Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 3
Introduction: Ocular trauma is a global concern causing visual impairment and blindness, affecting all age groups and occurring in various settings, including homes, workplaces and leisure activities. This study investigates the epidemiological patterns of ocular trauma in adult patients in China, to understand the characteristics and causes of these injuries.
Materials and methods: We analyzed data from a diverse sample of adult patients who suffered ocular trauma. Hospital stay duration, as an indicator of injury severity and recovery complexity, was the primary outcome measure. We used Analysis of the Variance (ANOVA) and post-hoc tests to compare hospital stays among different diagnostic categories. Changes in vision acuity before and after the injury were secondary outcomes, analyzed using paired t-tests.
Results: The majority of patients were male and farmers constituted a significant portion of the sample. Foreign body, falls, fights and traffic accidents were the most common causes of injury, with the left eye affected more frequently. Fractures and orbital injuries were the predominant diagnoses. The mean hospital stay was 14.69 days, varying significantly by diagnosis, injury cause and vision acuity changes. Occupation did not significantly affect hospital stay or vision acuity. However, male gender, binocular injury, poorer vision acuity at admission and specific diagnoses predicted longer hospital stays.
Conclusion: This study highlights a substantial occurrence of ocular injuries in the Chinese population, with certain factors and causes being more prevalent. Occupational and environmental conditions, as well as demographic characteristics, may influence the likelihood of ocular trauma. Understanding these epidemiological patterns can guide preventive measures and improve visual health outcomes in China.
Ocular trauma; Epidemiological patterns; Visual impairment; Injury severity; Chinese population
Ocular trauma injuries are an easily preventable cause of blindness, yet they are nonetheless a serious impairing health issue that affects individuals of all ages [1]. Injuries might occur within the household, at work, during leisure activities or in a car accident. It contributes to a significant number of injuries, accounting for approximately 7% of all bodily injuries and 10%-15% of all eye diseases [2,3]. Injuries can range from a closed globe, including contusion or lamellar laceration, to an open globe, including rupture, puncture and globe perforation. The statistics surrounding ocular trauma are alarming, with millions of individuals suffering from blindness or visual impairment as a result of ocular injuries. According to the World Health Organization (WHO), around 55 million eye injuries occur each year, impairing activities for more than one day. Around 750,000 of them will need hospitalization, including approximately 200,000 cases of open-globe accidents. Furthermore, an estimated 1.6 million persons are blind because of eye injuries; 2.3 million have bilaterally impaired vision and around 19 million have unilateral blindness or low vision [4]. Risk factors like age, gender, socioeconomic status and lifestyle contribute to the risk of ocular trauma and the injury location is also related to the severity level.
Several studies have reported that males are more likely to sustain ocular injuries than females [5,6]. At the same time, data from developed countries shows that most injuries occur in the household and sports-related injuries [7-9]. In contrast, statistics from research conducted across multiple developing nations, notably India and Nepal, show that agricultural labor environments are more dangerous [10,11]. Available information indicates that eye injuries have significant consequences in terms of medical care, vocational rehabilitation needs and socioeconomic costs [12]. Prevention is crucial in addressing this problem since most ocular injuries are preventable. To effectively tackle this problem, it is necessary to understand the nature and causes of ocular trauma through epidemiological data. However, most existing studies have focused on developed countries and their findings may have limited applicability to countries like China due to various factors such as climate, geography, lifestyle and socioeconomic conditions [13]. Therefore, comprehensive epidemiological studies targeting ocular trauma in the Chinese population are needed to enable more accurate prevention and management measures planning.
Our study aims to assess ocular trauma patterns in Chinese adults using a diverse sample. This will help us understand its incidence, causes and risk factors, enabling targeted prevention efforts. These findings will impact clinical practice and public health by guiding evidence-based strategies to reduce eye injuries in China, improve outcomes and inform healthcare professionals, policymakers and public awareness campaigns.
In this study, data on ocular trauma in China was obtained from The Third Hospital of Hebei Medical University, Department of Infection, through a systematic data collection process. Adult patients diagnosed with ocular trauma who received medical care at the hospital were included in the study. Patient demographic information, including age, gender and occupation was recorded, along with details regarding the type, location, causes and laterality of ocular trauma. Specific diagnoses made by medical professionals, such as fractures and orbital injuries, were documented, as well as the duration of hospital stays as an indicator of injury severity and recovery complexity. Visual acuity measurements at admission and follow-up were collected to assess changes in vision.
The primary outcome measure in this study is hospital stay, which is defined as the duration of time a patient remains in the hospital following an eye injury. Hospital stay is measured in days and serves as a proxy for the severity and complexity of the injury and subsequent recovery. ANOVA was employed to compare hospital stays across different diagnostic categories and post-hoc tests were conducted to identify specific differences between groups. The secondary outcome measures include changes in vision acuity before and after the injury. Vision acuity refers to the clarity and sharpness of an individual's vision. The change in vision acuity were assessed by comparing the visual acuity at admission to the visual acuity at discharge or follow-up. Specific types of trauma, such as blunt trauma, chemical and burn injuries, corneal injuries, cranial nerve disorders, eyelid and conjunctival injuries, fractures and orbital injuries, iris and sclera-related diagnoses, lacrimal system-related diagnoses, lens-related diagnoses, miscellaneous diagnoses, penetrating injuries and retinal and vitreous injuries, were examined separately to determine their impact on changes in vision acuity. The secondary outcome of changes in vision acuity were analyzed using paired t-tests to compare visual acuity at admission to visual acuity at discharge or follow-up for each type of trauma.
All statistical analyses were conducted using R software (version 4.2.2). Descriptive statistics were used to summarize the baseline characteristics of the study population. Categorical variables, such as sex, occupation, injury factor, eye laterality and diagnosis, were presented as frequencies and percentages. Continuous variables, including age and hospital stay, were reported as mean values with Standard Deviations (SD). ANOVA was conducted to examine the differences in hospital stay across different diagnostic categories. Post-hoc tests were performed using the Tukey method to compare the means between different diagnostic groups. The results were summarized with the corresponding p-values. To evaluate the changes in vision acuity after injury, paired t-tests were conducted for each type of trauma. The mean change in vision acuity was calculated, along with the standard deviation. To assess the relationship between hospital, stay and various factors, univariate linear regression analyses were performed. The diagnosis variable was treated as a categorical predictor, while sex, eye laterality and visual acuity at admission were treated as binary or continuous predictors. The results of the linear regression analyses were reported as regression coefficients, 95% Confidence Intervals (CIs) and p-values. For missing data were deleted the corresponding observation. The significance level was set at p<0.05.
Baseline summary
Table 1 presents a baseline summary of the included patients in the study. A total of 11,392 patients were included in the analysis. The majority of patients were male (82.9%), with a mean age of 37.79 years (SD=15.97). Among the patients, 65.7% were farmers, while other personnel, students and work/clerical staff accounted for 8.6%, 8.6% and 16.3% of the sample, respectively. The leading causes of injury were foreign body (40.8%), fall (20.9%), fighting (17.5%) and traffic accidents (17.8%). The injured eye was predominantly the left eye (49.3%), followed by the right eye (45.8%). Fractures and orbital injuries were the most common diagnosis, accounting for 29.9% of cases. The mean hospital stay for the patients was 14.69 days (SD=13.10). Table 2 provides detailed information about the injuries across different diagnostic categories. Within each category, specific types of injuries are listed along with their corresponding frequencies (Figure 1). For example, within the category of chemical and burn injuries, acid burn, alkali burn, chemical injury and hot burn were observed with frequencies of 17.39%, 39.13%, 17.39% and 26.09%, respectively (Tables 1 and 2).
| Characteristics | Level | Overall (n=1, 1392) |
|---|---|---|
| Year (%) | 2012 | 369 (27.8) |
| 2013 | 278 (20.9) | |
| 2014 | 193 (14.5) | |
| 2015 | 229 (17.2) | |
| 2016 | 260 (19.6) | |
| Sex (%) | Female | 227 (17.1) |
| Male | 1102 (82.9) | |
| Age (mean (SD)) | - | 37.79 (15.97) |
| Occupation (%) | Farmer | 873 (65.7) |
| Other personnel | 114 ( 8.6) | |
| Student | 114 ( 8.6) | |
| Unknown | 11 ( 0.8) | |
| Work/clerk | 217 (16.3) | |
| Injury factor (%) | Fall | 278 (20.9) |
| Fighting | 233 (17.5) | |
| Foreign body | 542 (40.8) | |
| Other | 40 ( 3.0) | |
| Traffic accident | 236 (17.8) | |
| Injured eye (%) | Binoculus | 65 ( 4.9) |
| Left eye | 655 (49.3) | |
| Right eye | 609 (45.8) | |
| Diagnosis (%) | Blunt trauma | 37 ( 2.8) |
| Chemical and burn injuries | 23 ( 1.7) | |
| Corneal injury | 48 ( 3.6) | |
| Cranial nerve disorders | 88 ( 6.6) | |
| Eye lid and conjunctival injury | 89 ( 6.7) | |
| Fractures and orbital injuries | 398 (29.9) | |
| Iris and sclera-related diagnoses | 11 ( 0.8) | |
| Lacrimal system-related diagnoses | 118 ( 8.9) | |
| Lens-related diagnoses | 40 ( 3.0) | |
| Miscellaneous diagnoses | 142 (10.7) | |
| Penetrating injury | 261 (19.6) | |
| Retinal and vitreous injuries | 74 ( 5.6) | |
| Hospital stay (mean (SD)) | 14.69 (13.10) |
Note: SD: Standard Deviation.
Table 1: Baseline summary of included patients.
| Diagnosis | Variable | n (%) |
|---|---|---|
| Blunt trauma | Blunt trauma | 37 (100) |
| Chemical and burn injuries | Acid burn | 4 (17.39) |
| Alkali burn | 9 (39.13) | |
| Chemical injury | 4 (17.39) | |
| Hot burn | 6 (26.09) | |
| Corneal injury | Corneal contusion | 4 (8.33) |
| Corneal decompensation | 1 (2.08) | |
| Corneal epithelial exfoliation | 9 (18.75) | |
| Corneal foreign body | 16 (33.33) | |
| Corneal lamellar laceration | 3 (6.25) | |
| Corneal perforation | 1 (2.08) | |
| Corneal scratch | 2 (4.17) | |
| Corneal ulcer | 12 (25) | |
| Cranial nerve disorders | Abducent paralysis | 2 (2.27) |
| Facial palsy | 2 (2.27) | |
| Oculomotor palsy | 6 (6.82) | |
| Traumatic optic neuropathy | 78 (88.64) | |
| Eye lid and conjunctival injury | Cicatricial entropion | 1 (1.12) |
| Conjunctiva laceration | 7 (7.87) | |
| Eyelid contusion | 3 (3.37) | |
| Eyelid defect | 11 (12.36) | |
| Eyelid foreign body | 3 (3.37) | |
| Eyelid laceration | 55 (61.8) | |
| Medial palpebral ligament rupture | 1 (1.12) | |
| Subconjunctival hemorrhage | 1 (1.12) | |
| Symblepharon | 2 (2.25) | |
| Traumatic ptosis | 5 (5.62) | |
| Fractures and orbital injuries | Orbital apex syndrome | 5 (1.26) |
| Orbital foreign body | 13 (3.27) | |
| Orbital fracture | 380 (95.48) | |
| Iris and sclera-related diagnoses | Cyclodialysis | 2 (18.18) |
| Iridodialysis | 2 (18.18) | |
| Iris injury | 1 (9.09) | |
| Sclera rupture | 3 (27.27) | |
| Traumatic iridocyclitis | 3 (27.27) | |
| Lacrimal system-related diagnoses | Dacryoadenitis | 1 (0.85) |
| Lacrimal canaliculi laceration | 112 (94.92) | |
| Lacrimal passage obstruction | 3 (2.54) | |
| Traumatic dacryocystitis | 2 (1.69) | |
| Lens-related diagnoses | Lens dislocation | 2 (5) |
| Lens foreign body | 1 (2.5) | |
| Lens subluxation | 25 (62.5) | |
| Traumatic cataract | 12 (30) | |
| Miscellaneous diagnoses | Blast injury | 6 (4.23) |
| Crush syndrome | 1 (0.7) | |
| Electrical injury | 1 (0.7) | |
| Hyphema | 80 (56.34) | |
| Intraocular foreign body | 40 (28.17) | |
| Neovascular glaucoma | 1 (0.7) | |
| Secondary glaucoma | 11 (7.75) | |
| Snapped inferior rectus | 1 (0.7) | |
| Superior oblique paralysis | 1 (0.7) | |
| Penetrating injury | Penetrating injury | 134 (51.34) |
| Perforating injury of eyeball | 2 (0.77) | |
| Rupture of the globe | 125 (47.89) | |
| Retinal and vitreous injuries | Commototio retinae | 6 (8.11) |
| Endophthalmitis | 2 (2.7) | |
| Retinal contusion | 15 (20.27) | |
| Retinal detachment | 10 (13.51) | |
| Traumatic macular edema | 1 (1.35) | |
| Traumatic macular hole | 4 (5.41) | |
| Vitreous hemorrhage | 36 (48.65) |
Table 2: Details of injuries across different categories.
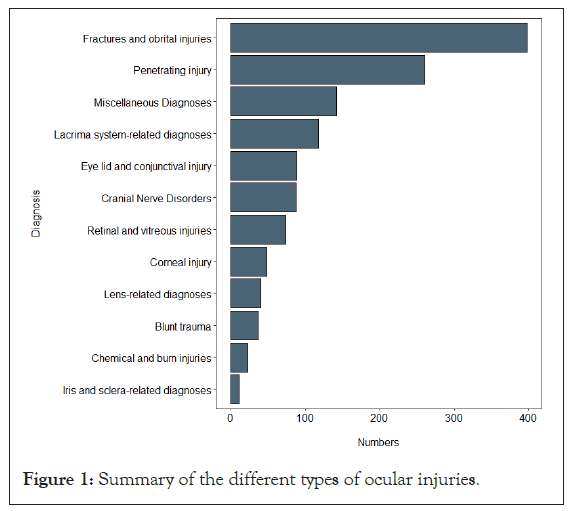
Figure 1: Summary of the different types of ocular injuries.
Stratification of hospital stay
The mean hospital stay varied significantly across different diagnoses (p<0.0001). Patients with chemical and burn injuries had the longest mean stay (21.3 days), while corneal injury cases had the shortest mean stay (10.4 days). When analyzing laterality, patients with binocular injuries had a longer mean hospital stay (19 days) compared to those with unilateral injuries (14.3 days, p=0.007). Occupation was marginally associated with hospital stay (p=0.053), with farmers having a mean stay of 14.4 days, students 12.5 days and work/clerical staff 16.2 days. The cause of injury also influenced hospital stay (p=0.0004), with fall-related injuries having the shortest mean stay (11 days) and foreign body-related injuries having the longest mean stay (15.2 days). However, there was no significant difference in mean hospital stay based on gender (p=0.51) (Table 3).
| Variable | Level | Mean hospital stay | P-value |
|---|---|---|---|
| Diagnosis | Blunt trauma | 11.1 (11.2) | <0.0001 |
| Chemical and burn injuries | 21.3 (23.4) | ||
| Corneal injury | 10.4 (6.33) | ||
| Cranial nerve disorders | 17.3 (15.3) | ||
| Eye lid and conjunctival injury | 11.3 (7.44) | ||
| Fractures and orbital injuries | 14.9 (14.8) | ||
| Iris and sclera-related diagnoses | 14.9 (9.82) | ||
| Lacrimal system-related diagnoses | 10.2 (7.05) | ||
| Lens-related diagnoses | 18.1 (20) | ||
| Miscellaneous diagnoses | 14.5 (9.66) | ||
| Penetrating injury | 16.3 (10.5) | ||
| Retinal and vitreous injuries | 16.9 (18.4) | ||
| Laterality | Binoculus | 19 (19.4) | 0.007 |
| Unilateral | 14.3 (12.8) | ||
| Occupation | Farmer | 14.4 (13.5) | 0.053 |
| Student | 12.5 (9.33) | ||
| Work/clerk | 16.2 (14.2) | ||
| Injury cause | Fall | 11 (7.70) | 0.0004 |
| Fighting | 14.2 (13.8) | ||
| Foreign body | 15.2 (12.3) | ||
| Traffic accident | 16.5 (17.9) | ||
| Gender | Female | 13 (8.23) | 0.51 |
| Male | 14.9 (14) |
Table 3: Stratification of hospital stay duration based on different variables.
Changes in vision acuity
Table 4 compares the vision acuity before and after injury across different types of trauma. Overall, there was a significant improvement in vision acuity after the injury compared to before (p<0.0001). When examining specific types of trauma, significant improvements in vision acuity were observed for blunt trauma (p=0.005), chemical and burn injuries (p=0.007), corneal injury (p<0.0001), cranial nerve disorders (p<0.0001), eye lid and conjunctival injury (p<0.0001), fractures and orbital injuries (p<0.0001), iris and sclera-related diagnoses (p=0.002), lacrimal system-related diagnoses (p<0.0001), lens-related diagnoses (p=0.001), miscellaneous diagnoses (p=0.001), penetrating injury (p<0.0001) and retinal and vitreous injuries (p<0.0001) (Figure 2 and Table 4).
| Variables | Vision acuity before | Vision acuity after | Mean difference | P-value |
|---|---|---|---|---|
| All patients | 0.41 (0.40) | 0.55 (0.39) | 0.14 | <0.0001 |
| Blunt trauma | 0.60 (0.39) | 0.74 (0.33) | 0.14 | 0.005 |
| Chemical and burn injuries | 0.24 (0.30) | 0.42 (0.41) | 0.18 | 0.007 |
| Corneal injury | 0.34 (0.28) | 0.55 (0.33) | 0.21 | <0.0001 |
| Cranial nerve disorders | 0.12 (0.23) | 0.25 (0.35) | 0.13 | <0.0001 |
| Eye lid and conjunctival injury | 0.67 (0.38) | 0.82 (0.23) | 0.15 | <0.0001 |
| Fractures and orbital injuries | 0.68 (0.34) | 0.80 (0.28) | 0.12 | <0.0001 |
| Iris and sclera-related diagnoses | 0.21 (0.21) | 0.59 (0.37) | 0.38 | 0.002 |
| Lacrimal system-related diagnoses | 0.65 (0.36) | 0.77 (0.28) | 0.12 | <0.0001 |
| Lens-related diagnoses | 0.091 (0.18) | 0.20 (0.21) | 0.1 | 0.001 |
| Miscellaneous diagnoses | 0.17 (0.28) | 0.42 (0.37) | 0.25 | 0.001 |
| Penetrating injury | 0.08 (0.19) | 0.23 (0.27) | 0.15 | <0.0001 |
| Retinal and vitreous injuries | 0.14 (0.19) | 0.33 (0.36) | 0.19 | <0.0001 |
Table 4: Comparison of vision acuity before and after injury across different types of trauma.
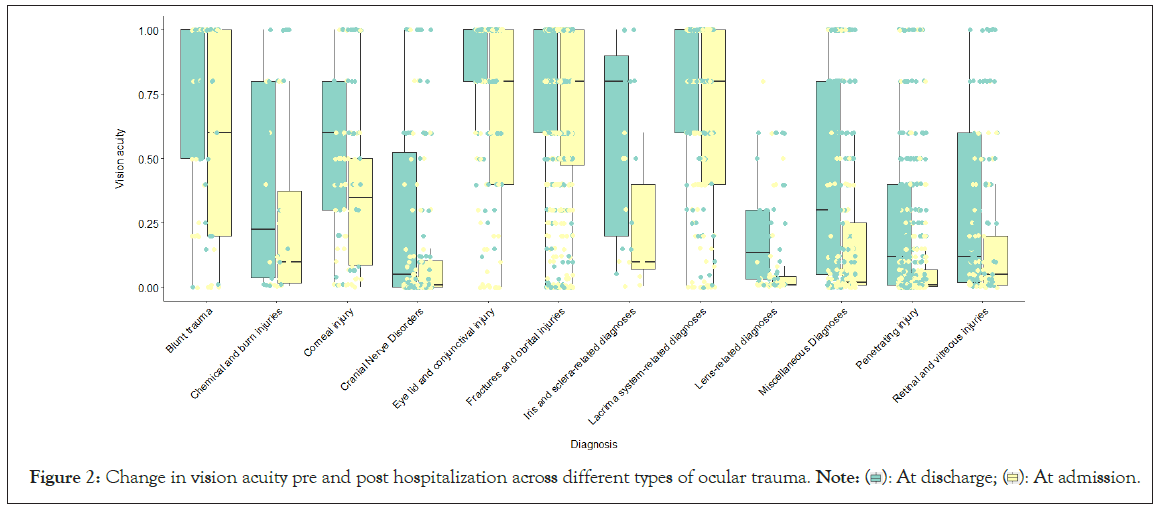
Figure 2: Change in vision acuity pre and post hospitalization across different types of ocular trauma. 
The change in vision acuity across different study variables is presented in Table 5. There was no significant difference in the mean change in vision acuity between genders (p=0.06) or occupations (p=0.86). However, the mean change varied significantly across different diagnoses (p<0.0001) and injury causes (p<0.0001). For example, patients with iris and sclerarelated diagnoses had the highest mean change in vision acuity (0.37), while those with fall-related injuries had the lowest mean change (0.09) (Table 5).
| Variable | Level | Mean change in vision acuity | P-value |
|---|---|---|---|
| Gender | Female | 0.120 (0.24) | 0.06 |
| Male | 0.157 (0.27) | ||
| Occupation | Farmer | 0.150 (0.26) | 0.86 |
| Student | 0.146 (0.26) | ||
| Work/clerk | 0.160 (0.27) | ||
| Injury factor | Fall | 0.09 (0.23) | <0.0001 |
| Fighting | 0.17 (0.27) | ||
| Foreign body | 0.19 (0.29) | ||
| Traffic accident | 0.11 (0.25) | ||
| Laterality | Binoculus | 0.18 (0.28) | 0.34 |
| Unilateral | 0.14 (0.26) | ||
| Diagnosis | Blunt trauma | 0.14 (0.28) | <0.0001 |
| Chemical and burn injuries | 0.18 (0.28) | ||
| Corneal injury | 0.21 (0.26) | ||
| Cranial nerve disorders | 0.13 (0.24) | ||
| Eye lid and conjunctival injury | 0.15 (0.32) | ||
| Fractures and orbital injuries | 0.12 (0.27) | ||
| Iris and sclera-related diagnoses | 0.37 (0.30) | ||
| Lacrimal system-related diagnoses | 0.12 (0.27) | ||
| Lens-related diagnoses | 0.11 (0.20) | ||
| Miscellaneous diagnoses | 0.25 (0.33) | ||
| Penetrating injury | 0.14 (0.21) | ||
| Retinal and vitreous injuries | 0.19 (0.27) |
Table 5: Change in vision acuity across different study variables.
Regression analysis
Univariate linear regression analysis was performed to identify factors predicting hospital stay as shown in Table 6. Male sex was associated with a longer hospital stay (coefficient=2.04, 95% CI=0.177-3.92, p=0.03). The injured eye being binocular was also associated with a longer hospital stay (coefficient=3.99, 95% CI=0.73-7.26, p=0.016). Vision acuity at admission was found to be a significant predictor of hospital stay, with poorer vision associated with longer stays (coefficient=-3.8, 95% CI=-5.59 to -2.01, p<0.001). Specific diagnoses, including chemical and burn injuries, corneal injury, eye lid and conjunctival injury and lacrimal system-related diagnoses, were found to significantly predict hospital stay (Table 6).
| Variable | Coefficient | 95% CI | P-value |
|---|---|---|---|
| Sex (male) | 2.04 | (0.177-3.92) | 0.03 |
| Age | -0.02 | (-0.063-0.024) | 0.39 |
| Injured eye (binoculus) | 3.99 | (0.73,7.26) | 0.016 |
| Vision acuity at admission | -3.8 | (-5.59,-2.01) | <0.001 |
| Fractures and orbital injuries | - | - | - |
| Blunt trauma | -4.07 | (-8.54,0.39) | 0.07 |
| Chemical and burn injuries | 6.86 | (1.24,12.47) | 0.01 |
| Corneal injury | -4.53 | (-8.52,0.53) | 0.02 |
| Cranial nerve disorders | 2.35 | (-0.68,5.37) | 0.12 |
| Eye lid and conjunctival injury | -4 | (-7.06,0.93) | 0.01 |
| Iris and sclera-related diagnoses | -0.05 | (-7.89,7.78) | 0.98 |
| Lacrimal system-related diagnoses | -4.76 | (-7.45,-2.07) | 0.0005 |
| Lens-related diagnoses | 3.14 | (-1.12,7.39) | 0.14 |
| Miscellaneous diagnoses | -0.57 | (-3.11,1.97) | 0.65 |
| Penetrating injury | 0.91 | (-1.25,3.06) | 0.4 |
| Retinal and vitreous injuries | 2.09 | (-1.21,5.40) | 0.21 |
Note: CI: Confidence Interval.
Table 6: Univariate linear regression for factors predicting hospital stay.
This study sheds new light on the epidemiology of work-related ocular injuries in China, including its rising prevalence and the leading etiologies. Such studies can identify significant risk variables that can be controlled through improved workplace safety and public health legislation. The dataset comprised information from 1,392 patients, encompassing the period from 2012 to 2016. Consistent with previous studies, our findings show a predominance of male participants, accounting for 82.9% of the sample. The mean age of the patients, as determined to be 37.79 years, implies that eye traumas can impact individuals spanning a wide range of ages. This aligns with prior research consistently demonstrating a more pronounced prevalence among young adult males. This pattern is believed to be primarily attributed to the documented scarcity of Personal Protective Equipment (PPE) usage during engagement in high-risk activities. The study findings revealed that a significant proportion of the patients, accounting for approximately 65.7% of the total sample, self-identified as farmers. This remarkable proportion strongly highlights the impact of distinctive environmental factors distinctively prevalent in China [14,15]. Consequently, this observation emphasizes the correlation between gender and injury occurrence, with males being more likely to sustain injuries that can be linked to occupational differences in risk exposure. This preference can be explained by the higher proportion of males working in hazardous professions. Nevertheless, a study aimed at accounting for occupational exposure to evaluate the risk of eye injuries in relation to gender revealed that, even after considering occupation, males still experienced higher rates of eye injuries in military settings. This suggests that occupation alone might not entirely account for the disparity in gender-associated risk for work-related eye trauma. One potential reason for this could be that young males have a lower tendency to wear sufficient eye protection compared to females. Previous research indicates that young men are less inclined to recognize the risks of dangerous behaviors and are less likely to utilize safety equipment and seat belts [16]. These findings collectively contribute to the higher occurrence of work-related eye injuries in males. The primary culprits responsible for causing eye injuries were foreign bodies, contributing to a significant 40.8% (n=542) of reported cases, followed by fighting and falls were identified as leading causes, accounting for approximately 20.9% (n=278) and 17.5% (n=233) of incidents, respectively. In contrast, a comparative study conducted in the United States reveals significantly distinct factors contributing to work-related injuries, accidental falls, motor vehicle accidents and accidental eye strikes [17]. These findings illuminate the difference between China and the United States due to the unique environmental factors prevalent in each country. Around one-third of the patients in the study exhibited fractures and orbital injuries, indicating a prevalence rate of 398 (29.9%) for fractures and 261 (19.6%) for orbital injuries. Interestingly, findings from another study conducted in Iran revealed a higher prevalence of cornea injuries, suggesting variations in the severity of injuries that could potentially be attributed to occupational factors within China [18]. These outcomes highlight the criticality of adhering to safety precautions, particularly the utilization of protective eyewear, as a means of averting such injuries.
The study revealed a mean duration of hospital stays as 14.69 days. Nonetheless, it is imperative to note that notable variations in durations were documented among different diagnoses. Interestingly, a parallel study conducted in Turkey reported a mean duration of 5 ± 3.4 days. The discrepancy in findings could potentially be attributed to the severity of possible injuries within China. Chemical and burn injuries were found to be related to the longest mean hospital stay, accounting for 23 cases (1.7%) of the study group. In contrast, corneal injuries, which accounted for 48 cases (3.6%), had the lowest mean hospital stay. The disparity in hospitalization time can be attributed to the complicated and severe nature of chemical and burn injuries.
The analysis of parameters influencing hospital stay showed some significant findings. First, male sex was related to a longer hospital stay, with a 95% confidence range ranging from 0.177 to 3.92. This shows that there may be gender disparities in injury severity or responsiveness to therapy, resulting in lengthier hospital stays for male patients. Another factor that predicted a lengthier hospital stay was that the afflicted eye was binocular. It is possible that the complexity and severity of damage to both eyes lead to the necessity for a lengthier hospital stay. Furthermore, specific diagnoses such as chemical and burn injuries, corneal injuries, eyelid and conjunctival injuries and lacrimal system-related diagnoses significantly predicted hospital stay. This emphasizes the importance of specialized care and management strategies for these conditions.
One limitation of this study is that the actual occurrence of work-related eye injuries is likely higher than what was reported, as not all injuries are severe enough to require a visit to the emergency department. However, this study does provide thorough information on various aspects of eye injuries in patients, including their characteristics, diagnosis, length of hospital stays, changes in vision and factors indicating the duration of hospitalization. These findings have important implications for preventive measures, clinical management and patient care. Further research is necessary to examine other factors and measures that might contribute to understanding and treating eye injuries.
In conclusion, our analysis identified several factors predicting hospital stay in ocular injury patients. These findings highlight the need for further investigation into gender-related differences, the impact of binocular injuries and the association between visual impairment and hospitalization duration. The results underscore the importance of tailored care for specific diagnoses requiring specialized management strategies. These findings have important implications for clinical practice and patient care. Healthcare professionals should be aware of the demographic and occupational factors that may increase the risk of eye injuries. Efforts should be made to promote preventive measures, particularly for individuals in high-risk occupations. Furthermore, individualized treatment plans and rehabilitation strategies should be developed based on the specific diagnosis and associated prognosis. Moreover, the significant improvements in vision acuity after the injury highlight the potential for visual recovery and the importance of timely and appropriate interventions. Healthcare professionals should focus on early diagnosis, prompt treatment and rehabilitation services to optimize visual outcomes for patients with eye injuries.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Miao H, Sun H, Wei X, Liu J, Jiang X, Soliman Y (2024) Epidemiological Patterns of Ocular Trauma in Adult Patients: A Comprehensive Study in China. J Clin Exp Ophthalmol. 15:980.
Received: 01-Apr-2024, Manuscript No. JCEO-24-30860; Editor assigned: 03-Apr-2024, Pre QC No. JCEO-24-30860 (PQ); Reviewed: 17-Apr-2024, QC No. JCEO-24-30860; Revised: 24-Apr-2024, Manuscript No. JCEO-24-30860 (R); Published: 02-May-2024 , DOI: 10.35248/2155-9570.24.15.980
Copyright: © 2024 Miao H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.