Journal of Cancer Science and Research
Open Access
ISSN: 2576-1447
ISSN: 2576-1447
Research Article - (2023)Volume 8, Issue 2
Objective: Breast cancer is one of the most common diseases affecting women worldwide. However, mortality rates are disproportionately high among Black women, regardless of incidence rates. Although several factors related to age, steroid hormones, breastfeeding, and genetic aberrations have been implicated, the exact mechanism for this disparity remains unclear. The purpose of this study was to investigate the genetic profile of non-coding DNA sequences and determine their potential impact on breast cancer development.
Methods: Tissue samples were obtained from patients at the Joliot-Curie institute in Dakar, Senegal. Using Polymerase Reaction Chain (PCR) and the Sanger method, we sequenced Beta-Fibrinogen (FGB) intron 7 and mitochondrial D-loop region. The nucleotide sequences of both genes were then compared to reference sequences in the MITOMAP, gnomAD, and ensembl databases, and performed analyses using mutation surveyor, CADD, FATHMM-XF, CSCAPE, and CSCAPE-SOMATIC.
Results: We found 77 novel mutations in FGB and D-loop, all of which were heterozygous. The mutational spectrum of the D-loop was transition dominant, unlike that of FGB intron 7. All mutations were tolerated, with the exception of c.1244+75T>A, which was predicted to be oncogenic by cancer-specific software. Our results also indicated a strong association between the mutations in both of the genes.
Conclusion: Thus, further investigations of non-coding areas of DNA may contribute to a better understanding of the development and progression of breast cancer and lead to more effective patient management.
Breast cancer; non-coding regions; FGB; D-loop
Breast cancer is one of the leading cause of death among women worldwide [1], with approximately 7.8 million women diagnosed between 2015 and 2020 [2]. The incidence of breast cancer differs according to geographical region, socioeconomic class, ethnicity, and other factors [3]. While there is a higher rate of incidence in developed countries than in developing countries, mortality rates are higher in Asia and Africa. In addition, Black women experience worse breast cancer outcomes [4]. In most developed countries, breast cancer is associated with advanced age [5,6]. In sub-Saharan Africa, women are disproportionately diagnosed with more aggressive forms such as grade III, triple-negative breast cancer [7]. In addition, they are relatively young, with an average age at diagnosis of 40-43 years reported in Senegal [8,9]. Epidemiologic data suggest that factors such as parity status, number of pregnancies, age at menopause, and use of contraception may influence the risk of developing breast cancer.
Given that these factors affect genome integrity, thousands of studies have been conducted in this field. However, investigations of human genome alterations predominantly focused on the coding parts of genes and considered intronic and intergenic regions as ‘junk DNA’ with no obvious transcriptional utility. This resulted in an incomplete understanding of the molecular underpinnings of carcinogenesis [10]. Upon realizing that most mutations they found occurred in these areas, researchers finally began investigating their likely involvement in cancer pathophysiology. With the advent of new technologies that allow whole genome sequencing [11], studies aimed at identifying and mapping cancer-causing alterations, such as Single-Nucleotide Variants (SNVs), insertions and deletions (indels), and structural variants, including non-coding regions, have emerged [12-15]. Therefore, the purpose of this study was to determine the mutational profile of breast cancer in Senegalese women using intron 7 of the Fibrinogen Beta chain (FGB) gene and mitochondrial displacement loop (D-loop).
Patients and samples
A biopsy was performed on 115 breast cancer patients treated at the Juliot Curie institute of the hospital center university Aristide Le Dantec in Dakar, Senegal. Informed written consent was obtained from each patient before the procedure. The tissue samples were sent to the molecular biology laboratory and preserved in 95% alcohol.
DNA extraction, PCR, and sequencing of FGB and D-loop
Total DNA was extracted using the Qiagen method (Qiagen, Hilden, Germany). The extracted DNA was purified and stored at -20°C. The presence and quality of the DNA were verified by electrophoretic migration with 5 μL of DNA and 3 μL of loading blue on a 1.5% agarose gel at 100 V for 30 min. Then, the DNA fragments were visualized using ultraviolet light after passing the gel through ethidium bromide for 15 min. The D-loop and FGB in the extracted DNA were amplified using polymerase chain reaction (PCR). One forward primer pair and reverse primer pair were used for each gene. PCR was performed using a reaction volume of 50 μL for both genes with 2 μL of template DNA. Positive PCR products were purified and sequenced with forward primers using Sanger sequencing. Sequencing reactions were performed in a PTC-225 Peltier Thermal Cycler (MJ Research, Reno, NV, USA) using the ABI PRISM kit (Applied biosystems, Foster City, CA, USA).
Molecular analyses
The DNA sequencing chromatograms were analyzed using Mutation Surveyor (version 5.1.2; Soft Genetics, State College, PA, USA) to determine the presence and exact position of mutations in different genes. The algorithm compared the sample sequences to a reference sequence (GRCh38.p14) from the GenBank database (NC_000004.12 and NC_012920.1) for FGB and D-loop, respectively. The resulting variants were submitted to the Ensembl and gnomAD databases for the FGB gene and MITOMAP for the D-loop. These databases also receive complementary data of known variants from other databases, such as ClinVar, dbSNP, and ClinGen, to support genomic interpretation (Figure 1).
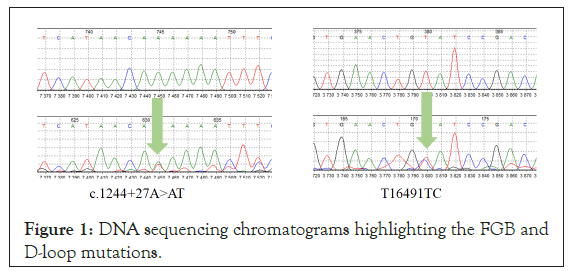
Figure 1: DNA sequencing chromatograms highlighting the FGB and D-loop mutations.
To understand the possible functional effect of the identified mutations, prediction software were used and grouped as follows: Generic (PhD-SNPg, MutationTaster2021, FATHMM- XF, and CADD) and cancer-specific (CScape, CScape-Somatic). MutationTaster2021 and CScape-Somatic are based on the GRCh37.p13 reference, which is an old version of the genome. Most non-coding gene prediction tools do not consider mitochondrial mutations due to differences in heredity, gene density, transcription machinery, and annotation availability [16]. In this study, ClinGen predictions embedded in the MITOMAP portal were the only non- coding gene prediction tools available. A mutation was considered pathogenic if it was predicted by two software programs in at least one group (generic or cancer-specific).
Statistical analysis
To determine whether there was any link between changes in the nuclear and mitochondrial genomes in breast cancer tissues, statistical tests on the FGB and D-loop mutations were performed. Fisher's exact test was used to determine whether there was an association between the two genes, and Cramer's V test was used to quantify the degree of association. The tests were performed using R software (version 2022.02.3; R Core Team, 2022) based on a null hypothesis, according to which there was no association between the FGB and D-loop mutations. The degree of significance was set at 5%.
Mutations
Four heterozygous mutations (variants) were found in the FGB sequences and one homozygous mutation with a recurrence of the c.1244+75T>A transversion. Two of the variants were recognized in the databases: c.1244+206G>A and c.1244+258A>G (Table 1).
| Position in GRCh38.p14 | Mutations | Frequency (%) | Effect on Sequence | dbSNP |
|---|---|---|---|---|
| 154569874 | c.1244+75T>A | 76 | No splicing site affected | New |
| 154569847 | c.1244+27A>T | 4 | New | |
| 154570005 | c.1244+206G>A | 4 | rs2227417 | |
| 154570057 | c.1244+258A>G | 16 | rs2227418 |
Note: GRCh38.p14: Current version of the human reference genome; dbSNP: Database of Single Nucleotide Polymorphisms.
Table 1: Nature, position, and impact of FGB mutations.
The D-loop sequences showed 127 somatic variants, of which 79 were heterozygous. Of these, 75 were novel. The variants A263G, A73G, T16519C, T152C, T195C, and C150T were the most frequent, with 10.37%, 9.98%, 6.65%, 6.26%, 5.09%, and 3.91%, respectively. Transition mutations constituted 81.6% of the variants (417/511) with more T→C changes, but the most common transition in the heterozygous variants was C→T.
Variants were found in the control region, hypervariable (HV) regions 1 and 2, -OH strand, conserved sequences blocks (CSBs) 1, 2, and 3, transcription factor (MT-TF) binding sites X, and Y, MT- HPR, and MT-3L. The control region and the MT-HV2 and heavy strand origin of replication (MT-OHR) loci were clustered with the majority of the variants. Cytidine duplications were also observed at nucleotide positions 308, 309, and 315 (Table 2).
| Mutation | Nature of mutation | Mutation status | Frequency (%) | MITOMAP | Pathogenicity | Locus (MT) |
|---|---|---|---|---|---|---|
| 4C>CT | T | Hetero | 0.2 | New | - | RC |
| 6C>CG | V | Hetero | 0.2 | New | - | RC |
| 11C>CT | T | Hetero | 0.2 | New | - | RC |
| 12T>TG | V | Hetero | 0.2 | New | - | RC |
| 26C>CG | V | Hetero | 0.2 | New | - | RC |
| 29C>T | T | Homo | 0.2 | Known | - | RC |
| 33C>CG | V | Hetero | 0.2 | New | - | RC |
| 73A>G | T | Homo | 9.98 | Known | Benign | HV2 |
| 74T>TC | T | Hetero | 0.2 | New | - | HV2 |
| 93A>G | T | Homo | 1.76 | Known | Benign | HV2 |
| 95A>C | V | Homo | 1.17 | Known | - | HV2 |
| 98C>G | V | Homo | 0.2 | Known | - | HV2 |
| 104C>CG | V | Hetero | 0.2 | New | - | HV2 |
| 127T>TC | T | Hetero | 0.2 | New | - | HV2-OHR |
| 128C>CT | T | Hetero | 0.2 | New | - | HV2-OHR |
| 143G>A | T | Homo | 0.98 | Known | Benign | HV2-OHR |
| 146T>C | T | Homo | 3.13 | Known | Benign | HV2-OHR |
| 146T>TC | T | Hetero | 0.2 | New | - | HV2-OHR |
| 150C>CT | T | Hetero | 0.39 | Known | - | HV2-OHR |
| 150C>T | T | Homo | 3.91 | Known | Benign | HV2-OHR |
| 151C>T | T | Homo | 1.37 | Known | Benign | HV2-OHR |
| 152T>C | T | Homo | 6.26 | Known | Benign | HV2-OHR |
| 152T>TC | T | Hetero | 0.2 | Known | Benign | HV2-OHR |
| 182C>T | T | Homo | 3.33 | Known | Benign | HV2-OHR |
| 183A>AG | T | Hetero | 0.39 | New | - | HV2-OHR |
| 185G>A | T | Homo | 0.39 | Known | Benign | HV2-OHR |
| 185G>C | V | Homo | 0.59 | Known | - | HV2-OHR |
| 185G>T | V | Homo | 0.98 | Known | Benign | HV2-OHR |
| 186C>A | V | Homo | 0.59 | Known | Benign | HV2-OHR |
| 189A>C | V | Homo | 0.59 | Known | Benign | HV2-OHR |
| 189A>G | T | Homo | 0.39 | Known | Benign | HV2-OHR |
| 195T>C | T | Homo | 5.09 | Known | Benign | HV2-OHR |
| 195T>TC | T | Hetero | 0.2 | Known | - | HV2-OHR |
| 198C>CT | T | Hetero | 0.2 | New | - | HV2-OHR |
| 198C>T | T | Homo | 2.15 | Known | Benign | HV2-OHR |
| 204T>C | T | Homo | 1.37 | Known | Benign | HV2-OHR |
| 207G>A | T | Homo | 1.37 | Known | Benign | HV2-OHR |
| 228G>T | V | Homo | 0.2 | Known | - | HV2-OHR-CSB1 |
| 232A>AC | V | Hetero | 0.2 | New | - | HV2-OHR-CSB1 |
| 242C>CT | T | Hetero | 0.2 | New | - | HV2-OHR-TFX |
| 247G>A | T | Homo | 1.17 | Known | Benign | HV2-OHR-TFX |
| 258C>CG | V | Hetero | 0.2 | New | - | HV2-OHR-TFX |
| 263A>AG | T | Hetero | 0.2 | New | - | HV2-OHR |
| 263A>G | T | Homo | 10.37 | Known | Benign | HV2-OHR |
| 279T>C | T | Homo | 0.39 | Known | - | HV2-OHR-TFY |
| 292T>A | V | Homo | 0.39 | Known | - | HV2-OHR-TFY |
| 292T>C | T | Homo | 0.39 | Known | - | HV2-OHR-TFY |
| 292T>TC | T | Hetero | 0.2 | New | - | HV2-OHR-TFY |
| 294T>TC | T | Hetero | 0.2 | New | - | HV2-OHR-TFY |
| 297A>G | T | Homo | 0.39 | Known | Benign | HV2-OHR-TFY |
| 303C>CA | V | Hetero | 0.59 | New | - | HV2-OHR-TFY |
| 308_309dupCC | D | - | 0.39 | Known | - | HV2-OHR-CSB2 |
| 309C>T | T | Homo | 0.2 | Known | Benign | HV2-OHR-CSB2 |
| 309dupC | D | - | 0.2 | Known | - | HV2-OHR-CSB2 |
| 310T>C | T | Homo | 0.2 | Known | Benign | HV2 |
| 310T>TA | V | Hetero | 0.59 | New | - | HV2-OHR-CSB2 |
| 315dupC | D | - | 0.2 | Known | - | HV2-OHR-CSB2 |
| 316G>A | T | Homo | 0.78 | Known | Benign | HV2-OHR-HPR |
| 316G>C | V | Homo | 0.2 | Known | - | HV2-OHR-HPR |
| 320C>A | V | Homo | 0.2 | Known | - | HV2-OHR-HPR |
| 321T>TA | V | Hetero | 0.2 | New | - | HV2-OHR |
| 322G>GA | T | Hetero | 0.2 | New | - | HV2-OHR |
| 324C>CG | V | Hetero | 0.2 | New | - | HV2-OHR |
| 324C>G | V | Homo | 0.2 | Known | - | HV2-OHR |
| 325C>CG | V | Hetero | 0.2 | New | - | HV2-OHR |
| 325C>T | T | Homo | 0.98 | Known | Benign | HV2-OHR |
| 326A>AG | T | Hetero | 0.2 | New | - | HV2-OHR |
| 338C>CT | T | Hetero | 0.2 | New | - | HV2-OHR |
| 345C>CA | V | Hetero | 0.78 | New | - | HV2-OHR |
| 345C>CT | T | Hetero | 0.2 | New | - | HV2-OHR |
| 357A>G | T | Homo | 1,17 | Known | Benign | HV2-OHR-CSB3 |
| 366G>GA | T | Hetero | 0.2 | New | - | HV2-OHR |
| 16326A>AT | V | Hetero | 0.2 | New | - | HV1 |
| 16326A>T | V | Homo | 0.2 | Known | - | HV1 |
| 16327C>T | T | Homo | 0.2 | Known | Benign | HV1 |
| 16335A>AT | V | Hetero | 0.2 | New | - | HV1 |
| 16336G>GT | V | Hetero | 0.39 | New | - | HV1 |
| 16337C>CT | T | Hetero | 0.39 | New | - | HV1 |
| 16338A>AT | V | Hetero | 0.39 | New | - | HV1 |
| 16339C>CT | T | Hetero | 0.78 | New | - | HV1 |
| 16340A>AT | V | Hetero | 0.59 | New | - | HV1 |
| 16341T>TG | V | Hetero | 0.59 | New | - | HV1 |
| 16343A>AT | V | Hetero | 0.59 | New | - | HV1 |
| 16344C>CT | T | Hetero | 0.39 | New | - | HV1 |
| 16355C>CT | T | Hetero | 0.98 | New | - | HV1 |
| 16355C>T | T | Homo | 0.59 | Known | Benign | HV1 |
| 16359T>TG | V | Hetero | 0.2 | New | - | HV1 |
| 16360C>CT | T | Hetero | 0.2 | New | - | HV1 |
| 16360C>T | T | Homo | 0.2 | Known | Benign | HV1 |
| 16362T>C | T | Homo | 2.74 | Known | Benign | HV1 |
| 16364C>CG | V | Hetero | 0.39 | New | - | HV1 |
| 16376C>CT | T | Hetero | 0.2 | New | - | HV1 |
| 16378C>CT | T | Hetero | 0.59 | New | - | HV1 |
| 16380C>CT | T | Hetero | 0.2 | New | - | HV1 |
| 16385A>AG | T | Hetero | 0.2 | Known | - | RC |
| 16386T>TG | V | Hetero | 0.2 | New | - | RC |
| 16387A>AG | T | Hetero | 0.2 | New | - | RC |
| 16390G>A | T | Homo | 2.94 | Known | Benign | RC |
| 16390G>GA | T | Hetero | 0.2 | New | - | RC |
| 16393C>CT | T | Hetero | 0.2 | New | - | RC |
| 16394C>CT | T | Hetero | 0.2 | New | - | RC |
| 16411C>CA | V | Hetero | 0.2 | New | - | RC |
| 16416A>AC | V | Hetero | 0.39 | New | - | RC |
| 16422T>TC | T | Hetero | 0.2 | New | - | RC |
| 16423A>AC | V | Hetero | 0.2 | New | - | RC |
| 16443T>TG | V | Hetero | 0.2 | New | - | RC |
| 16453C>CG | V | Hetero | 0.2 | New | - | RC |
| 16468T>TG | V | Hetero | 0.39 | New | - | RC |
| 16469T>TG | V | Hetero | 0.39 | New | - | RC |
| 16478C>CA | V | Hetero | 0.2 | New | - | RC |
| 16488C>T | T | Homo | 0.2 | Known | - | RC |
| 16490G>GT | V | Hetero | 0.2 | New | - | RC |
| 16491T>TC | T | Hetero | 0.2 | New | - | RC |
| 16491T>TG | V | Hetero | 0.2 | New | - | RC |
| 16493T>TG | V | Hetero | 0.2 | New | - | RC |
| 16497A>AT | V | Hetero | 0.2 | New | - | RC |
| 16499A>AT | V | Hetero | 0.2 | New | - | 3L |
| 16505T>TC | T | Hetero | 0.2 | New | - | 3L |
| 16514C>CG | V | Hetero | 0.2 | New | - | RC |
| 16519T>C | T | Homo | 6.65 | Known | Benign | RC |
| 16522T>TA | V | Hetero | 0.2 | New | - | RC |
| 16524A>AT | V | Hetero | 0.2 | New | - | RC |
| 16527C>CG | V | Hetero | 0.2 | New | - | RC |
| 16527C>T | T | Homo | 0.78 | Known | Benign | RC |
| 16544T>TG | V | Hetero | 0.2 | New | - | RC |
| 16563C>CG | V | Hetero | 0.2 | New | - | RC |
| 16568T>TA | V | Hetero | 0.2 | New | - | RC |
Note: T: transitions; V: Transversions; Homo: Homoplasmic; Hetero: Heteroplasmic; RC: Control region; CSB1-2-3: Conserved sequences block 1, 2 and 3; MT: Mitochondrial; HV1-2: Hypervariable sites 1 and 2; OHR: Heavy strand origin of replication; TFX-Y: Encoded transcription factor binding site X-Y.
Table 2: Nature, position, and impact of the D-loop mutations.
Impact of FGB mutations
No mutations in the FGB gene were predicted to be pathogenic or affect splice sites. However, cancer-specific prediction tools demonstrated that the c.1244+75T>A mutation is a cancer driver (Table 3).
| Generic tools | Cancer-specific tools | |||||
|---|---|---|---|---|---|---|
| Mutation | CADD | FATHMM-XF | MutationTaster | PhD-SNPg | CScape | CScape-Somatic |
| Benign | Oncogenic/Benign | |||||
| c.1244+75T>A | 0.2 | 0.029* | 0/100 | 0.014 | 0.577 | 0.567 |
| c.1244+27A>T | 0.206 | 0.142 | 0/100 | 0.049 | 0.618 | 0.311 |
| c.1244+206G>A | 0.378 | 0.039 | 0/100 | 0.004 | 0.582 | 0.363 |
| c.1244+258A>G | 1.91 | 0.025* | 0/100 | 0.008 | 0.233 | 0.562 |
Note: * With high confidence.
Table 3: Effect of FGB mutations.
Association of FGB and D-loop mutations
We found that a significant correlation between the mutations in the FGB and D-loop genes with a positive Fisher's exact test (P=0.0005) and a nonzero Cramer's V association coefficient (V=0.77).
This study aimed to establish a non-coding mutational profile for patients with breast cancer in Senegal using intron 7 of the nuclear gene FGB and the mitochondrial gene D-loop. Contrary to a previous report who showed no genetic variability in the FGB gene [17], we detected a polymorphism, which suggests its involvement in breast cancer development. The difference in results may be attributed to the previous study using aligned sequences in their analyses, which can lead to a loss of heterozygosity. In contrast, the benign character of the mutations corresponded perfectly to the typical characteristics of fibrinogen, most of which have minor modifications and polymorphisms that are neutral and do not affect its structure or function [18].
In the present study, all novel mutations found were tolerated; with the exception of the c.1244+75T>A mutation, which was predicted to be oncogenic by our cancer-specific tools. This mutation, which is the most frequent mutation, is a transversion and can change the structure of nuclear DNA. In breast cancers, T→A transversions correspond to mutational signatures 5 and 8, with a stronger presence in signature 8 [19]. The signature 5 is suspected to be associated to a late diagnostic corresponding to the epidemiological data in Senegal and West Africa [8,20]. As to the Signature 8, it has been associated with a homologous recombination deficit; however, its impact seems to only be effective in the late stages of mammary carcinogenesis. This suggests that the c.1244+75T>A mutation, and consequently the FGB gene, may play a role in the development and/or progression of breast cancer. Thus, further research is needed to investigate the effect of the T→A transversion in more detail and to determine glycoprotein action.
For the D-loop, the variants A263G, A73G, T16519C, T152C, T195C, and C150T were the most representative and the frequency of their recurrence indicates their involvement in the development or progression of breast cancer. Doupa et al. [21] observed the same mutations in Senegalese women with benign tumors and demonstrated that these mutations prevented the development of breast fibroids. In our study, prediction of the benign variants may confirm these findings. Conversely, Kuo, et al. [22], reported that D-loop mutations were associated with progesterone receptor (PR) negativity, which is an indicator of poor prognosis in breast cancer. Similarly, in Chinese and Taiwanese populations, A73G, T16519C, T195C, and C150T mutations were associated with an increased risk of developing chronic kidney disease [23], systemic lupus erythematosus [24], and lung squamous cell carcinoma [25]. The difference in these results suggests a singular action of the D-loop depending on the pathology [26] and according to Bai, et al. [23], it also reflects the particularity of the mitochondrial genetic inheritance of each population.
All new mutations characterized in this study were heteroplasmic. Heteroplasmy is associated with aging and degenerative diseases, such as Alzheimer's disease and Parkinson’s disease [27]. It is estimated to have a 1.94-fold higher pathogenic potential than homoplasmy and affects the control region of DNA to a greater extent [28]. Given that the mutations found in this study were also located in this area and are involved in different pathologies, not to mention that they could not be tested, we can assume their involvement in breast tumorigenesis.
The high degree of association found between FGB and D-loop mutations confirmed the link between nuclear and mitochondrial DNA. Indeed, in a study of 13 types of cancers involving somatic mutations in the nuclear and mitochondrial genomes, it was reported that nuclear gene expression in cancer-related pathways (tumor necrosis factor-α signaling, oxidative phosphorylation) was upregulated in tumor cells with truncating mutations in mtDNA [26]. Thus, we hypothesize that alterations in the D-loop leads to oxidative stress and results in tumor formation, which subsequently evolves into malignancy when coupled with inflammation induced by mutations in the FGB gene, either independently or in combination with reactive oxygen species. This is consistent with the latency of signature 8 mutations in breast carcinogenesis.
In this study, we identified a novel cancer-causing mutation in the FGB gene using sequence analysis. While predictions of splicing were inconclusive and the exact mechanism of action remains unknown, this new mutation may be a potential biomarker for the early diagnosis of breast cancer. In addition, we found large genetic variability in the mitochondrial D-loop, even though its mutations were predicted to be benign. Nevertheless, the strong association between mutations in both genes and the discovery of new heteroplasmic mutations suggests that both genes may be involved in the development and/or progression of breast cancer.
The authors acknowledge the genomics laboratory of the Department of Animal Biology, Faculty of Science and Technology, Cheikh Anta Diop University, Dakar.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Niang R, Mbaye F, Sembeme M (2023) Exploring the Role of Non-Coding Sequence Mutations in Breast Cancer. J Can Sci Res. 8:537.
Received: 31-Mar-2023, Manuscript No. JCSR-23-22757; Editor assigned: 03-Apr-2023, Pre QC No. JCSR-23-22757 (PQ); Reviewed: 17-Apr-2023, QC No. JCSR-23-22757; Revised: 24-Apr-2023, Manuscript No. JCSR-23-22757 (R); Published: 01-May-2023 , DOI: 10.35248/2576-1447.23.8.537
Copyright: © 2023 Niang R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.