Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2024)Volume 15, Issue 2
Vitiligo, an autoimmune skin disorder linked to hormonal and genetic factors, results in reduced pigmentation due to a gradual decline in melanocyte activity. This systematic review delves into the role of dietary intervention and nutrition in managing vitiligo. A comprehensive search on PubMed, Google Scholar, and European PMC identified 214 studies, with 14 meeting inclusion criteria post-screening. The selected studies primarily explored the impact of dietary supplements on disease activity. Heavy metal exposure, specifically Cd, Pb, and Hg, indicated potential links to heightened reactive oxygen species and vitiligo development. Conflicting evidence emerged regarding the role of trace minerals (Zn and Cu), with some studies suggesting deficiencies and others proposing excesses in vitiligo patients. Anti-inflammatory vitamins C, D, and B12, along with antioxidants, were investigated for their potential in repigmentation strategies. Additionally, Polyunsaturated Fatty Acids (PUFAs), especially in varying types of fat consumption, were implicated. Emphasizing the need to reduce reliance on pharmacological and phototherapy interventions, the review uncovers novel roles for dietary supplements as adjuncts or flare reducers. Despite potential avenues, the review acknowledges limitations such as geographic and ethnic factors, and small sample sizes, advocating for larger-scale research to establish standardized regimes in managing vitiligo through dietary approaches.
Vitiligo; Diet; Nutrition; Autoimmune; Skin disorder
Vitiligo, a skin disorder causing the reduction of pigmentation in affected skin regions due to a gradual decline in melanocyte activity, is now widely acknowledged as an autoimmune condition linked to hormonal and genetic factors. Issues related to metabolism, oxidative stress, and cellular deterioration have also been thought to be a culprit [1]. The primary theory explaining the development of this skin disorder continues to be oxidative stress. It appears that an upsurge in oxidants, coupled with a malfunction in the body's antioxidant mechanisms, plays a pivotal role in exacerbating this condition [2]. According to Mitra, et al. [3], erythrocytes from people with active vitiligo produced much more Reactive Oxygen Species (ROS) than erythrocytes from the healthy control group. Additionally, research showed that these patients also had higher levels of lipid peroxidation, a process that increases the existence of lipid hydroperoxides and peroxyl radicals, which in turn cause oxidative damage through free radicals [3]. Global prevalence estimates for vitiligo display significant variability, with reported figures spanning from as low as 0.004% to as high as 2.28% [4].
Research focusing on dermatologic comorbidities frequently indicates a connection between this condition and conditions such as atopic dermatitis, alopecia areata, and psoriasis [5]. The direct impact of diet on this autoimmune condition has not been thoroughly examined. However, there are specific dietary guidelines that emphasize foods rich in antioxidants and nutritional value, which may be beneficial in managing the condition. Omega-6 fatty acids have the potential to boost the generation of Reactive Oxygen Species (ROS) and proinflammatory cytokines, which could potentially contribute to the development of vitiligo. Even, avoidance of common triggers might help reduce flares. In two case reports involving patients with vitiligo who had previously not shown improvement with topical agents and phototherapy, there was observed partial repigmentation following the adoption of a gluten-free diet [6]. Alpha-lipoic acid has also been identified as a suitable option and works very well in combination with the Narrow Band-Ultra Violet B (NB-UVB) light [7]. In a study conducted by Siddiqui, et al. [8], it was discovered that when phenylalanine was administered in conjunction with UV-A irradiation, nearly 94.7% of individuals displayed follicular repigmentation, and 26.3% achieved dense repigmentation. In contrast, either of these methods alone did not produce such a favorable outcome. Vitiligo is considered to be a completely reversible disease, which is rare in the autoimmune domain of diseases.
The main approach towards treatment has been from a pharmaceutical standpoint. Topical corticosteroids and calcineurin inhibitors have been found to support the repigmentation process, while systemic corticosteroid treatment effectively stabilizes highly active cases of the disease.
This has been supplemented by Psoralen Plus Ultraviolet-A radiation (PUVA) and more recently, NB-UVB which has been found to be superior to its predecessor with a notably reduced risk of skin cancer and other common adverse effects. Both these techniques focus on melanocyte proliferation [9]. There have been many studies studying the link between diet and vitiligo, which is the purpose of this systemic review. To what extent does the answer to managing vitiligo lie in dietary interventions?
Search strategy
Two independent reviewers conducted an exhaustive search across a range of electronic databases, which included PubMed, Google Scholar, and European PMC, to identify relevant studies related to the interplay between vitiligo and dietary factors. The search strategy was customised to the syntax rules of each database, utilizing Medical Subject Headings (MeSH) terms, keywords, and free-text terms combined with Boolean operators (e.g., OR, AND). Targeted filters and keywords related to vitiligo, diet, and nutrition, as well as specific dietary interventions such as antioxidants, vitamins, minerals, herbal supplements, gluten-free diets, and exclusion diets, as well as filters for specific study designs, were utilized. The entire search process was documented in adherence to the PRISMA 2020 Checklist. Search results from databases were then directly imported into Rayyan. The software helped organize these studies efficiently and remove any duplicates. The search strategy commenced in June 2023 and was successfully concluded by July 2023. A protocol was registered on PROSPERO with the registration number CRD42023464740.
Eligibility criteria
In this systematic review, we applied stringent inclusion and exclusion criteria to ensure the selection of pertinent studies for our analysis. Our inclusion criteria encompassed studies that specifically investigated the influence of diet and nutrition on vitiligo, were published in English, involving human participants, and had full-text articles accessible for review. We limited the study designs to randomized control trials and observational studies, thereby specifying research methodologies, and also imposed a time frame of 2003-2023. Our primary focus was on individuals diagnosed with vitiligo, and the intervention of interest was diet and nutrition factors. As for the comparison, we did not prescribe any specific comparison group, allowing for flexibility in the types of comparisons made across the included studies. Our main outcome of interest was the impact of diet and nutrition on vitiligo, with a particular emphasis on measurable changes such as improvements in pigmentation, reductions in lesion size, or alterations in disease progression.
In contrast, to uphold the pertinence of our systemic review, we implemented exclusion criteria. Studies not directly addressing vitiligo or those lacking a focus on diet and nutrition were omitted. We specifically limited our analysis to studies published in English to ensure consistent comprehension among reviewers. Additionally, we excluded animal or in vitro studies as they do not directly relate to the impact of diet and nutrition on human vitiligo. The exclusion of review articles, editorials, conference abstracts, and letters was also carried out to concentrate on original research. Moreover, studies lacking complete or accessible full-text articles were excluded to maintain the robustness of our ability to thoroughly assess and synthesize the findings. Through the application of these clearly defined criteria, we aimed to ensure the integrity and relevance of the studies incorporated into our systematic review.
Screening
The screening process was conducted by two independent reviewers to identify eligible studies for inclusion in this systematic review. The screening process commenced with the assessment of titles and abstracts of retrieved studies against the predefined inclusion and exclusion criteria. Rayyan, a specialized software tool, was used to facilitate and streamline the screening process. This platform allowed both the reviewers to independently assess and categorize studies as "Include," "Exclude," or "Maybe" based on the predefined criteria that unequivocally met these criteria or required further evaluation. The next stage, involved a thorough examination of the full-text articles to ascertain their alignment with the established criteria. This ensured our study was closely aligned with the precise objectives of this systemic review.
Data extraction
The primary goal of our data extraction process was to assemble an accurate dataset that would effectively address our research questions. The data extraction process was conducted by a dedicated team of three reviewers. To streamline the extraction process, we employed specialized software tools such as PDF Gear and Elicit. To ensure consistency and standardization in the information gathered, a structured data extraction form was created within Microsoft Excel software.
After the extraction process was completed, this dataset was systematically organized and the data extraction form was utilized for thorough documentation and reporting. This form covered critical data elements, including study identification details (such as title, first author, publication year, and country), methodological attributes (study design, sample size, gender distribution, mean age, participant characteristics, dietary factors, control groups, and subgroups within the study), outcome measures (both those assessed and reported), as well as a concise summary of the study itself. Data validation and quality control measures were implemented to identify and rectify errors or discrepancies. A systematic approach was followed for handling missing data and maintaining meticulous records to ensure data accuracy. We adhered to a detailed timeline, ensuring that data extraction was completed by September 9, 2023.Risk of bias assessment
The primary goal was to assess and reduce the risk of bias. Two reviewers dedicated to the assessment used the Critical Appraisal Skills Programme (CASP) tool to assess the risk through which we determined all the domains of risk assessment. The data was compiled on an Excel sheet. Any discrepancies were addressed. The CASP tool can be used to appraise systematic reviews, randomised controlled trials, cohort studies, case-control studies, economic evaluations, diagnostic studies, qualitative studies, and clinical prediction rules.
Some of the benefits of using CASP tools are to help you identify high-quality research evidence, understand the strengths and weaknesses of different research studies, assess the implications of research findings for practice, and make informed decisions about the care of your patients or clients.
Synthesis of data
The primary goal of this step is to ensure that the data collected is comparable. This was mainly done by a team of three reviewers. The data was tabulated in various categories according to first author, year, country, study design, total participants (cases/control), gender (male/female), mean age of patients, types of patients, treatment (dietary factors given to patients), control, subgroups, outcome assessed, outcome reported. The data was unified into particular sets of short codes which enabled efficient categorization and consolidation of the extracted information. The data was then visually presented in the form of pie charts, and bar diagrams.
Screening
The results were selected based on the inclusion and exclusion criteria. Any duplicate records were removed, and the automation tool Rayyan was used to screen records. Initially, there were 214 studies identified through the search string. After removing duplicates, the count was reduced to 195. Following the primary screening, 22 entries remained, and after the secondary screening, the final selection narrowed down to 14. Out of the 14 studies finalized in the secondary screening, 7 were case-control studies and 7 were cross-sectional studies (Figure 1 and Table 1).
| S.no | Study id | Year | Study design | Sample size | Age group | Gender distribution | Dietary factors |
|---|---|---|---|---|---|---|---|
| 1 | Wacewicz-Muczyńska, et al. [10] | 2020 | Case-control study | <100 | Older adults | Females>50% | Cadmium (Cd), Lead (Pb) and Mercury (Hg) |
| 2 | Soltani, et al. [11] | 2023 | Case-control study | >100 | Younger adults | Females>50% | Vitamin D |
| 3 | Singh, et al. [12] | 2012 | Case-control study | >200 | Younger adults | Females>50% | Folic acid, vitamin B12 and homocysteine |
| 4 | Narang, et al. [13] | 2021 | Cross-sectional study | >100 | Younger adults | More males in the treatment group, more females in cases | Copper (Cu) and Zinc (Zn) |
| 5 | Muawia, et al. [14] | 2020 | Case-control study | 100 | Older adults | Male>50% | Copper (Cu) |
| 6 | Sundar, et al. [15] | 2021 | Cross-sectional study | <100 | Both age groups | N/A | Folic acid, vitamin B12 and homocysteine |
| 7 | Khosdel, et al. [16] | 2022 | Case-control study | >200 | Older adults | Females>50% in both groups | Copper (Cu) and Zinc (Zn) |
| 8 | Salem, et al. [17] | 2018 | Case-control study | 100 | Older adults | Females>50% in both groups | Copper (Cu) and Zinc (Zn) |
| 9 | Mogaddam, et al. [18] | 2017 | Cross-sectional study | >100 | Younger adults | Male > 50% in both groups | Zinc (Zn) |
| 10 | Derakhshandeh-Rishehri, et al. [19] | 2019 | Cross-sectional study | >200 | Younger adults in both groups | More female in cases and more male in control group | Fatty acids |
| 11 | Garg, et al. [20] | 2019 | Cross-sectional study | <100 | Younger adults | Females>50% | Protein and adequate diet |
| 12 | Kulkarni, et al. [21] | 2016 | Cross-sectional study | <100 | Younger adults | Females>50% in both groups | Incompatible diet |
| 13 | Abdallah, et al. [22] | 2020 | Case control study | >100 for vitamin d and <100 for MSH | Older adults in both groups | Female>50% in control group and equal participants in cases | Vitamin D and alpha MSH (hormone) |
| 14 | Praneeth, et al. [23] | 2019 | Cross-sectional study | <100 | Both age groups | N/A | Zinc, copper and selenium |
Table 1: The study characteristics of the articles included in this systemic review are shown.
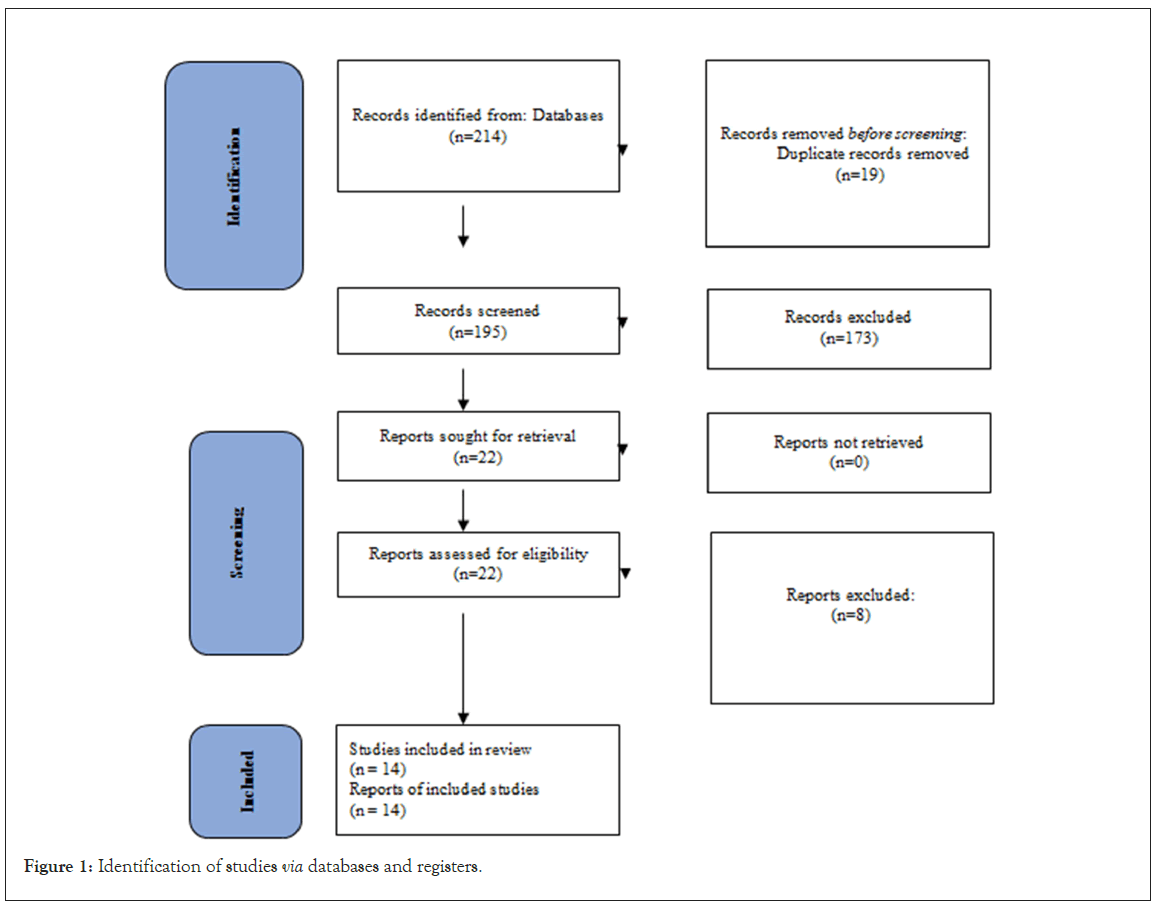
Figure 1: Identification of studies via databases and registers.
In Wacewicz-Muczyńska, et al. [10], case-control study involving older adults in which there were more females than males, the sample size being less than 100 the author found significant associations between exposure to heavy metals, specifically Cadmium (Cd), Lead (Pb), and Mercury (Hg), and adverse health outcomes. The study suggested that higher levels of these heavy metals were linked to increased health risks in the older adult population.
Soltani, et al. [11], conducted a case-control study on younger adults of which there were more females than males, with a sample size of 200, and reported an association between lower levels of vitamin D and the health outcome they investigated. This suggests that vitamin D deficiency may be a risk factor for the health condition under study in younger adults.
Singh, et al. [12], conducted a case-control study on younger adults of which there were more females, with a sample size of more than 200, and found associations between lower levels of folic acid, vitamin B12, and higher levels of homocysteine with health outcomes. This suggests that deficiencies in these nutrients may contribute to the development of the health condition in younger adults. In a cross-sectional study on younger adults, Narang, et al. [13], observed differences in Copper (Cu) and Zinc (Zn) levels between the treatment and control groups. The study noted that males were more predominant in the treatment group, while females were more prevalent in the control group, and these differences may be associated with the health outcome being studied.
Muawia, et al. [14], conducted a case-control study involving older adults with a male-predominant population, with a sample size of more than 100, and found that higher levels of Copper (Cu) were associated with health outcomes. This suggests that Copper exposure may be a risk factor for the condition in older adults, with males having a higher prevalence. The follow-up period was 4 months. Sundar, et al. [15], conducted a cross-sectional study involving both age groups with a sample size of less than 100 but did not specify a clear association. They investigated folic acid, vitamin B12, and homocysteine, indicating that further research may be needed to establish any direct links between these factors and the health outcome. The follow-up period was one year. In a case-control study on older adults with a sample size of more than 200, Khosdel, et al. [16], found associations between Copper (Cu) and Zinc (Zn) levels and health outcomes. Both cases and controls had a female predominance in their gender distribution.
Salem, et al. [17], conducted a case-control study on older adults with a sample size of 100 and reported associations between Copper (Cu) and Zinc (Zn) levels and health outcomes. The gender distribution was predominantly female. The follow-up period was 7 months.Mogaddam, et al. [18], conducted a cross-sectional study on younger adults and observed differences in Zinc (Zn) levels between groups, with a male predominance in both cases and controls, the sample size being more than 100. The study suggested that Zinc levels might be related to the health condition. In a cross-sectional study on younger adults, Derakhshandeh-Rishehri, et al. [19], found associations between fatty acids and health outcomes. Interestingly, there were differences in gender distribution between cases and control groups, with more females in cases and more males in controls with a sample size of more than 200. Garg, et al. [20], conducted a cross-sectional study on younger adults with a sample size of less than 100 and reported associations between protein intake, having an adequate diet, and health outcomes.
There was also a relation found between skipping breakfast and vitiligo. The study also had a predominantly female gender distribution. In a pilot study with a sample size of less than 100, Kulkarni, et al. [21], conducted on younger adults with a female predominance mentioned the role of an incompatible diet. The modulation of diet was significantly felt more in the control group than in the vitiligo-diseased group. However, the study did not specify a clear association with the health outcome. In this case- control study on older adults with a female predominance in a sample size of more than 100 for vitamin D and less than 100 for alpha MSH, Abdel-Rahim Abdallah, et al. [22], found associations between vitamin D levels and alpha MSH (hormone) levels with health outcomes. Female vitiligo patients had lower vitamin D levels as compared to controls but no such observation was seen in male patients.
The study reported a female predominance in the control group and an equal distribution of participants in the cases. In a case- control study done on 30 patients where the levels of Cu, Zn, and Se were estimated by using atomic absorption spectrometry, Praneeth, et al. [23], determined that vitiligo patients’ levels of serum zinc were diminished. In contrast, the level of serum copper and selenium increased. This is especially evident in severe vitiligo. However, the study did not specify a clear association with the health outcome being studied.
Risk of bias
The assessment was carried out with the help of the CASP tool checklist with the scores indicated as follows in (Table 2). A score of 0-3 indicates a high risk of bias, 4-6 a moderate risk of bias, and 7 or greater a low risk of bias. Hence all 14 of the studies chosen have a low risk of bias according to the assessment.
| S.No | Study id | ROB score |
|---|---|---|
| 1 | Wacewicz-Muczyńska, et al. (10) | 21 |
| 2 | Soltani, et al. (11) | 23 |
| 3 | Singh, et al. (12) | 14 |
| 4 | Narang, et al. (13) | 21 |
| 5 | Muawia, et al. (14) | 22 |
| 6 | Sundar, et al. (15) | 11 |
| 7 | Khosdel, et al. (16) | 19 |
| 8 | Salem, et al. (17) | 13 |
| 9 | Mogaddam, et al. (18) | 14 |
| 10 | Rishehri, et al. (19) | 21 |
| 11 | Garg, et al. (20) | 12 |
| 12 | Kulkarni, et al. (21) | 10 |
| 13 | Abdalla, et al. (22) | 15 |
| 14 | Praneeth, et al. (23) | 18 |
Table 2: The risk of bias scores.
The analyses of the relationship between diet and the pathogenesis of vitiligo hold great importance. Pharmacological and radiation therapies largely focus on the autoimmune hypothesis of this disease, and target it via an immunomodulatory approach. This includes the use of topical anti-inflammatories or immunomodulators, UV radiation, and the use of systemic corticosteroids in severe cases [24].
NB-UVB, as discussed earlier, is one of the best treatments for this disease. Its mode of action is melanocyte proliferation and works very well with adjuncts. All these therapies have still been unsuccessful in treating some of the patients suffering from this disease, which necessitates the imploration of supportive measures for treating the disease through dietary supplements and herbal adjuncts [24].
The studies included in this review largely focused on dietary supplements and how they help in controlling disease activity. Toxic heavy metals including Cd, Pb, and Hg can have negative impacts on human health even at very low concentrations [25]. These mainly exert their influence through the production of ROS and interference with key metabolic processes. Wacewicz-Muczyńska, et al. [10], through their case-control study, concluded that these heavy metals can lead to high reactive oxygen species, contributing to the development of vitiligo, and other diseases.
Micronutrients have also been a key area in which research has progressed. Tyrosinase and several other metalloenzymes involved in the biosynthesis of melanin depend on trace metals Zn and Cu as cofactors. Additionally, they are necessary cofactors for the antioxidant enzyme superoxide dismutase to function, which shields skin from reactive oxygen species [16]. Studies have shown conflicting evidence in this area. In a case-control study on older adults, Khosdel, et al. [16] found that levels of copper (Cu) and Zinc (Zn) were lower in patients suffering from the disease. Both cases and controls had a female predominance in their gender distribution in this study. The study also recommended further research into the supplementation benefits of these trace minerals. The research also concluded that the levels of Zn were less in the vitiligo group, significantly (p=0.0001). This study had a male predominance overall. Muawia, et al. [14], conducted a case-control study involving older adults and found that higher levels of Copper (Cu) were associated with the disease (case v control groups; 21.69 ± 5.17 mμol/l and 18.05 ± 3.51 mμol/l, p value=0.00001). This suggests that copper exposure may be a risk factor for the condition in older adults, with males having a higher prevalence. Narang, et al. [13], concluded that the levels of Zn were lower and the levels of Cu were higher in cases than in controls, but it also deduced that these levels were beyond the normal ranges of these trace minerals. The mean levels in the serum were significantly different from each other, between the 2 groups (p<0.001). On the other hand, some studies couldn’t establish a meaningful relationship. In a cross- sectional research covering both age groups, Praneeth, et al. [23], looked at the levels of zinc, copper, and selenium. The study could not, however, clearly identify a correlation with the health outcome. So, as we can see there is a lot of conflicting evidence, and further research is warranted to standardize treatment protocols.
Many vitamins like vitamin C, D, and B12 have been hypothesized to be anti-inflammatory and help in decreasing the ROS, furthermore helping in the management of vitiligo. One study has found that combining vitamin C and B12 with topical corticosteroids makes it an effective treatment strategy against vitiligo. Although, the role of vitamin D is seen as controversial [26]. In a pilot study, the effectiveness of high-dose oral vitamin D supplementation on vitiligo repigmentation was investigated in 16 individuals with vitamin D deficiency vitiligo. Over half of the patients experienced 26%–75% repigmentation after consuming 35,000 IU daily [27]. Supplementation is advised but dosing strategies aren’t established. A study by Sundar, et al. [15], which included both age groups, that the levels of vitamin B12 were decreased in patients who had vitiligo, with a stronger predominance for males between the cases and controls.
Even fatty acids have been thought to be beneficial for patients suffering from vitiligo. There is a significant interconnection between dietary fat and the effect it has on the modulation of our immune system. According to some findings, Saturated Fatty Acids (SFAs) were shown to have less of an immunosuppressive impact than Polyunsaturated Fatty Acids (PUFAs) [15].
A case-control study performed by Derakhshandeh-Rishehri, et al. [19], found out that a higher dietary fat intake was associated with a higher incidence risk for the development of the disease, but also stressed on the importance of the effects varying with what type of fat had been consumed (PUFA, SFA, EFA, etc.). However, a randomized controlled trial in China used a combination therapy of Alpha Lipoic Acid (ALA) alongside NB UVB in patients and found that the improvement in both the groups (cases and controls) at 1 month, 3 months, and 6 months from the initiation of therapy was statistically insignificant, even though it is well known that ALA is a potent antioxidant [28]. The limitations of this review were that it includes studies from a variety of countries, hence it is difficult to rule out geographical and ethnic factors that do play a part in disease development. Additionally, the sample sizes of the studies were small, thus reinforcing the idea of large-scale studies being conducted in the future.
Reducing the dependency on pharmacological and phototherapy interventions for vitiligo is imperative as it helps us discover newer treatment avenues. It also reveals new roles for dietary supplements, either as adjuncts with corticosteroids and/or ultraviolet therapy or to reduce disease flares. They also have lower adverse effect profiles, which can be considered as an added advantage over conventional therapies. While progress has been made, there still is a paucity of literature to establish standardized regimes of dietary interventions for patients suffering from vitiligo. Further research is warranted to discover novel techniques for managing the disease from a dietary standpoint.
Interest regarding complementary medicines and natural approaches to tackle diseases, has in general, grown over recent times. The same can be said for vitiligo. While dietary interventions cannot be thought of as a standalone therapy, they still make a case for being used as adjuncts. Many items that behave as antioxidants can be used in therapy for this disease, because of a pathophysiological nature of the disease. Further large scale clinical trials are warranted to establish strong evidence and protocols, and might also help reduce the dependency on pharmacological methods, which come with their own adverse effect profiles.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Hadi Z, Kaur R, Parekh Z, Khanna S, Khalil ABB, Abbasi HQ, et al. (2024) Exploring the Impact of Diet and Nutrition on Vitiligo: A Systematic Review of Dietary Factors and Nutritional Interventions. J Clin Exp Dermatol Res.15:661.
Received: 02-Feb-2024, Manuscript No. JCEDR-24-29035; Editor assigned: 05-Feb-2024, Pre QC No. JCEDR-24-29035 (PQ); Reviewed: 19-Feb-2024, QC No. JCEDR-24-29035; Revised: 26-Feb-2024, Manuscript No. JCEDR-24-29035 (R); Published: 04-Mar-2024 , DOI: 10.35841/2155-9554.24.15.661
Copyright: © 2024 Hadi Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.