Journal of Pharmaceutical Care & Health Systems
Open Access
ISSN: 2376-0419
ISSN: 2376-0419
Research Article - (2024)Volume 11, Issue 4
This study examines the healthcare costs associated with hypertension from 2018 to 2020 using data from the Medical Expenditure Panel Survey (MEPS) supplemented by interviews with 30 participants. The findings suggest that individuals with hypertension face varying monthly treatment expenses and highlights significant disparities in out-of-pocket healthcare expenses among different racial and ethnic groups, with Black and Asian individuals tending to spend more on healthcare treatment than Hispanic and White individuals. The results underscore the challenges faced by these groups in managing the financial burden of hypertension. Furthermore, the study emphasizes the important role of health insurance in mitigating medication expenses and reducing barriers to healthcare access, with evidence suggesting that uninsured individuals face difficulty accessing healthcare services and encounter elevated healthcare costs. These findings underscore the urgent need for equality and fairness in healthcare, particularly in addressing the financial barriers faced by certain racial and ethnic groups in managing hypertension-related expenses.
Hypertension; Medical expenditure; Minority groups; Management
Hypertension (HP) is a disease that arises from elevated or High Blood Pressure (HBP). According to the World Health Organization (WHO, 2012), nearly 1 billion adults globally suffer from HP, and the incidence is rising. It is a very significant variable risk factor for Cardiovascular Diseases (CVD) around the globe. Approximately 50% of total stroke events and ischemic heart diseases are ascribed to hypertension [1-4].
Therefore, HP is a significant global health challenge and a notable cause of death among elders and impacts marginalized groups disproportionately [5-9]. Piette et al., posits that one in four adults has HP globally, and the incidence may increase by 60%, impacting about 1.5 billion individuals by 2025 [7]. Its prevalence in the United States in 2017-2018 was estimated at 45.4% and 51.0% among women and men, respectively [6]. Additionally, patients with poor information and Health Literacy (HL) cannot control chronic diseases like HP and adhere to medical directions, and minority populations are significantly impacted due to low information and health inequalities [5,9,10]. Therefore, it is essential to lower BP because it can decrease heart attack, stroke, and heart failure incidences and drastically lower healthcare costs. This study uses the Medical Expenditure Panel Survey (MEPS) and interview data to explore the medical expenditure of persons with HP. The following research question will guide this study: What are the costs associated with hypertension management?
As a risk factor, HP is of significant concern because of its connection to cerebrovascular and cardiovascular diseases [4]. It occurs when the Systolic Blood Pressure (SBP) is ≥ 130 mmHg or Diastolic Blood Pressure (DBP) is ≥ 80 mmHg. Individuals currently taking medications to lower high BP are included in this group [11]. One in every four adults suffers from HP globally, and the incidence may increase by 60%, impacting about 1.5 billion individuals by 2025 [6,7]. Moreover, it is a health concern in the US, occurring 45.4% among women and 51.0% among men [6].
Lowering blood pressure is essential to decrease heart attack, stroke, and heart failure incidences; however, this health management is important but challenging. Ostchega et al., and Nguyen et al., tested some variables, which are also influential factors of HP-low literacy/high information needs, gender, age, depressive symptoms, BP medication, medication problems, diabetes, history of myocardial infarction, median income, years of education, and Body Mass Index (BMI) [6]. Health awareness adapted to distinct social groups or communities can improve connection with health providers [12]. Likewise, the NHSR (2021) summarized HP prevalence as follows: HP rises with age amongst all adults (ages 18-39 (23.4%), 40-59 (52.4%), for 60+ (74.1%)). It was highest among non-Hispanic black adults for men and women combined (non-Hispanic black: 56.9%, non- Hispanic asian: 44.6%, non-Hispanic white: 43.5%, and Hispanic: 42.7%). Also, the incidence of HP was lowest amongst those with household income greater than 350% of the Federal Poverty Level (FPL) compared with those with household income greater than 130% through 350% FPL and was lowest amongst those with at least a college degree.
Influential factors
Studies have shown that the influential factors of HP are high salt intake, tobacco use, high intake of saturated and trans fats, diabetes, obesity, stress, lack of exercise, and elevated blood pressure [5,7,11-15]. In addition, Zhang et al., added meat intake, drinking, region, and reduced physical exercise as risk factors [15]. These factors suggest that eating habits can significantly affect HP occurrence and control. Furthermore, the severity of HP increases with age and the presence of other diseases, such as diabetes and other underlying ailments.
Symptoms and treatment of HP
High Blood Pressure (HBP) is regarded as an invisible assassin because of the absence of consistent symptoms before killing its victim. Nevertheless, a few individuals may have nosebleeds, headaches, and shortness of breath [13], and whether these are valid for the elders will be verified with the MEPS dataset.
Treatment refers to the current use of antihypertensive medications [16]. Treatment of HP reduces the risk of stroke, coronary artery disease, congestive heart failure, and cardiovascular mortality and morbidity from cardiovascular origins [17]. About 54 percent of patients with HP receive treatment, and 28 percent have sufficiently controlled BP [17]. Additionally, HP is a risk factor for stroke, congestive heart failure, dementia, myocardial infarction, renal failure, and progressive atherosclerosis.
Regular medications for HP treatment are Bay 94-8862, AR9281, Etamicastat, Alamandine, Vasomera, and some vaccines such as CYT006-AngQ. While the new drugs being introduced include inhibitors of vasopeptidases, aldosterone synthase, agonists of natriuretic peptide A and vasoactive intestinal peptide receptor-2, and a novel mineralocorticoid receptor antagonist [18,19]. While medication is a good option in hypertension treatment, lifestyle changes such as diet, exercise and stress management could also be considered [2,5,11,18,20,21]. Engaging in regular physical activity, maintaining a daily intake of balanced meals, prioritizing quality sleep, and practicing stress management can significantly improve health.
Treatment costs
HP, especially if untreated, leads to high costs borne indirectly by the entire society [3]. There are many costs related to hypertension, such as spending relating to therapy (nursing, consultations, drugs, diagnostics, hospitalization, and transport), pharmaceutical care costs, i.e., costs related to the pharmacist’s participation in the treatment, and finally, costs of stroke or other direct costs. Other costs that may be indirect include economic losses caused by diminished productivity of personnel, absence from duty caused by illness, and premature deaths [3,22]. Wierzejska et al., and colleagues conducted a systematic review to obtain a global perspective of HP annual costs globally; estimates of the mean drug costs for all the analyzed countries reveal 9,767,903,328.53 Int$ and 1,092.81 Int$ per individual [3]. Furthermore, Choromanska et al., reported that in 2016, the total indirect costs of arterial hypertension and its complications in Poland amounted to a substantial PLN 2,722,988,728.26, representing a loss of 0.14% of GDP [22]. Also, in 2017, the indirect costs totaled PLN 2,621,405,923.16, representing a loss of 0.13% of GDP. These costs, which include absenteeism, informal care, presenteeism, permanent and partial inability to work, and premature deaths, underscore the significant impact on the economy and the urgent need for action. While the costs of healthcare systems and financial barriers to healthcare are widespread, particularly among the uninsured, immigrants, lowresourced, and communities of color are disproportionately affected [18,23-25]. However, evidence suggests that insurance can significantly impact the direct cost of hypertension and healthcare in general and reduce barriers to healthcare access [26,27]. Studies have shown that racial and ethnic minorities had higher uninsured rates than non-Hispanic whites [28,29]. Nearly a third of Hispanics, one in five African Americans, and almost 17% of Asians were uninsured, compared to 11.1% of non-Hispanic whites [29]. This lack of insurance can lead to difficulty accessing healthcare services, delayed medical care, and elevated healthcare costs, highlighting the urgent need for equality and fairness in healthcare.
Method
To answer the research question, we obtained data from the Medical Expenditure Panel Survey (MEPS), a part of the Health Research and Data Quality, for our analysis. The MEPS data presents nationally representative evaluations of health care use, expenses, payment sources, and insurance coverage for the United States civilian noninstitutionalized population. The authors obtained medical conditions data covering the period from 2010 to 2020, when we started this study later years had not been uploaded on their website. Subsequently, we excluded the data from 2010 to 2017 due to the absence of direct hypertension costs and changes in certain parameters. Consequently, the focus shifted to the data from 2018 to 2020. The code for HP is 401 under the ICD09CODX coding system in the MEPS data, but I10 is under ICD10CODX. We used Microsoft Excel to obtain data on 3665 patients with HP diseases.
Our analysis was enriched by the inclusion of a range of variables that provided a comprehensive view of the factors influencing hypertension and medical spending. These variables include ADHECR42 (Rating of Health care), DUPERSID (personal ID), AGEDIAG (age at diagnosis), SEX (gender), EXRCIS53 (amount of exercise), FAMINC09 X (family income), BMINDX53 (Body mass index), ERTOTX (Emergency room visits), ADAPPT42 (visits to the medical office for care), OBVOTHX (all other visits combined), WAGEPX (personal wage income), FAMINC09 (family income), CHDDX (ever diagnosed of coronary heart disease), OHRTDX (if diagnosed with other heart diseases), ADSMOK42 (currently smoking), RXNUM (prescribed medication), NOFAT53 (Restrict High Fat/Cholesterol Food), and NOSMOK42 (Dr. advise smoking in the home is bad), ADNSK42 (Dr. Advised to quit smoking) or ADSMOK42 (currently smoking and we chose this). We performed data cleaning and processing, removed duplicates or null data, and normalized it. We also applied feature selection and evaluation metrics.
Our research was enriched by including interview data from 30 participants. This dataset was collected through purposive sampling of 30 cohorts of adults with hypertension residing in the DMV (District of Columbia, Maryland, and Virginia) area. Purposive sampling is a method for selecting individuals or groups based on specific criteria relevant to the research question [30]. This approach offers greater control over the sampling process, enabling the researchers to sample adults with hypertension that yield the most valuable information for the study. The interviews were conducted from February to April 2024 and provided real-life perspectives on the impact of hypertension on medical spending [31-34]. The MEPS data informed the interview collection phase, and the results of the analyses were compared, making this study well-integrated.
This study examines the healthcare costs associated with hypertension from 2018 to 2020 using MEPS data supplemented by interviews with 30 participants. The data extracted from MEPS contained 3665 respondents and 49 variables. Following the removal of 507 observations lacking hypertension costs, the dataset revealed that approximately 57% of the participants identified as White, 17% as Hispanic, 20% as Black, and 6% as Asian, with varying levels of educational attainment. The average family income ranged from $42,000 to $70,000 per year, with Blacks and Hispanics falling within the lower range, as illustrated in Figure 1.
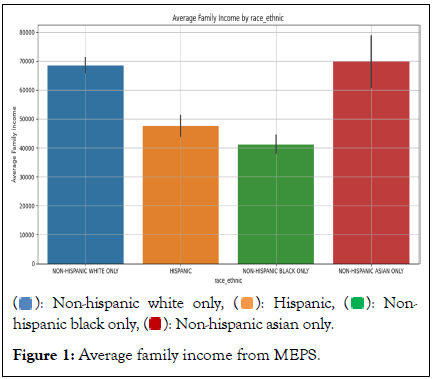
Figure 1: Average family income from MEPS.
The MEPS data indicates variations in out-of-pocket healthcare expenses by different racial and ethnic groups. According to the data, Black and Asian individuals tend to spend more annually on healthcare treatment, with amounts averaging $9,000 and$9,500, respectively. The next higher spender is Hispanic individuals spending approximately $7,500 and White individuals spending the least at $7,000 annually, as shown in Figure 2. Such significant expenses, particularly considering that they come from annual incomes ranging from a mere $42,000 to $70,000, will likely impact these individuals substantially Figure 2.
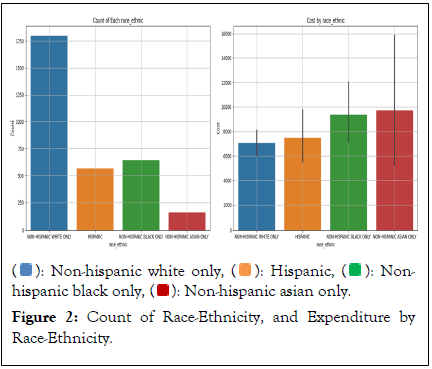
Figure 2: Count of Race-Ethnicity, and Expenditure by Race-Ethnicity.
Even though the white population is the largest in this dataset, their HP expenditure is the lowest compared to other races. This shows that minority population are disproportionately impacted by medical spending as previously noted by Bernard et al., and Jetty et al., [23,24].
As for the interview, participants were 15 (50%) females and 15 (50%) males; about 40% identified as Black, 27% as White, 23% as Hispanic, and 10% as Asian, as shown in Table 1.
| Variable | Frequency | |
|---|---|---|
| Gender | Male | 15 |
| Female | 15 | |
| Race | White | 8 |
| Black | 12 | |
| Hispanic | 7 | |
| Asian | 3 | |
Table 1: The variable and frequency of each gender.
The annual income of interview participants ranged between $50,000 and $80,000. We then conducted content analysis using grounded theory. We created a coding book and enlisted a second coder to ensure the objectivity and reliability of the coding process. Any discrepancies in the coding process were resolved through mutual agreement between the two coders and assessed the level of agreement using Cohen’s kappa [25]. The inter-coder reliability was evaluated using both percent agreement and the kappa coefficient, which was determined to be 78%, indicating substantial agreement. Participants were asked to share, on average, their HP-related expenses per month. The findings from the interviews indicate that individuals with hypertension incur varying monthly expenses on treatment, ranging from $5 to $500, depending on their insurance coverage. 65% of participants have insurance, and the remaining 35% do not. Depending on the type of insurance policies, those with insurance spend an average of $60 to $720 annually, while those without insurance face higher costs, ranging from $1,200 to $6,000 annually. Furthermore, comparing the interview findings with the MEPS revealed similar spending trends, with the MEPS showing higher expenditure levels. It suggests a correlation between the interview insights and the broader dataset. It is evident from the findings that health insurance plays a significant role in mitigating these expenses, with most participants highlighting the substantial or moderate reduction in medication costs due to insurance coverage. The dollar-specific amounts provided by participants with and without insurance are summarized on Table 2.
| Category | With insurance ($) | Without insurance ($) |
|---|---|---|
| Lowest cost | 5 | 100 |
| Mean cost | 29.19 | 250 |
| Median cost | 20 | 200 |
| Highest cost | 60 | 500 |
Table 2: HP Cost per month: With and without insurance.
Content analysis of the interview also identified some themes such as affordability, concerns, and Insurance. The majority of the participants reported manageable or minimal costs associated with insurance, providing a sense of relief. Responses mentioning affordability suggest they are not under any financial pressure with insurance. For example, Two Participants said, "Not much with insurance," three Participants said they had good insurance, "With insurance $10 to $20", and while two others said paid "Next to nothing" with insurance (about $5). However, high costs without insurance and recent changes in insurance policies are significant concerns for participants. Participants expressed concerns primarily related to changes in insurance and the high cost of medications without insurance. Common phrases indicating anxieties include:
Change in insurance and increased co-pay
Participant 5 mentioned changes in insurance policies impacting their costs. Some note that their costs have increased recently, possibly due to changes in their insurance plans.
Without insurance
When insurance is not available, high expenses are reported, indicating a significant financial burden. As previously noted by Adams et al., and Holden et al., many participants without insurance in this study were people of color [28,29].
Some of the medications they mentioned that they take daily include ace inhibitors, beta-blockers, water pills, and diuretic pills, specifically Hydrochlorothiazide, Candacearton, Losartan, Amlodipine, Benazepril, Perindoprin, olmesartan, Lisinopril, and others. Oparil et al., already identified some of these medication options [19].
Indirect costs of hypertension were found in loss of human resources, productivity, weakness, and inability to go to work or work effectively. One Participant noted, "Hypertension can be very disturbing because it can limit how much time and energy one must devote to a task. The consciousness that you should also avoid getting into stressful work where, at times, that might be needed for better productivity can also be a limitation. No matter which way it is, that, having been a potential for some time, and the cautiousness of taking care of that has reduced, or at least limited, my productivity. I have to avoid getting into work that can become very stressful and trigger a crisis? And others with the same potential, and perhaps a more serious HP that is quite uncontrollable, would not be able to do many things that they would have loved to do.” Three other Participants, such as 11, 12, and 19, supported this stance by saying they quickly have fatigue and fainting spells at work, which limit their productivity. On certain occasions, they may be unable to go to work due to excessive fatigue and fainting. Wierzejska et al., previously echoed these off-duty indirect costs [3]. Also, insurance significantly reduces average and median medication costs, reducing barriers to healthcare and limiting the range and variability of expenses, the effects that have earlier been noted by Rosendaal et al., and Fang et al., [26,27].
The study explored the impact of Hypertension (HP) on medical expenses by utilizing data from MEPS and conducting interviews. It has brought to light factors that significantly contribute to alleviating the financial burden of hypertension on individuals and families. The findings indicate that hypertension results in both direct and indirect costs. Furthermore, comparing findings from the interviews with MEPS has revealed similar spending trends, with the MEPS indicating slightly higher expenditure levels. This connection between the insights from interviews and the broader dataset has bolstered the credibility of the findings. Insurance could mitigate expenses, as most participants reported manageable or minimal insurance costs. However, the cost of insurance has not been factored into this study.
The study's findings underscore the urgent need for steady insurance policies and support programs. Participants expressed significant concerns about the high costs of healthcare without insurance and the potential impact of changes in their insurance policies, such as co-pays. This highlights the clear need for improved education on insurance benefits to empower individuals with broader knowledge and preparedness. The study's recommendations for stable and affordable insurance policies, support programs for uninsured individuals, and transparent medication pricing are important to addressing these concerns.
The study's recommendations, if implemented, have the potential to significantly improve the landscape of hypertension treatment. The government's provision of educational insurance coverage resources, society's advocacy for stable insurance policies, and the development of programs to support uninsured individuals and promote transparent medication pricing could all contribute to a more equitable and accessible healthcare system. While further research is needed to fully understand the US current spending on hypertension by race and ethnicity, these recommendations provide a promising path forward. Future research will focus on lifestyle changes in the treatment of hypertension.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Oladapo LO, Ratnam C, Bissadu K (2024). Examining Hypertension's Financial Impact: Analyzing Individual Expenditure Using MEPS and Interviews. J Pharm Care Health Syst. 11:342.
Received: 08-Aug-2024, Manuscript No. JPCHS-24-33450; Editor assigned: 12-Aug-2024, Pre QC No. JPCHS-24-33450 (PQ); Reviewed: 26-Aug-2024, QC No. JPCHS-24-33450; Revised: 02-Sep-2024, Manuscript No. JPCHS-24-33450 (R); Published: 09-Sep-2024 , DOI: 10.35248/2376-0419.24.11.342
Copyright: © 2024 Oladapo LO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.