International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
+44 1300 500008
ISSN: 2329-9096
+44 1300 500008
Research Article - (2021)
Aim: Experience of rehabilitation for patients with mild and moderate COVID-19 without remote systems. A retrospective observation study.
Background: Several studies have reported on rehabilitation for patients with COVID-19, with most studies using remote systems and focusing on patients with a severe condition. Few studies have examined rehabilitation for patients with mild or moderate conditions or considered patients’ backgrounds, including Activities of Daily Living (ADL), comorbidities, and destinations after discharge. The purpose of this study was to report an experience of rehabilitation for patients with mild and moderate COVID-19 without a remote system.
Methods: Seventeen patients with mild or moderate COVID-19 were investigated in this study (eight women and nine men). Patients’ average age at the time of admission was 65.9 years. Face-to-face rehabilitation was performed with patients who had low or decreased ability in Activities of Daily Living (ADL). We evaluated the number and rate of patients that received face- to-face rehabilitation and used the Barthel Index (BI) to evaluate patients’ Activities of Daily Living (ADL). The number and types of patients’ comorbidities and their destinations after discharge from hospital were also investigated.
Results: Five patients (29.4%) received face-to-face rehabilitation. Patients’ average BI score improved from 74.4 at admission to 84.4 at discharge. The average number of comorbidities was 2.5 per patient. These comorbidities included various diseases that negatively influenced immunity, walking ability, and Activities of Daily Living (ADL). Ten patients (58.8%) returned to their homes or a rest home after discharge.
Conclusion: Patients with COVID-19 are at high risk for decreased Activities of Daily Living (ADL). Face-to-face rehabilitation may be performed with more patients if there is appropriate protection against infection. Overall, face-to-face rehabilitation for patients with mild or moderate COVID-19 was meaningful considering the various backgrounds of patients including comorbidities. The practitioner (a rehabilitation doctor) performing face-to-face rehabilitation did not experience serious problems with their health.
Rehabilitation; Respiratory syndrome; Alzheimer’s disease; Immunity
Pneumonia from the novel coronavirus severe acute respiratory syndrome (SARS)-CoV-2 (COVID-19) was first reported in Wuhan, China, in late December 2019 [1,2]. The pandemic rapidly spread around the world, and outbreaks are continuing.
Although 1.2%-74.8% of patients with COVID-19 is reported to be asymptomatic, some patients develop a severe condition and need support from artificial ventilators and extracorporeal membrane oxygenation, with the worst cases resulting in death [3-5]. COVID-19 has shown recurrent mutations, although many governments have managed to achieve a degree of infection control based on the social condition of their country [6-10]. Japan, including Fukuoka prefecture, experienced a third wave of COVID-19 from January to March 2021.
Maintaining or recovering adequate ability in Activities of Daily Living (ADL) is important for patients with COVID-19. Guidelines for rehabilitation of patients with COVID-19 were formulated based on experience of SARS-CoV-1 and the Middle Eastern respiratory syndrome [11,12]. These guidelines recommend rehabilitation using remote systems rather than contacting patients directly, or wearing Personal Protective Equipment (PPE). However, some hospitals and facilities experienced difficulty in preparing remote systems for rehabilitation because of issues such as tight budgets. In addition, the guidelines recommended securing full-time rehabilitation staff for patients with COVID-19, and noted that these staff should not engage with patients without COVID-19 [11,13]. However, many countries are experiencing chronic shortages of medical staff, including nurses and physical therapists [14]. Hospitals and other healthcare facilities must provide care for patients with COVID-19, and need to accommodate these patients as well as other patients. Unfortunately, the number of hospitals and facilities that can provide adequate treatment for patients with COVID-19 remains limited. If physical therapists provide rehabilitation for patients with COVID-19, it may be difficult for them to continue rehabilitation work with patients without COVID-19. It would therefore be desirable if healthcare staff other than physical therapists could participate in rehabilitation for patients with COVID-19.
Several studies have reported on rehabilitation for patients with COVID-19, with most studies using remote systems and focusing on patients with a severe condition [13,15-19]. Few studies have examined rehabilitation for patients with mild or moderate conditions or considered patients’ backgrounds, including Activities of Daily Living (ADL), comorbidities, and destinations after discharge. Understanding patients’ backgrounds is important when considering their treatment and life after discharge. Therefore, the purpose of this study was to report our experience of face-to-face rehabilitation for patients with mild or moderate COVID-19 delivered by a rehabilitation doctor, and investigate Activities of Daily Living (ADL), comorbidities, and patients’ destinations after discharge.
This study included 17 patients (eight women and nine men) that had mild or moderate COVID-19 during the third wave of COVID-19 in Japan. Table 1 presents participants’ characteristics. Two patients needed total assistance in Activities of Daily Living (ADL). The average days from COVID-19 onset to hospitalization was 4.2 days (range, 0-10 days), and the average duration of hospitalization was 12.6 days (range 3-41 days). Patients’ average age at the time of admission was 65.9 years (range, 19-94 years), and the mean body mass index was 22.1 kg/m2 (range, 13.3-33.3 kg/m2). Fourteen patients were admitted following confirmation of COVID-19 by Polymerase Chain Reaction (PCR) and had been referred to the study hospital for admission by local health centers. Two patients were confirmed to be infected with COVID-19 by Polymerase Chain Reaction (PCR) at the date of or during hospitalization. The remaining patient visited the emergency room because of pyrexia and was admitted to hospital after a diagnosis of COVID-19 infection.
The degree of severity of COVID-19 was determined based on the Companion of Medical Care for COVID-19 Infection (2nd edition) published by the Japan Ministry of Health, Labour and Welfare [20]. Cases with oxygen saturation (SaO2) of ≥ 96% that were without respiratory symptoms were classified as mild irrespective of whether the patient was coughing. Cases with a SaO2 of 96%-93% and respiratory symptoms were classified as moderate grade I. Cases with a SaO2 of <93% that needed oxygen administration were classified as moderate grade II. Cases that needed artificial respiratory support were classified as severe. This study included seven mild cases, one grade I moderate case, and nine grade II moderate cases (Table 1). There were no severe cases. Quarantine ended 10 days from onset and 72 hours from symptomatic relief.
| Case | Age (years) | Sex | BMI(kg/m2) | Degree of severity | Days from onset to hospitalization | Duration of hospitalization (days) |
|---|---|---|---|---|---|---|
| 1 | 67 | M | 23.21 | Moderate Ⅱ | 3 | 11 |
| 2 | 19 | M | 29.41 | Mild | 2 | 6 |
| 3 | 65 | M | 19.91 | Moderate Ⅱ | 3 | 9 |
| 4 | 71 | F | 19.77 | Mild | 7 | 10 |
| 5 | 83 | F | 22.83 | Moderate Ⅱ | 7 | 41 |
| 6 | 94 | F | 20.73 | Mild | 7 | 4 |
| 7 | 48 | M | 33.31 | Moderate Ⅱ | 7 | 8 |
| 8 | 73 | F | 18.91 | Mild | 10 | 5 |
| 9 | 32 | F | 21.51 | Mild | 0 | 3 |
| 10 | 84 | M | 13.82 | Moderate Ⅱ | 10 | 18 |
| 11 | 88 | M | 22.23 | Mild | 4 | 13 |
| 12 | 63 | M | 25.72 | Moderate Ⅱ | 1 | 9 |
| 13 | 84 | M | 18.65 | Moderate Ⅱ | 3 | 26 |
| 14 | 86 | F | 23.31 | Moderate Ⅱ | 3 | 18 |
| 15 | 74 | F | 22.09 | Moderate Ⅱ | 1 | 12 |
| 16 | 39 | M | 23.14 | Mild | 0 | 9 |
| 17 | 50 | F | 20.72 | Moderate Ⅰ | 3 | 12 |
| Mean (range) | 69 (19-94) | 22.31 (13.82-33.31) | 4.2 (0-10) | 12.6 (3-41) |
Note: F : Female; M : Male; BMI : Body Mass Index
* Face-to-face rehabilitation was performed with the cases in italics.
Table 1: Patient’s characteristics of degree of severity determined based on the companion of medical Care for COVID 19 Infection (2nd edition) published by the Ministry of Health, Labour and Welfare, Japan. Date of onset was defined as the first day of symptoms or the date when polymerase chain reaction test results were confirmed to be positive in asymptomatic cases.
Face-to-face rehabilitation was performed with patients whose levels of Activities of Daily Living (ADL) were low or decreased as determined in informal conferences between a rehabilitation doctor (one of the present authors; SK) and on-duty doctors or nurses in the quarantine ward. All rehabilitation was performed 4-5 days per week by the same doctor (SK). During rehabilitation, care was taken to avoid face-to-face encounters with many patients with COVID-19 and staying in the red zone for a long period after patients’ Activities of Daily Living (ADL) levels were considered to be self-sustained based on the informal conferences.
The rehabilitation comprised simple, moderate exercise, which included locomotion training and rib cage stretching that were performed when the patient’s condition permitted mild exercise. Voluntary training was encouraged. Locomotion training included exercises recommended for older people by the Japanese Orthopaedic Association [21]. Range of motion training was only performed when patients were bedridden or needed heavy assistance.
We investigated the number and rate of patients that received face-to-face rehabilitation and assessed Activities of Daily Living (ADL) with the Barthel Index (BI). BI scores were evaluated based on activity during rehabilitation and clinical records. Patients that did not receive face-to-face rehabilitation were evaluated based on records completed by nurses or other medical staff. The number and types of comorbidities and patients’ destinations after discharge from hospital were retrospectively investigated. Wilcoxon signed rank test was used for the statistical analysis.
The level of significance was set at p<0.05. Informed consent was obtained on an opt-out basis. This study was conducted as a retrospective observation study .and approved by the Fukuoka University Hospital Institutional Review Board (approval number H21-05-002).
In total, five patients (29.4%) received face-to-face rehabilitation. Moderate exercises (locomotion gymnastics, rib cage stretching, and gait exercise) were performed with three patients to help prevent falls and recover their respiratory condition. Two patients received range of motion training as they needed total assistance to prevent progression to articular contracture. The average BI score for the 17 patients improved from 77.1 (range, 0-100) at admission to 84.1 (range, 0-100) at discharge from hospital (p<0.01).
The average number of comorbidities per patient was 2.5 (range, 0-5). Comorbidities that were thought to easily aggravate symptoms and cause immune deficiency were respiratory diseases including asthma and chronic obstructive pulmonary disease (n=3), diabetes mellitus (n=2), terminal renal failure with dialysis (n=2), and multiple myeloma in treatment (n=1). In addition, seven patients had orthopedic diseases including osteoporosis, lumbar compression fracture, lumbar disc herniation, osteoarthritis of the hip, and osteoarthritis of the knee. Two patients had aftereffects of cerebrovascular disease; one patient was confined to bed and the other had left hemiplegia. These nine patients had difficulties in gait or transferring to wheelchairs. Finally, three patients had psychiatric diseases (Alzheimer’s disease, alcoholism, and depression) and were considered to have difficulties in communication and compliance with quarantine.
Evaluation of discharge destinations showed that 10 patients (58.8%) could return to their homes or rest homes after discharge from hospital. Other destinations after discharge were other hospitals for treatment of comorbidities or rehabilitation (n=3), accommodation that was originally a hotel because they were mild cases (n=2), and other wards in the study hospital for treatment of comorbidities (n=2). These results are summarized in Table 2.
| Case | Number of comorbidities (comorbidities) | BI at admission | BI at discharge | Face-to-face rehabilitation | Destination after discharge | |
|---|---|---|---|---|---|---|
| 1 | 2 | (DM, dyslipidemia) | 90 | 100 | Not performed | Home |
| 2 | 0 | 100 | 100 | Not performed | Accommodation | |
| 3 | 2 | (ESRF, LDH) | 95 | 95 | Not performed | Home |
| 4 | 1 | (OH) | 90 | 90 | Not performed | Changed ward |
| 5 | 2 | (HYPO, OP) | 55 | 80 | Performed | Changed hospital |
| 6 | 3 | (HT, OP, CC) | 80 | 80 | Not performed | Rest home |
| 7 | 5 | (Asthma, DM, DP, HT, OB) | 85 | 100 | Not performed | Home |
| 8 | 0 | 85 | 100 | Not performed | Home | |
| 9 | 2 | (Dermatitis, mediastinal tumor) | 100 | 100 | Not performed | Accommodation |
| 10 | 4 | (Alcoholism, dyslipidemia, HT, OAB) | 80 | 90 | Performed | Rest home |
| 11 | 4 | (ESRF, DM, HT, dyslipidemia) | 80 | 90 | Not performed | Changed hospital |
| 12 | 3 | (AP, asthma, COPD) | 70 | 100 | Not performed | Home |
| 13* | 2 | (Aftereffect of ASH, OP) | 0 | 0 | Performed | Changed hospital |
| 14 | 4 | (COPD, DP, OP HT) | 80 | 85 | Not performed | Home |
| 15* | 4 | (AD, CC, OP, OK) | 30 | 30 | Performed | Rest home |
| 16 | 1 | (DM) | 100 | 100 | Not performed | Changed ward |
| 17 | 4 | (HT, left hemiplegia, MM, LCF) | 90 | 90 | Performed | Home |
| Mean (range) | 2.5 (0-5) | 77.1 (0-100) | 84.1 (0-100) | |||
Face-to-face rehabilitation was performed with the cases in italics.
Note: * Range of motion training only was performed
Table 2: Patient’s comorbidities, ability in activities of daily living, rehabilitation, and post-discharge destinations.
An 83-year-old woman who was usually able to walk without an aid was diagnosed with COVID-19 by Polymerase Chain Reaction (PCR) after experiencing a mild continued fever for a few days. She was segregated in accommodation that was usually used as a hotel. Her SaO2 decreased to 92% even during rest and she was admitted to the study hospital by emergency request from a local health center. A chest radiography showed bilateral diffuse interstitial shadow in the lungs (Figure 1). Oxygen administration was needed, and she was classified as a grade II moderate case. Her respiratory discomfort and fatigue were intensive and she could not move. A course of medication (mainly remdesivir (Veklury R) and steroids) was initiated, along with prone position therapy. Rehabilitation started 3 days after admission, which involved maintaining a sitting position for a few minutes with rib cage stretching. The patient had difficulty taking deep breaths and lifting her chest. Her Numerical Rating Scale score for suffocation was 8, and oxygenation of 4–5 L/min was needed after exercise. Lifting the chest and transfer to a wheelchair was possible 8 days after admission. Squats with mild knee flexion and calf raises in a standing position were initiated (one set of 10 reps each) 9 days after admission because respiratory discomfort (as a subjective complaint) was improving with acceleration, although oxygenation of 3 L/min needed to keep her SaO2 above 95%. Walking using a walker for about 20 m started 10 days after admission. The walking distance was gradually increased. She began to try to walk independently without any aid and under room air about 1 month after admission. However, her SaO2 decreased to 90% after walking 50-80 m and she received oxygenation of 1 L/min during gait exercise to ensure her safety. She was then transferred to another hospital for rehabilitation; her BI score had improved from 10 points at the start of rehabilitation to 85 points at hospital transfer (Figure 2). The report from her new hospital said that she was able to be discharged home about 3 months after onset and had achieved an independent gait for 800 m with several rests without oxygenation.
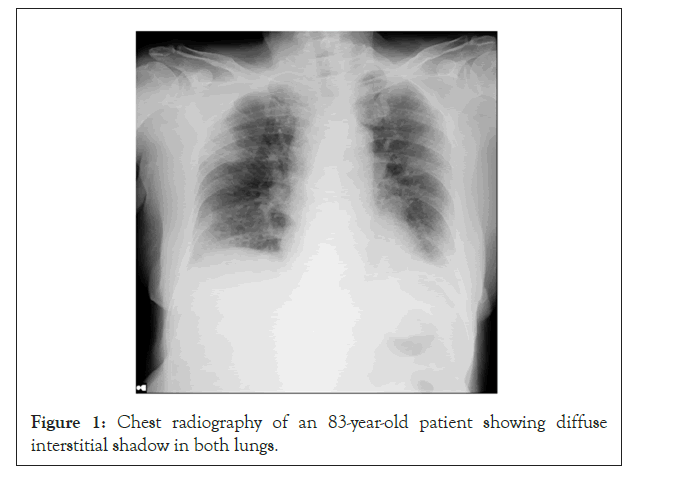
Figure 1: Chest radiography of an 83-year-old patient showing diffuse interstitial shadow in both lungs.
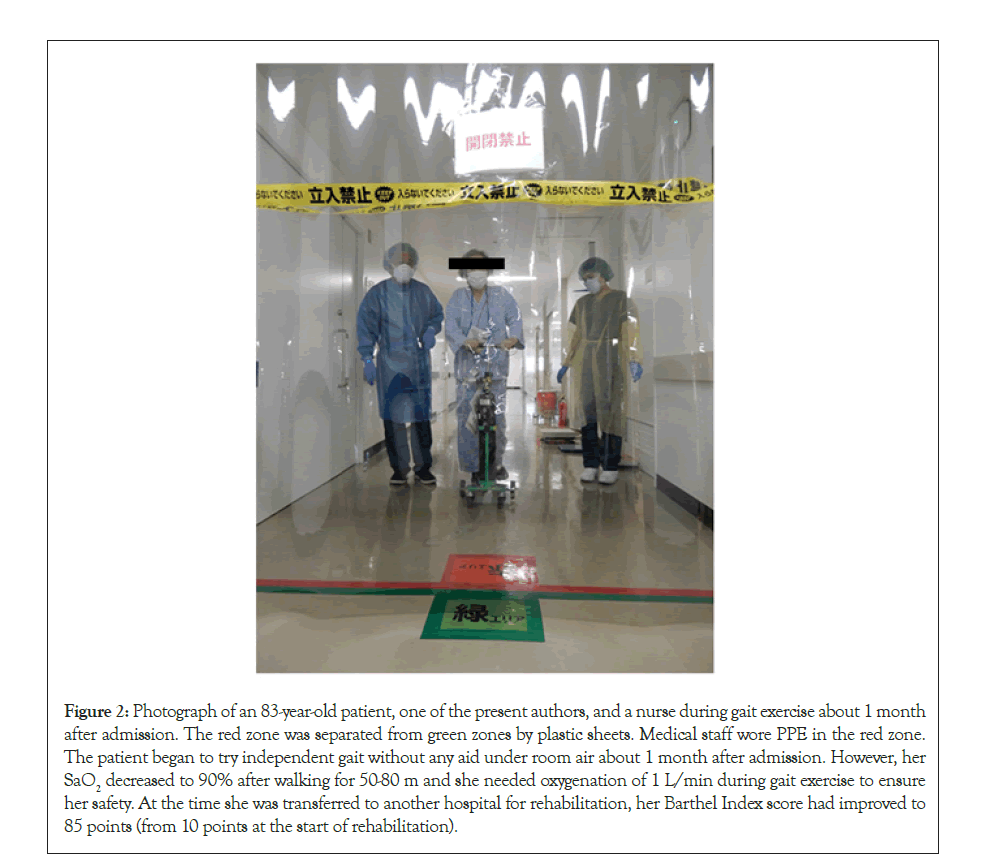
Figure 2: Photograph of an 83-year-old patient, one of the present authors, and a nurse during gait exercise about 1 month after admission. The red zone was separated from green zones by plastic sheets. Medical staff wore PPE in the red zone. The patient began to try independent gait without any aid under room air about 1 month after admission. However, her SaO2 decreased to 90% after walking for 50-80 m and she needed oxygenation of 1 L/min during gait exercise to ensure her safety. At the time she was transferred to another hospital for rehabilitation, her Barthel Index score had improved to 85 points (from 10 points at the start of rehabilitation).
This study reported our experience with face-to-face rehabilitation for patients with mild or moderate COVID-19. An important finding this study, in which only seventeen patients were included, was that patients’ backgrounds, including Activities of Daily Living (ADL) before COVID-19 infection, condition, and comorbidities, were diverse and important considerations in planning their treatment and life after discharge. This suggests that doctors from different fields should be engaged in treatment of patients with COVID-19 where possible. Many patients in this study had comorbidities that negatively influenced their immunity, walking ability, and Activities of Daily Living (ADL), and some patients were not able to perform their own care and needed support from others. Some had received rehabilitation in their daily life before COVID-19 infection through rehabilitation services, although these data were not available for all 17 patients. Patients with COVID-19 are at high risk for decreased Activities of Daily Living (ADL) and need rehabilitation. Reported that early rehabilitation and mobilization were important for patients with COVID-19 [18]. In addition, decreased Activities of Daily Living (ADL) and COVID-19 infection may create difficulties in deciding patients’ destinations after treatment and discharge. This means that preventing further decrease in Activities of Daily Living (ADL) while patients are receiving treatment for pneumonia in quarantine is important. Rehabilitation doctors could therefore play an important role in the treatment of patients with COVID-19.
In rehabilitation therapy in Japan, therapists usually provide therapy in 20-minute blocks of training, which is recognized as one unit. This means they touch patients with and without COVID-19 infection for a longer time per encounter than other medical staff. They also move between hospital wards. Rehabilitation staff therefore have a high risk for COVID-19 infection and potential to spread infection around the hospital. reported that COVID-19 therapy teams should not overlap with patients who were not infected with COVID-19 [13]. In the study hospital, physical therapists had already engaged in rehabilitation for patients with severe cases of COVID-19 in the intensive-care unit. Ensuring other full-time or dedicated physical therapists that were available for patients with mild or moderate conditions was difficult, and providing sufficient rehabilitation for all patients with COVID-19 was impossible. Negative influences to rehabilitation for patients without COVID-19 were also apprehended. Remote rehabilitation, which is considered safe in the context of COVID-19 infection and does not need full-time or dedicated physical therapists, was reported to be effective for younger patients, whereas face-to-face rehabilitation was reported to work for older patients [13]. However, remote rehabilitation requires a sufficient budget to establish (e.g., technology requirements) and may not be as effective in maintaining Activities of Daily Living (ADL) levels, especially in older patients with psychiatric diseases or who are bedridden. Ensuring the safety of staff and patients during face-to-face rehabilitation is important, but may present challenges.
Patients who received rehabilitation in this study were only able to exercise for less than 20 minutes because of breathing difficulties, fatigue, and mental problems. However, rehabilitation for mild or moderate COVID-19 cases in this study did not need specialized techniques. Rehabilitation may therefore be possible in quarantine wards, even if the practitioners are not therapists. In this study, one of the authors (SK) visited patients with mild and moderate COVID-19 in the quarantine ward, examined their conditions, and engaged in rehabilitation exercises 4–5 days per week with patients whose Activities of Daily Living (ADL) had decreased. To maintain safety, these patient encounters were scheduled at the end of each day. The main burden of treatment for patients with COVID-19 is carried by doctors in the emergency department, pulmonologists, general physicians, and nurses. However, cases with COVID-19 infection need treatment from diverse professionals beyond specific clinical departments because of their various backgrounds. Rehabilitation doctors can be meaningfully engaged in treatment of patients with COVID-19 to prevent further decrease in their Activities of Daily Living (ADL) or problems in deciding destinations after treatment and discharge. This will help to reduce the burden on staff in the COVID-19 ward, including doctors and nurses.
Interestingly, the patient described in the present case presentation could not stretch her rib cage, lift her chest, or take a deep breath well at admission. However, she could gradually perform these exercises as her Activities of Daily Living (ADL) recovered. Exercises focused on the chest may offer an index of disease condition. This is important as the use of clinical instruments and clinical examinations are restricted to the minimum in the quarantine ward to prevent the spread COVID-19, meaning there is sometimes difficulties in comprehending a patient’s condition [23,24]. For example, the disease condition may tend to remit when patients develop better ability to exercise their chest through rehabilitation, although validation of this point is needed.
There were some limitations in this study. Only five patients received face-to-face rehabilitation. This was because few patients for whom rehabilitation should be performed were identified. The stay time might at longest be sixty minutes in a time. However, inclusion of a small number of patients in rehabilitation reduced the time spent in the red zone and helped reduce the practitioner’s risk for infection with COVID-19. The practitioner in this study did not experience health problems as a result of this study. Wearing proper Personal Protective Equipment (PPE) when in the red zone, wearing a mask, washing hands frequently, and checking body temperature daily were considered important [22-24]. In Fukuoka prefecture, vaccination had not started at the beginning of the third wave of COVID-19 and many medical staff in the study hospital completed their course of vaccinations after third wave. The risk for COVID-19 infection after vaccination would decrease, although the mutated virus subsequently appeared [9,10]. Face-to-face rehabilitation may be able to include a larger number of patients if appropriate measures are implemented to protect against infection. In this study, the BI was mainly evaluated based on patients’ clinical records and number of patients was small. The evaluation of Activities of Daily Living (ADL) using B.I was just for reference. Scientific evaluations were not possible in the context of COVID-19. For example, evaluation of grip strength by hand dynamometers refrained because the use of clinical instruments in the red zone was limited to those essential for treatment. However, the background of patients in this study showed some of them potentially needed rehabilitation and the present authors believed rehabilitation, even over a short time, was meaningful because it helped to resolve problems related to patients’ destinations after discharge, and rehabilitation after quarantine could be performed seamlessly.
In this study, patients’ condition and backgrounds, including Activities of Daily Living (ADL), before COVID-19 infection were diverse. Many patients had comorbidities that negatively influenced their immunity, walking ability, and Activities of Daily Living (ADL). Face-to-face rehabilitation was meaningful, even over a short time.
The authors declare that there are no conflicts of interest.
We thank, Audrey Holmes, MA, from Edanz Group (https:// www.edanz.com/ac) for editing a draft of this manuscript.
Citation: Kamada S, Fujimi K, Shiota E, Harada T, Ishizu M, Hiyoshi T, et al. (2021) Experience of Rehabilitation for Patients with Mild and Moderate COVID-19 Without Remote Systems. Int J Phys Med Rehabil. 9:003.
Received: 30-Nov-2021 Accepted: 14-Dec-2021 Published: 21-Dec-2021
Copyright: © 2021 Kamada S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.