Journal of Hematology & Thromboembolic Diseases
Open Access
ISSN: 2329-8790
ISSN: 2329-8790
Case Report - (2023)Volume 11, Issue 9
Extramedullary Hematopoiesis (EMH) is a rare but intriguing condition where blood cell production occurs outside the bone marrow. While commonly observed in organs like the liver and spleen, EMH can manifest unexpectedly, presenting unique diagnostic and therapeutic challenges. This case report details an exceptional instance of EMH occurring in the posterior mediastinum, a highly unusual location. The anatomical location of the mediastinal mass is notable, given its rarity within the context of EMH. While EMH has been reported in various extramedullary sites, the mediastinum remains an exceptionally infrequent location. This region's proximity to vital structures, including the heart and major blood vessels, accentuates the clinical significance and necessitates further research on potential compression and management strategies. The successful surgical intervention and swift postoperative recovery underscore the significance of a multidisciplinary approach in hematology. This case challenges established paradigms and emphasizes the importance of considering unconventional presentations of hematological conditions. Continued research and reporting of unique cases such as this contributes to advancing our understanding of hematology and enhancing patient care.
Extramedullary hematopoiesis; Posterior mediastinum; Hematological disorders; Diagnostic challenges; Surgical intervention.
Extramedullary Hematopoiesis (EMH) is a fascinating and relatively rare condition within the realm of hematology, characterized by the production of blood cells outside of the bone marrow. While the liver and spleen are the most common sites for EMH, this condition can manifest in unexpected locations throughout the body, offering unique challenges for diagnosis and treatment [1]. In this case, we present an unusual instance of EMH occurring within the posterior mediastinum. Mediastinal masses are typically associated with various conditions, including neurogenic tumors and lymphomas, making it imperative to accurately identify the nature of the mass. In this particular case, the discovery of a posterior mediastinal mass during a physical examination prompted further investigation. To distinguish between neurogenic and mediastinal masses, Video-Assisted Thoracoscopic Surgery (VATS) was performed, providing a minimally invasive means of exploring the mass and obtaining tissue samples for pathological analysis.
The postoperative pathological results yielded a surprising and intriguing finding: The mass was consistent with extramedullary hematopoiesis. This discovery is remarkable because EMH cases that do not coincide with chronic anemia are exceptionally rare, and the clinical features of such occurrences have scarcely been reported in the medical literature. Understanding the clinical implications of this unique case is crucial. Extramedullary hematopoiesis is typically seen as a compensatory mechanism in response to bone marrow disorders or chronic anemia, where the body attempts to produce more blood cells outside the marrow to maintain blood cell counts [2]. However, cases like the one described here challenge our conventional understanding of EMH. It raises important questions about the triggers and mechanisms that lead to EMH in the absence of chronic anemia, and whether it might represent a broader spectrum of hematological responses to various stimuli.
Additionally, the anatomical location of the mediastinal mass in this case is noteworthy. While EMH has been reported in numerous extramedullary sites, including the liver, spleen, and even the central nervous system, occurrences in the mediastinum are exceptionally rare. The mediastinum is a vital area housing essential structures such as the heart, major blood vessels, and the trachea, making the presence of an EMH mass in this region even more intriguing. The potential implications for compression of nearby structures and the clinical management of such cases are topics that warrant further investigation [3]. In the case of extramedullary hematopoiesis in the posterior mediastinum, as described here, serves as a reminder of the complexity and diversity of hematological disorders. It underscores the importance of considering rare and unconventional manifestations of conditions like EMH, especially when they deviate from the typical clinical presentation. Further research and case studies are needed to better understand the underlying mechanisms and clinical implications of such exceptional occurrences, ultimately advancing our knowledge of hematology and improving patient care.
The case of the 66 year old male with a posterior mediastinal mass highlights the importance of thorough clinical evaluation, advanced diagnostic techniques, and precise surgical interventions in the field of hematology. The patient's history of a posterior mediastinal mass occupying the space for two years, detected during a physical examination, raised concerns about potential underlying conditions. Upon admission, comprehensive laboratory tests were conducted, shedding light on the patient's hematological profile [4]. The results indicated a white blood cell count of 8.24 × 10^9/L, hemoglobin level of 117 g/L, a red blood cell count of 5.92 × 10^12/L, hematocrit at 38.10%, mean erythrocyte volume of 64.40 fL, mean hemoglobin content of 19.80 pg, and mean hemoglobin concentration of 307.00 g/L. Notably, these values were largely within normal limits, suggesting that the patient did not exhibit signs of chronic anemia, which is a common trigger for Extramedullary Hematopoiesis (EMH).
The next crucial step in the diagnostic process involved radiological imaging. Contrast-enhanced Computed Tomography (CT) examination of the chest revealed a lateral mass measuring 28 mm × 32 mm on the right side of the 10th thoracic vertebra. This mass exhibited a density of 60 Hounsfield Units (HU), and although it was considered benign, the possibility of it being a neurogenic tumor was entertained. The radiological findings served as a valuable guide for surgical planning and decision-making (Figure 1).
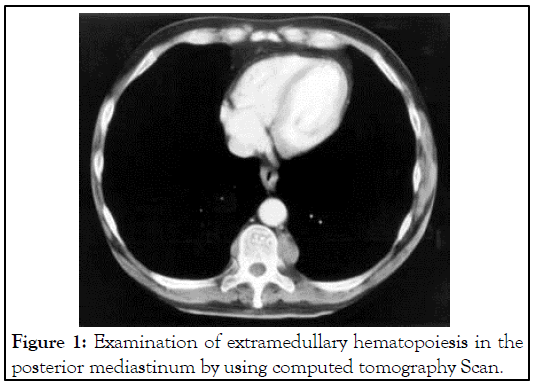
Figure 1: Examination of extramedullary hematopoiesis in the posterior mediastinum by using computed tomography Scan.
To further investigate the patient's condition and ensure an accurate diagnosis, color Doppler ultrasound was performed. Importantly, the ultrasound did not reveal splenomegaly, which can be associated with EMH in certain cases. This finding added another layer of complexity to the diagnostic puzzle, as the absence of splenomegaly suggested that the source of EMH might not be immediately apparent.
The decision was made to proceed with a single port thoracoscopic resection of the posterior mediastinum mass under general anesthesia. The surgical approach involved an incision in the right midaxillary line at the fifth intercostal space. During the operation, the characteristics of the mass were noted: It was situated on the right side of the spine, had a dark red appearance, exhibited a long elliptical shape, possessed a complete capsule, and was supported by a rich blood supply from the base.
Immunohistochemical analysis of the tissue samples provided valuable insights into the nature of the mass. The results indicated positive staining for CD117 (scattered positive), CD235a (positive), CD34 (vascular positive), CD61 (scattered positive), CD68 (tissue cells positive), E-cadherin (a small amount positive), KI-67 (70 percent positive), Lysozyme (partially positive), and Myeloperoxidase (MPO) partially positive. These findings collectively led to the final pathological diagnosis of posterior mediastinum extramedullary hematopoiesis.
The successful surgical intervention and the postoperative course of the patient were noteworthy. The chest drainage tube was removed on postoperative day 3, indicating uncomplicated recovery. The patient was discharged on day 4 after surgery, marking a swift and favorable outcome.
This case underscores the importance of a multidisciplinary approach in hematology, where clinical evaluation, laboratory investigations, and advanced imaging techniques are combined to arrive at a precise diagnosis. The rarity of extramedullary hematopoiesis without chronic anemia adds an intriguing dimension to our understanding of hematological disorders. Furthermore, the choice of a minimally invasive surgical approach in this case highlights the significance of precise and innovative surgical techniques in the management of such conditions.
Continued research and clinical reporting of unique cases like this one contribute to the expanding knowledge base in hematology and enhance our ability to diagnose and manage complex hematological conditions effectively [5]. As the field of hematology advances, it is likely that we will uncover more cases that challenge conventional thinking and broaden our understanding of the diverse manifestations of blood-related disorders.
Extramedullary hematopoiesis is a phenomenon where blood cell production occurs outside the bone marrow. It is considered a compensatory mechanism in response to the inability of the hematopoietic organs, primarily the bone marrow, to adequately produce the required number of red blood cells to meet the body's demand. Pathological EMH is often associated with chronic blood disorders, including anemia and myelodysplastic syndrome. While EMH is more commonly observed in organs like the liver, spleen, and lymph nodes, occurrences in the posterior mediastinum are exceedingly rare [6]. The first documented case of posterior mediastinal EMH dates back to 1912 when Guizetti made this discovery during an autopsy. The rarity of this condition and the potential for misdiagnosis underscore the importance of a thorough understanding of the patient's medical history and clinical presentation. In some cases, it is advised not to surgically remove extramedullary hematopoietic tissue unless there is significant organ compression or spinal canal invasion, or when patients experience symptoms such as dyspnea due to spontaneous bleeding.
However, diagnosing mediastinal EMH can be challenging, especially when it is not associated with an underlying hematopoietic disease [7]. The paravertebral region is a common site for extramedullary hematopoietic tissue, accounting for approximately 15% of paravertebral tumors. When it manifests in this region, it typically presents as a thoracic paravertebral mass. These masses often do not cause obvious symptoms, though in some cases, they can lead to issues like difficulty breathing, pleural effusion, or hemothorax. Medical imaging, particularly chest CT scans, plays a vital role in diagnosing mediastinal EMH. On imaging, thoracic paravertebral EMH masses usually appear as soft tissue masses with areas of fat attenuation and without calcification. When these specific imaging features are identified, especially in the context of a predisposed medical condition such as myelodysplastic disease or severe anemia, extramedullary hematopoiesis becomes a strong consideration. Magnetic Resonance Imaging (MRI) is also a valuable diagnostic tool, as it can reveal soft tissue shadows and help differentiate EMH from other conditions like lipoma [8].
Due to the rarity of mediastinal EMH, there are no established evidence-based guidelines for its management. However, existing studies suggest that treatment is typically reserved for cases where patients exhibit symptoms. Management options may include blood transfusion to address anemia, radiotherapy to shrink the EMH masses, the use of hydroxyurea to inhibit blood cell production in extramedullary sites, or, in selected cases, surgical resection.
In conclusion, mediastinal EMH represents a unique and rare condition within the broader field of hematological disorders. Its diagnosis and management require a combination of clinical judgment, medical imaging, and consideration of the patient's overall health and symptomatology. Continued research and reporting of cases like this one contribute to a better understanding of this rare phenomenon and can help inform future guidelines for its diagnosis and treatment.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Falda A, Verma K, Tran D, Bryan BA, Mitchell DC (2023) Extramedullary Hematopoiesis in the Posterior Mediastinum-A Rare Case Report. J Hematol Thrombo Dis. 11:565.
Received: 01-Sep-2023, Manuscript No. JHTD-23-26823; Editor assigned: 04-Sep-2023, Pre QC No. JHTD-23-26823 (PQ); Reviewed: 18-Sep-2023, QC No. JHTD-23-26823; Revised: 25-Sep-2023, Manuscript No. JHTD-23-26823 (R); Published: 02-Oct-2023 , DOI: 10.35248/2329-8790.23.11.561
Copyright: © 2023 Falda A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.