Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2021)Volume 11, Issue 7
Objective: Monitoring the evolution of postpartum blood pressure by conventional and ambulatory measurement of blood pressure on the one hand and proteinuria on the other hand in women who presented with gravidic hypertension and/or pre-eclampsia in two (02) university maternity hospitals of Cotonou (Benin).
Materials and methods: This was a prospective cohort study with a descriptive aim conducted over a period of six (06) months from May 1 to October 31, 2020. Pregnant women and parturients who presented with gravidic hypertension or pre-eclampsia in two university maternity hospitals were included. Blood pressure and proteinuria had been measured on the fifteenth, thirtieth, and forty-second postpartum days. An ambulatory blood pressure measurement was also performed in those in whom blood pressure remained elevated on day 42 of postpartum.
Results: The incidence of gestational hypertension and pre-eclampsia was 22.56%. The mean age of the patients was 28.96 ± 1.46 years and pregnant women aged between 20 and 30 years were the most affected by the two hypertensive disorders of pregnancy (55.7%). Blood pressure remained elevated at ambulatory measurement in 34% of cases (18/52) and significant proteinuria was found in 32.7% of cases (17/52) on day 42 of postpartumrrhea.
Conclusion: Monitoring blood pressure and proteinuria during postpartum in women with hypertensive disorders of pregnancy is necessary for the follow-up. Ambulatory blood pressure measurement is a tool to refine the diagnosis. Its use in this indication should be promoted.
In Africa, Gestational Hypertension (GHT) and Pre-Eclampsia (PE) occur in more than 10% of pregnancies and are major causes of maternal and perinatal morbidity and mortality due to their severity and complications. Blood pressure and/or proteinuria usually disappear within a few weeks in the postpartum period [1], but in some cases persist, leading to hypertensive disease. It is therefore important not only to manage these conditions adequately, but also to monitor their development in the postpartum period. Thus, a consultation is recommended three months after delivery to establish the final diagnosis (chronic hypertension, gravidic hypertension and/or pre-eclampsia), to confirm that the hypertension and proteinuria have disappeared in the absence of any treatment, and to identify the cause of the pre-eclampsia (underlying nephropathy, auto-immune disease). Few studies in Benin have addressed this issue. The objective of this study is to assess the evolution of postpartum blood pressure by conventional and Ambulatory Blood Pressure Measurement (ABPM) on the one hand, and proteinuria on the other hand, in women who presented with GHT or PE in the maternity of two university-associated hospitals in Cotonou (Benin).
Type and study period
This was a prospective descriptive cohort study conducted over a period of six (06) months from May 1 to October 31, 2020.
Population
It focused on pregnant women admitted in the delivery room of two university-associated hospitals.
Inclusion criteria
Pregnant women or parturients diagnosed with GHT or PE defined as Systolic Blood Pressure (SBP) ≥ 140 mm Hg and/or Diastolic Blood Pressure (DBP) ≥ 90 mmHg after 20 weeks of amenorrhea with or without significant proteinuria) were included in the study.
Sampling
Sampling was non-probabilistic and exhaustive, taking into account deliveries meeting the inclusion criteria. The dependent variable was postpartum hypertension and proteinuria. The nondependent variables were socio-demographic, clinical, paraclinical, and therapeutic.
Data collect
Data were collected from the respondents by interview and clinical examination. Blood Pressure (BP) and proteinuria were measured on the fifteenth, thirtieth, and forty-second days postpartum (D15, D30, and D42). An Electrocardiogram (ECG) and ABPM were performed in addition to those whose BP remained elevated at D42 postpartum. Blood pressure was measured with an Automatic Electronic Blood Pressure Monitor (OMRON) validated according to British hypertension society criteria. It was taken in seated patients after five minutes of rest; the conditions for taking BP were uniform for all patients. Proteinuria was tested with multiparametric urine strips and the result was significant for a value greater than or equal to two crosses.
Data processing and analysis were done using EPI INFO 7, Statistical Package for Social Sciences (SPSS) version 18.0, Excel 2013, and Word 2013. Simple frequency calculation was used for sample description.
During the study period, 532 women gave birth, 120 of whom presented with gravidic hypertension or pre-eclampsia, i.e. a frequency of 22.56% (09.56% for gravidic hypertension and 13% for pre-eclampsia). For various reasons, our sample consisted of 52 patients (15 cases of gravidic hypertension and 37 cases of preeclampsia).
The mean age of the patients was 28.96 ± 1.46 years with extremes of 18 and 41 years. More than half of our sample (55.17%) was between 20-30 years of age.
Table 1 shows the distribution of hypertensive disorders by age group among the respondents.
| Type of hypertension in pregnancy | Total | % | ||
|---|---|---|---|---|
| Age group | Pre-eclampsia | Gravidic HTA | ||
| ≤ 20 years | 03 | 06 | 09 | 17.3 |
| 20-30 years | 26 | 03 | 29 | 5.7 |
| 30-40 years | 07 | 06 | 13 | 25.00 |
| ≥ 40 years | 01 | 00 | 01 | 01.92 |
| Total | 37 | 15 | 52 | 100,00 |
Table 1: Distribution of hypertensive disorder in pregnancy by age group.
Pregnant women aged between 20 and 30 years were the most affected by hypertensive disorders in pregnancy with 55.7%.
The majority of patients were poor (73%) and paucigest (60%).
At admission, patients with severe hypertension were the most numerous with 80.77% for SBP ≥ 160 and 75% for DBP ≥ 110. (Table 2).
| Numbers | (%) | |
|---|---|---|
| SBP (mmHg) <140 | 04 | 7.69 |
| (140-160) | 06 | 11.54 |
| ≥ 160 | 42 | 80.77 |
| Total | 52 | 100 |
| DBP (mmHg) | ||
| <90 | 04 | 7.69 |
| (90-110) | 09 | 17.31 |
| ≥ 110 | 39 | 75 |
| Total | 52 | 100 |
Table 2: Distribution of respondents by blood pressure on admission to the delivery room.
Proteinuria has also been measured at admission on urine dipstick. It was significant (2++) in 32 patients or 61.54% of cases (Table 3).
| Proteinuria | Number | (%) |
|---|---|---|
| - | 06 | 11.54 |
| +/- | 05 | 09.62 |
| + | 09 | 17.31 |
| ++ | 16 | 30.77 |
| +++ | 16 | 30.77 |
| Total | 52 | 100 |
Table 3: Distribution of respondents according to the results of urine dipstick proteinuria on admission.
The majority of patients had received treatment based on antihypertensive drugs in mono or bitherapy (Methyl-dopa and/ or Nicardipine) by oral or parenteral route, and anticonvulsants (mainly magnesium sulphate). Cesarean section was performed in 59.62% of cases (N=31). A uterine revision was performed in 88.24% of patients (45 patients).
There was a decrease in the percentage of patients with elevated SBP or DBP between the date of delivery and D42 postpartum (80.76% to 51.92% for SBP and 92.31% to 51.92% for DBP).
In both cases, however, there was an increase in the percentage of high SBP and DBP between D30 and D42. Information on the evolution of blood pressure in the patients at D15, D30, and D42 after delivery is summarised in Table 4.
| Delivery | Day 15 | Day 30 | Day 42 | |||||
|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | |
| PAS en mmHg | ||||||||
| <140 | 10 | 19,23 | 41 | 78.84 | 42 | 80,77 | 25 | 48,08 |
| 140-160 | 38 | 73,07 | 07 | 13.46 | 07 | 13,46 | 20 | 38,46 |
| ≥ 160 | 04 | 07,69 | 04 | 07.69 | 03 | 05,77 | 07 | 13,46 |
| Total | 52 | 100,00 | 52 | 100.00 | 52 | 100,00 | 52 | 100,00 |
| PAD en mmHg | ||||||||
| <90 | 04 | 07,69 | 09 | 17.30 | 38 | 73,08 | 25 | 48,08 |
| (90-110) | 45 | 86,54 | 40 | 76.92 | 09 | 17,31 | 12 | 23,08 |
| ≥ 110 | 03 | 05,77 | 03 | 05.77 | 05 | 09,62 | 15 | 28,84 |
| Total | 52 | 100,00 | 100 | 100.00 | 52 | 100,00 | 52 | 100,00 |
Table 4: Changes in blood pressure of women in labor over time.
On Day 42, 27 patients still had high BP and received ABPM. For that patient, the mean SBP was 137 mmHg and the mean DBP was 87 mmHg over the whole day. In addition, the mean value of SBP and DBP was higher during the day than at night. Figure 1 shows the mean SBP and DBP of the patients at ABPM.
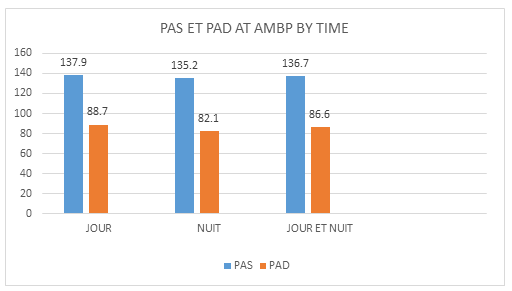
Figure 1: Distribution of patients' mean systolic and diastolic blood pressure values at ABPM by day of the week.
Of the 27 patients who underwent ABPM, 18 (66.66%) were found to have hypertension (Table 5).
| Numbers | (%) |
|
|---|---|---|
HTA systolic-diastolic |
14 |
51,85 |
HTA a dominance diastolic |
03 |
11,11 |
HTA a dominance systolic |
01 |
03,70 |
| Normal AMBP | 09 | 33,33 |
Total |
27 | 100,00 |
Table 5: Distribution of deliveries according to ABPM findings on day 42.
An increase in the number of patients with negative proteinuria was noted over time, from 61.54% at D15 to 67.3% at D30 and D42 postpartum.
The frequency of gravidic hypertension and pre-eclampsia among parturients and deliveries in the two maternity units was 22.56 (09.56% for gravidic hypertension and 13% for pre-eclampsia). According to the literature [2], the prevalence of hypertension during pregnancy varies between 10 and 15% [3]. In Africa, gestational hypertension is present in more than 10% of pregnancies. In Benin, 10% of women aged 15-49 years have high blood pressure figures according to DHS IV [4]. This relatively high frequency in our study could be explained by the fact that it was conducted in tertiary level maternity where most pathological pregnancies are referred. The difference in prevalence between countries is probably due to the mode of recruitment, the means and methods of measuring blood pressure and proteinuria, or environmental factors [5,6].
The mean age of the women in our series was 28.96 ± 1.46 years with extremes of 18 and 41 years. According to the DHS IV 2011- 2012 in Benin [4], the fertility rate increases very rapidly to reach its maximum at 25-29 years.
Our result is comparable to that of in Morocco which was 28.8 ±7 [5].
On the other hand, in Lomé found a mean age of 30 ± 7 years [7]. In our study, the majority of patients were paucigravida (60%) and pauciparous (73%).
F. Diallo in Bamako found a predominance of primigravida and large multigravida. In developed countries too, 10% to 15% of hypertension in pregnancy is found in nulliparous women. N. Chahid et al. noted a slight predominance of hypertensive disease in primiparous women (52% vs 44.3%) [8].
Patients with severe hypertension were the most numerous with 80.77% for SBP ≥ 160 and 75% for DBP ≥ 110. Many authors also found severe forms of GHT in their studies [7].
These severe forms can be explained by late diagnosis and poor compliance with treatment for various reasons (ignorance, lack of financial resources). They may also be explained by the tertiarylevel hospital nature of our study setting.
Proteinuria on urine dipstick, performed on the admission of patients, was significant (2++) in 61.54% of cases confirming the picture of pre-eclampsia for the majority of patients admitted. For it was greater than 0.3 g/24 h in the majority of pregnant women with hypertension [9]. For many authors, its appearance is a factor of poor feto-maternal prognosis [10]. According to Beaufils, the fetal risk is multiplied by 20 when hypertension is associated with proteinuria of more than 1 g per 24 hours [3].
S. Baragou in his study found that both maternal and fetal complications were often associated with proteinuria ≥ 3 g/24 h and hyperuricemia [7].
The management of the patients consisted of hospitalization and dietary advice. These measures were supplemented by drug treatment and/or obstetrical or surgical treatment. In our study, this consisted either of monotherapy (alpha methyl-dopa or nifedipine) in 60% of cases or of dual therapy (combination of two antihypertensive drugs) in 30% of cases. These drugs are the most affordable in Benin and have a good tolerance during the gravidopuerperium.
At D42 postpartum, patients with pathological blood pressure on ABPM represent 67% of our sample (N=18) of which 66.66% (N=12) were with gestational hypertension and 33.33% (N=6) with pre-eclampsia.
Ambulatory monitoring of the BP is very important because it gives a good idea of the variation in blood pressure, especially in nursing mothers who observe very little rest. Unfortunately, this device is not accessible to all social classes.
According to Beucher et al., the persistence, aggravation, or de novo appearance of arterial hypertension is to be feared in the immediate post-partum period. Among the studies that have evaluated the blood pressure evolution of pre-eclamptic women in the post-partum period, some have found an initial decrease in blood pressure immediately after delivery and then a re-ascension of the figures between the 3rd and 6th day. In an observational study of 110 women with PE, normalization of blood pressure (diastolic blood pressure <90 mmHg) occurred on average 16 days ( ± 10 days) after delivery, with the time to normalization being inversely proportional to term [8]. In another study evaluating 100 patients with severe PE, blood pressure normalization occurred in half of the cases during the first week postpartum [8].
Recently Tan, et al. studied the time to blood pressure normalization in a heterogeneous group of women with gestational hypertension or pre-eclampsia and found that for those with gestational hypertension, blood pressure normalized much faster than for those with pre-eclampsia (6 days versus 16 days) [11].
In our series, proteinuria was non-significant (<2++) in 61.54% at D15 and 67.31% at D30 and D42.
The impact of pre-eclampsia on the subsequent outcome of renal function, or in other words, the risk of renal sequelae, is extremely difficult to assess [12]. In most cases, the pre-conceptional renal status is not known, sometimes leading to the erroneous classification of persistent moderate proteinuria as a renal "sequela" of pre-eclampsia, which was in fact due to a condition preexisting during the pregnancy which itself favored the occurrence of PE (PE in addition to nephropathy). Hence the recommendation, three months after delivery, of a nephrology consultation to establish the final diagnosis (chronic hypertension, gravidic hypertension, and/ or pre-eclampsia, whether or not superadded) and to confirm that hypertension and proteinuria have disappeared in the absence of any treatment. It is also an opportunity to identify a cause for this pre-eclampsia (underlying nephropathy, auto-immune disease).
Postpartum monitoring of blood pressure and proteinuria in women with hypertensive disorders of pregnancy is necessary to establish follow-up. ABPM is an instrument to refine the diagnosis. Its use in this indication in maternity units should be promoted.
Limitation of the study
The limited duration of this study does not allow a conclusion on the final diagnosis, but it gives an idea of the evolutionary trend of these two parameters.
Citation: Aboubakar M, Dangbemey P, Tognifode MV, Ogoudjobi OM, Raimi AAN, Agbodande A, et al. (2021) Evolution Of Blood Pressure And Proteinuria in the Postpartum Period in Women With Gestational Hypertension or Pre-Eclampsia in Cotonou). Gynecol Obstet (Sunnyvale) 11:562.
Received: 22-Jul-2021 Accepted: 31-Jul-2021 Published: 07-Aug-2021
Copyright: © 2021 Aboubakar M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.