Journal of Pharmacological Reports
Open Access
+44-77-2385-9429
+44-77-2385-9429
Case Report - (2023)Volume 7, Issue 1
In recent years, with the continuous maturation of gastrointestinal endoscopy technology, endoscopic treatment has become the method of choice for foreign body removal. In this paper, we share a rare case of a 63-year-old patient with schizophrenia who ingested a large amount of foreign body of approximately 1 kg. Its rarity is strongly related to the patient's psychiatric disease and presents some challenges to the endoscopic procedure. When the number of foreign bodies is huge, how to remove them accurately and quickly is a critical problem to be solved. This case illustrates different endoscopic techniques that can be used to remove different foreign bodies with different sizes and textures, aiming to provide some practical advice for endoscopists on how to proceed.
Endoscopy; Foreign body; Schizophrenia
In clinical practice, foreign bodies in the esophagus and stomach are common, and the majority are caused by accidental swallowing during feeding [1]. It is extremely rare for a patient to actively swallow such a large number of foreign bodies. With the continuous development of gastrointestinal endoscopy technology, endoscopic treatment has become the method of choice for foreign body removal [2]. We present the case of a schizophrenic patient who ingested a large number of foreign bodies, which were successfully retrieved endoscopically from the gastric cavity.
A 63-year-old female patient was admitted to the emergency department due to dysphagia after ingesting several foreign bodies. The blood routine examination showed leukocytes 8. 22 × 10^9/L, neutrophils - 89. 4%, CRP 3. 86 mg/L, hemoglobin 100 g/L, D-D dimer 6. 28 mg/L. As shown in Figure 1, abdominal CT revealed a markedly distended gastric cavity with gas and debris.
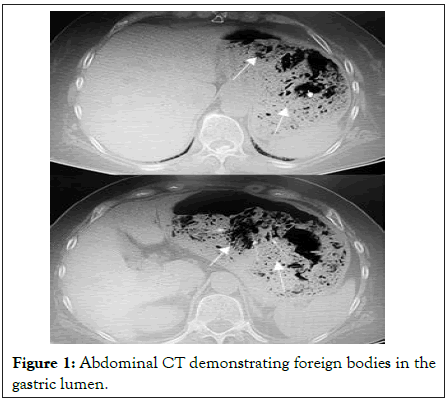
Figure 1: Abdominal CT demonstrating foreign bodies in the gastric lumen.
During the preoperative evaluation, we considered that the patient had a history of schizophrenia for 46 years and was likely to be unable to fully cooperate with ordinary surgery, so endoscopic foreign body removal was performed under intubation anesthesia. There was a large amount of foreign material and food residue in the gastric cavity. The foreign material was mainly various polyethylene plastic overwrapped boxes, details of which are shown in Figure 2.

Figure 2: Endoscopic view of several foreign bodies in the gastric cavity and its removal using forceps and caps.
In this case, how to accurately and quickly remove these soft and hard foreign bodies of different sizes, was the difficulty of treatment and the innovation of this operation. During the operation, we first used foreign body forceps to detect the texture of the foreign body. If it was soft, we placed the forceps in the middle of the foreign body and picked it up. When the volume of the plastic product was large, it was first dragged to a relatively flat place in the stomach cavity, folded repeatedly, and then clamped up. If the foreign body was hard, picked up the foreign body from the head end and slowly pulled it out. This method can ensure that the pliers are not easy to slip out from the surface of the foreign body.
In Figure 3, we can see a portion of the foreign body embedded in the mucosa, causing local edema and ulceration. In this case, to avoid further scratching of the stomach wall, we used a transparent cap.
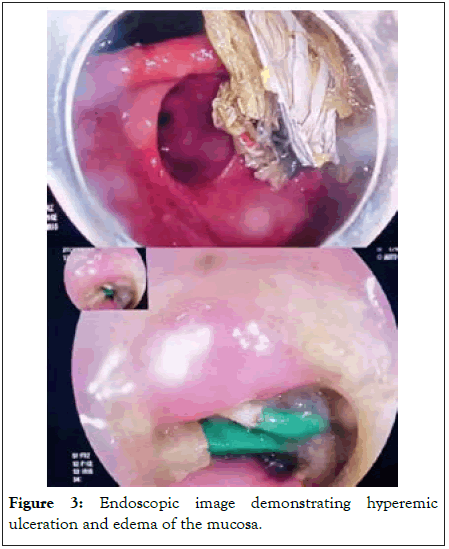
Figure 3: Endoscopic image demonstrating hyperemic ulceration and edema of the mucosa.
We managed to bring the blunt end of the foreign body close to the inner lens end, placed one end of the foreign body inside the transparent cap, grasped the foreign body with a foreign body clamp, and then tried to keep the longitudinal axis of the foreign body and the wall of the tube parallel to the retraction. For a foreign body embedded in the mucosa, it could be removed by slowly incorporating a transparent cap placed at the front end of the endoscope, while for a foreign body embedded in the mucosa at both ends, we chose to loosen the shallow embedded end first, then pull out the other end and adjust the direction of the foreign body so that the head end would be incorporated into the transparent cap for removal. When the mucosal injury was obvious, ice saline norepinephrine solution was sprayed locally and the wound was clamped with a titanium clip to stop the bleeding. In addition, when the foreign body was fragmented or massed, we used a lithotripsy mesh basket to snare the foreign body. After repeated use of foreign body forceps, clear caps, and lithotripsy baskets, the procedure lasted 2 hours and approximately 1 kg of foreign body was removed, as shown in Figure 4.
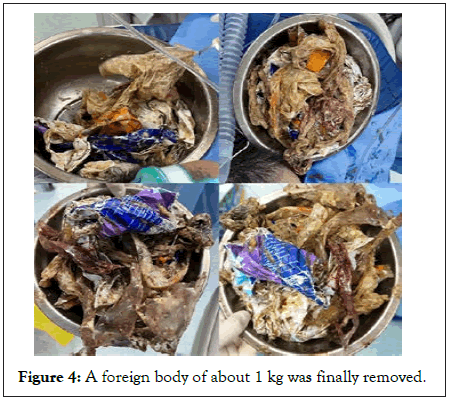
Figure 4: A foreign body of about 1 kg was finally removed.
The entire endoscopic treatment procedure was shown in the Figure 5. Postoperatively the patient was started on broadspectrum antibiotics to prevent infection and was discharged asymptomatic the day after the surgery.
Figure 5: Endoscopic video of foreign body removal.
There are few reported cases of patients who actively swallow large amount of foreign bodies due to mental illness. Studies have shown that 18% of adult patients who actively ingest foreign bodies have primary neurological disorders, including schizophrenia, Parkinson's disease, mental retardation, or cerebral palsy [3]. In the field of mental health medicine, such active swallowing of foreign objects is usually defined as xenophagia. It refers to a very complex syndrome of multiple disorders caused by metabolic disorders, taste abnormalities and psychiatric disorders in patients without an objective cultural context. There have been many studies describing the removal of ingested coins, batteries, magnets and other foreign bodies from the upper aerodigestive tract [4]. Recently, endoscopy has become the preferred approach to remove foreign bodies in the upper tract, since it is more economical, effective, quick, less painful, and less traumatic and with fewer complications, comparing to surgical procedures [5]. The European Society for Gastrointestinal Endoscopy has published guidelines on the removal of foreign bodies [6], which detail the indications and contraindications for endoscopic treatment of foreign bodies, and specifically state that general anesthesia or tracheal intubation with forceps for foreign bodies is recommended for the mentally disturbed and uncooperative operator. The patient in this case was operated under tracheal intubation and general anesthesia according to the guidelines. The guidelines describe the management of different types of foreign bodies in the upper gastrointestinal tract and suggest that the size, sharpness, and shape of the ingested foreign body are some of the characteristics that medical personnel should consider when dealing with this condition. Guidelines recommend the use of instruments such as clear caps, condoms and cuffs in the management of sharp foreign bodies. During the procedure in this patient, we used clear caps and lithotomy mesh baskets to maximize the protection of the patient's gastric mucosa and reduce the incidence of perforation and infection [7]. During the future clinical practice, we will try to use more protective devices to better complete the procedure.
In general, the main complications caused by swallowing foreign bodies include gastrointestinal obstruction, bleeding, and perforation, depending on the nature, shape, retention time, and physician's level of practice. Previous studies have shown that when the size of foreign body exceeds 5 cm or has a sharp shape, it tends to greatly increase the incidence of GI (gastrointestinal) obstruction and perforation in patients [8]. That makes higher demands on the technical level of the endoscopist. Surgical treatment is often required for foreign bodies in the gastrointestinal tract that cannot be treated endoscopically, especially when the foreign body is large, irregular in shape or spiky, and when endoscopic removal is difficult. However, before open surgery, we should attempt laparoscopic surgery to remove the ingested foreign body. Minimally invasive laparoscopic surgery due to its advantages should be preferred over open surgery in clinical selection [9].
In summary, to our knowledge, this is a very rare case of huge amount of foreign bodies removed through endoscopy. To overcome technical difficulties, we recommend that endoscopists evaluate the different textures of each foreign body, in order to place the forceps and choose in which direction the foreign body is best removed to prevent complications.
This article has not simultaneously been submitted to any other journal for review and/or publication.
Wen Bao collected and collated the information on the case and drafted the manuscript; Jie Lu critically revised important elements of the manuscript. All authors reviewed and approved the final version of the manuscript.
We wish to thank the patient and her family for their assent and participation in the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval to report this case was obtained from the Institutional Ethics Committee of the Tenth People’s Hospital of Tongji University, Shanghai, China (SHSY-IEC-4. 1/20-40/01).
Written informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
[Google Scholar] [PubMed]
Citation: Lu J, Bao W (2023) Extremely Rare Large Intragastric Foreign Body?A Case Report. J Pharma Reports. 07: 170
Received: 02-Feb-2023, Manuscript No. JPR-23-21685; Editor assigned: 06-Feb-2023, Pre QC No. JPR-23-21685 (PQ); Reviewed: 21-Feb-2023, QC No. JPR-23-21685; Revised: 28-Feb-2023, Manuscript No. JPR-23-21685 (R); Published: 06-Mar-2023 , DOI: 10.35248/jpr.23.7.170
Copyright: © 2023 Lu J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.