Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2017) Volume 5, Issue 1
Background: Most tuberculosis (TB) patients are not visiting heath facilities and hence transmit disease to healthy individuals in the community for a longer time in Ethiopia. This study was, therefore, aimed at estimating the duration of delay for initiation of anti-TB treatment in Hiwot Fana Specialized University Hospital (HFSUH) and assessing its determinants factors associated with unacceptable delay for medication.
Methods: Facility based cross sectional study was conducted in HFSUH from March 1-May 30, 2016. Convenient sampling was employed to select eligible patients who avail on time of data collection. Data was collected prospectively from 280 TB patients aged 15 years and above and who attended to the hospital using a face to face interview with a predetermined set of questions. Data was analyzed using SPSS version 16. Finally, cross tabulation and Pearson chi-square test were employed for comparison of categorical variables.
Results: A large number of extra pulmonary and smear negative pulmonary TB patients delayed more than the World Health Organization (WHO) recommended periods before taking medications. Amongst all TB patients interviewed, half (50%) of them sought treatment after WHO recommended periods (21 days). Fortunately, the median patient delay was found to be the same with WHO cut off point in this study. According to the study, the major reasons for patient delay were related to assuming symptoms are not severe (58%) followed by lack of money (32%) and health facility too far (6%). Moreover, educational status, occupation and residence were among major predictors of patient delay (p<0.05).
Conclusion: Poor knowledge of TB signs and symptoms and patients' beliefs about curses as the origin of diseases lead to delaying care-seeking at the hospital level in an area of eastern Ethiopia. These infectious TB cases are transmitting the disease to their families and in the wider community making prevention and control difficult. Those living in the rural area, illiterate and distant from health care settings suffer from TB long time and at the same time transmit the disease in the community.
<Keywords: Tuberculosis; Patient delay; Factors; Hiwot Fana hospital
According to the WHO, about 8.6 million cases were estimated to have occurred in 2012, approximately 2.9 million of whom were women. Most cases are estimated to be in Asia and Africa (58% and 27% respectively), with the highest incidence seen in India and China, together accounting for 38% of the total number of cases [1].
Like other countries, Ethiopia needs applicable information from clinical and operational studies to help the rational setting of health priorities. Tremendous effort has been made to control TB since it was declared as an emerging health problem. Early case identification and prompt treatment of the infectious cases were used as the major mechanism to prevent and control TB [2].
WHO Launched directly observed treatment short-course (DOTS), patients take anti-TB drugs under the supervision of health care providers, as the main strategy of TB control in the mid of 1900s.Ethiopia has adopted DOTS strategy as a pilot in Arise and Bale Zones of Oromia region in 1992. In 2013, geographical coverage of DOTS reached 100% while the health facility coverage is 95% [3,4].
Ethiopia was among countries which are off track to reach the millennium development goal with respect to the case detection rate. The national case detection rate in Ethiopia was 64% in 2012, decreased by 4% as compared to the case detection rate in 2011. Delayed diagnosis and treatment might be among the factors related to low case detection rate in Ethiopia in general [2].
Delayed diagnosis and initiation of anti-TB treatment increase suffering of the patient and the chance of transmission of the disease in the community. Both the health system and patient contribute to delayed diagnosis and treatment of TB [2]. Smoking cigarette also increases the delay for diagnosis and treatment as compared to nonsmokers and ex-smokers [5]. Delayed diagnosis of pulmonary TB is also associated with drug resistance as indicated in study conducted in South Africa [6]. Therefore, this study aimed at assessing determinant factors for delay in initiation of diagnosis and treatment of TB at HFSUH, Harar, Eastern Ethiopia.
Study design and setting
Health facility based cross sectional study design was employed at HFSUH from March 1-May 30, 2016. The study setting is located in Harar town, which is located 526 km from the capital of Ethiopia, Addis Ababa to the East.
Study population
All TB patients initiating treatment during the period of data collection (sputum smear positive pulmonary TB, sputum smear negative pulmonary TB and extra pulmonary TB) and registered as “new” as well as aged 15 years and above in TB clinic of HFSUH from Mar 1-May 30, 2016 were included in the study. Other categories of TB than newly registered (referred, cured, default, death --); not on treatment during the data collection period; and those who were not willing to participate were excluded.
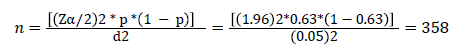
Sample size and sampling technique: The sample size was determined using the formula for estimation of single population proportion where:  at 95% CI (1.96 )d, marginal error 0.05, and, proportion obtained from a previous study in East Wollega, Ethiopia (0.63) [7].
at 95% CI (1.96 )d, marginal error 0.05, and, proportion obtained from a previous study in East Wollega, Ethiopia (0.63) [7].
Since total TB patients in HFSUH were found to be 1035 (<10,000), the final sample size was adjusted as follows.
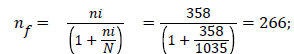 where, ni=initial sample size; nf=final sample size; N=total population.
where, ni=initial sample size; nf=final sample size; N=total population.
With 5% none response rate=266*0.05=13.3~14, the total sample size was found to be 266+14=280. Convenient sampling was employed to select eligible patients that avail on time of data collection.
Data collection tool and technique
A pre tested, questionnaire was used for data collection after getting their written consent which contains all necessary information regarding socio demographic profile, duration and reasons for patient delay. The data were collected by face to face interview using a set of questions targeting TB patients. During data collection, the English version was translated to Afan Oromo and Amharic language and back translated to keep the consistency of information gathered.
Data processing and analysis
The data were processed and analyzed using SPSS version 16. Cross tabulation followed by Pearson chi-square was applied to compare categorical variables with patient delay. When appropriate, mean ± SD was also applied. P<0.05 was considered to be statistically significant. Tables, figures and charts were used for data presentation.
Quality control
Quality of data collection was given first priority throughout the study period. These include: close monitoring of patients, interviews, cross-checking of completed questionnaires on a daily basis, and daily reviews conducted to address any difficulties encountered. To ensure the validity of the study, relevant literature was reviewed and opinions from the experts in the concerned field of TB research were obtained.
From 280 patients, 91(32.5%) were aged within 15–24 followed by those who were within 24-34 age ranges 68 (24.3%). As the age of the patient increases, the patient delay is more likely to discriminate above the WHO recommended period and this association was found to be statistically significant. This study revealed that, 154 (55%) was found to be male patients. The remaining 126 (45%) were accounted for female patients from which, 80 patients delayed above the median and the recommended cut off point. Coming to marital status of TB patients, the study showed that 215(76.8%) patients were found to be married from which 116 delayed the initiation of antiTB drugs as per the recommendation.
Regarding their residence, the finding revealed that 250 (89.3%) patients came from rural area from which 130 patients showed the delayance of initiation of antiTB medications (p<0.05). Urban dwellers were found to be 30 (10.7%) and 10 of those delayed the initiation of ant TB drugs. According to the study, farmers were found to be 232 (82.9%) and from whom 126 patients accounted for delayance (p<0.05) (Table 1).
| Socio-demographic variables | Categories | Patient delay (d) < 21 d (%) >21 d(%) Total (%) | Pearson χ2 | p –value | ||
|---|---|---|---|---|---|---|
| Sex | Female | 74(26.4) | 80(28.6) | 154(55.0) | 13.287 | 0.774 |
| Male | 66(23.6) | 60(21.4) | 126(45.0) | |||
| Age ( y) | 15-24 | 57(20.4) | 34(12.1) | 91(32.5) | ||
| 25-34 | 35(12.5) | 33(11.8) | 68(24.3) | |||
| 35-44 | 19(6.8) | 24(8.6) | 43(15.4) | |||
| 45-54 | 20(7.1) | 26(9.3) | 46(16.4) | 7.476 | 0.019* | |
| 55-64 | 9(3.2) | 16(5.7) | 25(8.9) | |||
| ≥65 | ----- | 7(2.5) | 7(2.5) | |||
| Marital status | Unmarried | 38(13.6) | 20(7.1) | 58(20.7) | ||
| Married | 99(35.4) | 116(41.4) | 215(76.8) | 5.177 | 0.521 | |
| Divorced | 1(0.4) | 2(0.7) | 3(1.1) | |||
| Widowed | 2(0.7) | 2(0.7) | 4(1.4) | |||
| Residence | Rural | 120(42.9) | 130(46.4) | 250 (89.3) | 1.644 | 0.011* |
| Urban | 20(7.1) | 10(3.6) | 30(10.7) | |||
| Occupation | Government employed | 1(0.4) | --- | 1(0.4) | ||
| Student | 14(5) | 5(1.8) | 19(6.8) | |||
| Farmer | 106(37.9) | 126(45) | 232(82.9) | 8.9 | 0.031* | |
| Others | 19(6.8) | 9(3.2) | 28(10.0) | |||
| Education | Illiterate | 102(36.4) | 120(42.9) | 222 (79.3) | 11.31 | 0.036* |
| Primary (1-8) | 31(11.1) | 17(6.1) | 48(17.2) | |||
| Senior (grade 9-12) | 2(0.7) | 1(0.4) | 3(1.1) | |||
| Higher education | 5(1.8) | 2(0.7) | 7(2.5) | |||
| Income | 97(34.6)95(33.9)192(68.6) 5.420.512 | |||||
| ≥500 ETB | 43(15.4) | 45(16.0) | 88 (31.4) | |||
| History of TB | Yes | 1(0.4) | 3(1.1) | 4 (1.4) | 4.505 | 0.609 |
| No | 139(49.6) | 137(48.9) | 276(98.6) | |||
| Ever smoke cigarette | Yes | 4(1.4) | 6(2.1) | 10 (3.6) | 1.667 | 0.797 |
| No | 136(48.6) | 134(47.9) | 270 (96.4) | |||
| Ever drunk alcohol | Yes | 3(1.1) | 3(1.1) | 6(2.2) | 5.14 | 0.526 |
| No | 137(48.9) | 137(48.9) | 274 (97.9) | |||
| HIV status | +ve | 7(2.5) | 2(0.7) | 9 (3.2) | ||
| -ve | 133(47.5) | 138(49.3) | 271(96.8) | 11.678 | 0.070 | |
| Distance (km) | 30(10.7)21(7.5)51(18.2) | |||||
| ≥10 | 110(39.3) | 119(42.5) | 229 (81.8) | 15.843 | 0.015* | |
Measurement was made by Pearson chi-square (χ2) test; p value less 0.05 was considered statistically significant (n=280).
Table 1: Socio-demographic characteristics of TB patients in relation to patient delay at HFSUH, Harar, Ethiopia, 2016 (n=280).
Concerning educational background of patients, this study revealed that 222 (79.3%) patients were found to be illiterate from which 120 patients accounted for the delayance (p<0.05). Majority of the patients 192 (68.6%) have gotalcohol from which half of the patients delayed the initiation of treatment. Coming to their HIV status, 271 (96.8%) were found to be HIV negative. Furthermore, majority of the study participants 229 (81.8%) travelled ≥10 km from which 119 patients delayed (p<0.05) (Table 1).
Generally, half (50%) of the patients delayed more than 21d, which is out of WHO recommendation whereas the rests delayed Table 2).
| Patient delay (d) | Smear+Ve PTB (%) | Smear -vePTB(%) | Extra PTB (%) | Total (%) | |
|---|---|---|---|---|---|
| ≤ 21 d | 1–7 d 8–14 d 15–21 d | ---- | ----- | ----- | ----- |
| 12(13.9) | 30(18.6) | 5(15.2) | 47(16.8) | ||
| 40(46.5 ) | 50(31.1) | 3(9.1) | 93(33.2) | ||
| Total | 52 (60.5) | 80 (49.6) | 8(24.2) | 140(50) | |
| >21 d | 22–30 d 31–60 d >60 | 14(12.3) | 36(22.4) | 9(27.3) | 59(21.1) |
| 20(16.3) | 45(27.9) | 16(48.5) | 81(28.9) | ||
| ------ | ---- | ----- | ------- | ||
| Total | 34(39.5) | 81(50.3) | 25(75.8) | 140(50) | |
Patient delay as per WHO cut off point (n=280), d=day, PTB: Pulmonary Tuberculosis, +ve: Positive, -ve: Negative
Table 2: Patient delay by TB categories in HFSUH, Harar, Ethiopia, 2016 (n=280).
According to this study, majority of the patients (58%) assumed that symptoms are not severe. Patients who delayed due to lack of money also found to be 32%. Some patients (6%) provided health facility is too far as reason for their delay. A few (2.1%) patients delay due to work load. The rest patients delayed due to inaccessibility of transport (Figure 1).
Majority of the patients (75%) went to the government hospital for the first time when they became sick. Around 17.5% patients went to the private clinic/hospital whereas 14.6% patients went to health posts. The remaining 2.9% patients went to the health center for the first time. According to this study, most of the diagnosis (97.1%) was confirmed at the government hospital. Majority of the patient (93.2%) haven't tried any option whereas 4.6% patients used medicinal plants. Moreover, majority of the TB patients 228 (81.4%) came to HFSUH after the disease became moderate (Table 3).
| Variables | Frequency | % | |
|---|---|---|---|
| First place of contact | Private clinic/ hospital Government hospital Health post Health center |
49 210 13 8 |
17.5 75.0 4.6 2.9 |
| Place of TB confirmed | Health center Government hospital NGO clinic/hospital |
5 272 3 |
1.8 97.1 1.1 |
| Treatment option | Medicinal plants Holly water I tried no option Spiritual healer |
13 4 261 2 |
4.6 1.4 93.2 0.7 |
| Severity of symptoms | Minor Moderate Severe |
13 228 39 |
4.6 81.4 13.9 |
Table 3: Patient characteristics in terms of the place of first contact, place of TB confirmed, treatment option and severity of symptoms in HFSUH, 2016.
Majority of the patients (99.3%) manifested cough more than 2 weeks. The remaining (0.7%) patients did not manifest cough. Two hundred forty one (86.1%) patients manifested prolonged fever. Patients that characterized loss of appetite and weight loss individually accounted for 87.1%. Majority of patients (84.6%) manifested shortness of breath. Patients suffered from sweating were found to be 89.6%. Moreover, patients showed chest pain were 39.3% (Table 4).
| Variables | Frequency | % | |
|---|---|---|---|
| Cough | Yes | 278 | 99.3 |
| No | 2 | 0.7 | |
| Fever | Yes | 241 | 86.1 |
| No | 39 | 13.9 | |
| Chest pain | Yes | 110 | 39.3 |
| No | 170 | 60.7 | |
| Haemoptysis | Yes | 34 | 12.1 |
| No | 246 | 87.9 | |
| Weight loss | Yes | 244 | 87.1 |
| No | 36 | 12.9 | |
| Shortness of breath | Yes | 237 | 84.6 |
| No | 43 | 15.4 | |
| Sweating | Yes | 251 | 89.6 |
| No | 29 | 10.4 | |
| Loss of appetite | Yes | 244 | 87.1 |
| No | 36 | 12.9 | |
Table 4: Frequency distribution of sign and symptoms of TB patient that they manifest in HFSUH, 2016.
According to this study, 188 (67.1%) patients believed that TB is not transmitted to the other person if one member is infected. Some (55.4%) patients believed that TB is not transmitted to the other person by using common utensils. Patients that thought TB as nontransmittable disease by living in crowded people were found to be 53.9%. The remaining 58.9% patients assumed that TB does not transmit by coughing. Besides, among respondents, 251 (89.64%) patients were ashamed when they became diagnosed with TB. Majority of the patients (81.4%) assumed TB as disease of poor (Table 5).
| Variables | Frequency | % | |
|---|---|---|---|
| By coughing | Yes | 115 | 41.1 |
| No | 165 | 58.9 | |
| Use common utensils | Yes | 125 | 44.6 |
| No | 155 | 55.4 | |
| Live in crowded | Yes | 129 | 46.1 |
| No | 151 | 53.9 | |
| If a member infected | Yes | 92 | 32.9 |
| No | 188 | 67.1 | |
| Away from/be ashamed | Yes | 251 | 89.6 |
| No | 29 | 10.4 | |
| Disease of poor | Yes | 228 | 81.4 |
| No | 52 | 18.6 | |
Table 5: Frequency distribution of knowledge,attitude and perceived sigma of patients on TB Transmission in HFSUH,2016.
Majority of the study patients, 159 (56.8%) were the reproductive age group, 15-34 years old. It was comparable to a similar study conducted in Pakistan, where 76% patients were from 15-35 years old [8].
According to this study, 154 (55%) patients were females, from which 80 patients delayed more than the median as well as WHO recommendation period. This was also comparable with the previous study conducted in Ethiopia where 54% of all TB patients were found to be females [2].
Unacceptably longer duration between the onset of TB symptoms and initiation of treatment of infectious TB patients was high in HFSUH. It is also observed that the number of days of patient delay is still much longer than the “acceptable” duration of three weeks recommended by the WHO for suspected tuberculosis cases [9]. The duration of unacceptable level of patient delay observed in this study is consistent with previous studies in Ethiopia [2,7,10] and several other countries [3,11,12], where a delay of more than three weeks was reported. They transmit the disease to the general community and their families making TB prevention and control more difficult. Patients living in the rural part of the study area and who earn 500 ETB or less Ethiopian birr per month delay longer time before taking anti-TB treatment. However, the former variable was found to be statistically significant with patient delay in this study. The median delay for initiation of treatment after recognizing TB symptoms was 21 days. This delay was significantly lower than the previous studies conducted in the Afar and Oromia regions of Ethiopia [13,14]. The possible reason for this difference might be due to the study participants had got slightly better awareness than previous studies.
Definitive diagnosis of smear negative pulmonary TB is more difficult than smear positive counter parts, making the treatment initiation delayed for a longer time [15]. What is more, extra pulmonary TB patients delayed even more than smear-ve pulmonary TB patients. This might be ascribed to the variation in the severity, onset and identifications of symptoms that are dedicated to TB case in each TB category [16]. Apart from this, most of the tuberculosis diagnosis 272 (97.1%) was confirmed at the hospital level rather than at health centers or clinics even if they are closer to the community. A similar situation was reported by another study from Ethiopia [7] where 163 (83.2%) of the diagnoses of tuberculosis were made in district hospitals. This might be due to the referral from the health center, health posts and others.
Unacceptable delay for initiation of TB treatment was higher among residents in the rural area in Ethiopia. Similarly, majority of TB patients involved in this study were from the rural parts of East Harargae. In line with the findings of the present study, inquiries made by researchers in Afghanistan [17] and Nigeria [11] had found being resident in the rural area as a risk factor for delayed initiation of treatment. There was also a statistically significant association in this study.
The main reasons for this unacceptable longer duration before treatment might be due to geographical access to health service and the cost of transportation to reach the health facility in a longer distance from their residence [4]. However, in migrant population in china, there is no association between longer delay for diagnosis and treatment and residential area. This might be due to improved income of citizens to cover the transportation cost in China [18].
From this finding, only 4 (1.4%) patients had a previous history of TB. In contrary, 54% of the patients had previous exposure to tuberculosis in Pakistan [8]. The difference might come from exclusion of newly admitted and new TB patients on treatment in the present study.
The study showed that educational status of under college level was also a predictor for patient delay. Illiterate patients and patients with eight to twelve educational statuses were more likely to delay when compared to patients with college and above educational status. This could be due to the fact that those patients who had education status of college and above level have better access for information about TB and more likely to seek medical care from healthcare facilities at an early stage of the diseases. Similar finding was also reported in previous study [14].
Majority of the patients, 151 (53.9%) believed that TB is not transmitted to the other person by living in a crowded environment. This is also consistent with the finding reported in Pakistan where 50% of cases thought that TB is not transmitted by living in a crowded environment [8].
Large number of extra pulmonary and smear negative pulmonary TB patients delayed more than the WHO cut off point before taking medications and hence render them noninfectious after a few weeks. These infectious TB cases were transmitting the disease to their families and in the wider community making prevention and control difficult. Those living in the rural area, distant from health care setting and paid the least amount of money per month suffer from TB long time and at the same time transmit the disease in the community. People living in the rural area of Harare had poor geographical access to health facilities and difficulty of the cost of transportation. These call for an improved access for diagnosis and treatment of TB in the rural community. In general, 50% of TB patients sought treatment after WHO recommended periods (21 d). In this study, educational status, residence, occupation and distance were the major predictor of patient delay.
Operational definitions
Patient delay: Time interval between onset of symptoms and presentation to a health care provider.
Smear-negative pulmonary TB (PTB): A patient who has symptoms suggestive of TB with at least 3 initial smear examinations negative for AFB by direct microscopy.
Smear-positive pulmonary TB (PTB+): A patient with at least two initial sputum smear examinations positive for AFB by direct microscopy.
Extra-pulmonary TB: A form of TB that affect organs beyond the pulmonary system.
Approval and permission was sought from Institutional Research Ethics Review Committee, College of Health and Medical Sciences, Haramaya University. Permission was also obtained from HFSUH after giving them a recommendation letter written by Haramaya University. Finally informed consent was obtained from the study participant before retrieving data and interviewing. Informed verbal consent was secured from every eligible TB patients before inclusion into the study. Privacy and confidentiality were ensured.
WB conceived the original idea, conducted the research; MS supervised the overall process and prepared this manuscript for publication. YB also reviewed it critically. All authors read and approved the final manuscript.
Competing interest
The authors have declared that there is no competing interest.
We would like to thank Haramaya University for provision of material supports. We also extend our deep appreciation for Hiwot Fana specialized university hospital staffs and administrator for their kindly support.