunately late diagnosed. The participation of the ophthalmologist from the initial phase of the disease should be emphasized in order to take early therapeutic measures to avoid the occurrence of ophthalmological sequelae that fall under surgical treatment.
Citation: Elien GYRR, Seydou B, Adam DM, Thera JP (2020) Epidemio-clinical profile of the symbpharon during toxic epidermal necrolysis (TEN) at the Institute of African Tropical Ophthalmology-Teaching Hospital. J Clin Exp Ophthalmol. 11:831. DOI: 10.35248/ 2155-9570.20.11.831
Received: 27-Mar-2020 Accepted: 10-Apr-2020 Published: 17-Apr-2020 , DOI: 10.35248/2155-9570.20.11.831
Copyright: © 2020 Elien GYRR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.