Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 3
Infection with Coronavirus Disease-19 (COVID-19) can manifest with multi-system sequelae, including thrombosis and other coagulopathies. The effects of COVID-19 on specific coagulation factors are not well known. In this case, proconvertin (Factor VII) deficiency was observed in a 14-year-old pediatric patient with active COVID-19 infection, along with mild thrombocytopenia, active mucosal bleeding, prolonged Prothrombin Time (PT) and likely vitamin K deficiency. Despite worsening thrombocytopenia, the patient's mucosal bleeding subsided with eventual normalization of his coagulation measures following vitamin K supplementation. We postulate that due to widespread inflammation from active COVID-19 infection, our patient developed vitamin K deficiency resulting in acquired Factor VII deficiency. The mechanism of systemic inflammation causing vitamin K deficiency in the setting of COVID-19 infection should be explored in future studies. Furthermore, Factor VII deficiency should be considered in the setting of COVID-19 infection, especially when patients present with excessive bleeding, prolonged PT and normal Activated Partial Thromboplastin Time (APTT).
Prothrombin time; Congenital factor VII; Tissue factor; Thrombocytopenia; Activated partial thromboplastin time
Infection with COVID-19 can manifest with multi-system sequelae, including thrombosis and other coagulopathies. However, the effects of COVID-19 on specific coagulation factors are not well known. In this case, Factor VII deficiency was observed in a 14-year-old male pediatric patient who presented to the emergency department with active COVID-19 infection, along with mild thrombocytopenia, active mucosal bleeding, prolonged Prothrombin Time (PT) and likely vitamin K deficiency. Despite worsening thrombocytopenia, the patient’s mucosal bleeding subsided with eventual normalization of his coagulation measures following vitamin K supplementation. We postulate that due to widespread inflammation from active COVID-19 infection, our patient developed vitamin K deficiency resulting in acquired Factor VII deficiency. This case illustrates a new concept for physicians in that Factor VII deficiency should be considered in the setting of COVID-19 infection, especially when patients present with excessive bleeding. The mechanism of systemic inflammation causing vitamin K deficiency in the setting of COVID-19 infection should be explored in future studies.
A 14-year-old male with no known medical history presented to the emergency department with a six-day history of fever, nausea, bilateral frontal headache and non-bloody diarrhea, which progressed to left lower quadrant abdominal pain. The patient also reported intermittent epistaxis, two episodes of hematemesis and one episode of frank bleeding from his left ear. Additionally, he experienced symptoms of cough, congestion and significantly decreased oral intake. The patient had tested positive for COVID-19 six days prior to the emergency department visit. His maximum recorded temperature at home was 103.9°F. There were no reported allergies and the patient was not taking any medications before presenting to the hospital. He consumed regular table food. There was no family history of bleeding disorders. On initial assessment, his vital signs included temperature of 100.3°F, heart rate of 109 beats per minute, respiratory rate of 18 breaths per minute, blood pressure of 121/59 mmHg and Oxygen Saturation (SpO2) of 100% on room air. Physical examination demonstrated a tired-appearing patient with dried blood in his left ear canal and mild to moderate tenderness to the left lower quadrant of the abdomen.
The remainder of his examination, including his neurologic examination, was unremarkable. Initial laboratory testing revealed a leukocyte count of 5000 per cubic millimetre (cmm), with neutrophils 85%, lymphocytes 10.6% and a low platelet count at 100k per cmm. His C-Reactive Protein (CRP) was elevated to 3.6 mg/dl, with a normal Erythrocyte Sedimentation Rate (ESR) of 15 mm/hr. The patient was noted to have elevated PT and International Normalized Ratio (INR) at 19.5 secs and 1.72 respectively and elevated D-dimer of 1849 ng/ml. Remainder of the labs were normal, including an APTT that was normal for the lab in which it was performed. His Chest X-ray was unremarkable. A Computerized Tomography (CT) scan showed findings consistent with acute left-sided maxillary sinusitis. The patient received an IV fluid bolus in the emergency department and was admitted for dehydration, coagulopathy, thrombocytopenia and active mucosal bleeding. The patient received oral vitamin K supplementation for 3 days, although exact dosing could not be confirmed. It was noted that his intermittent epistaxis had stopped after initial doses of vitamin K. Augmentin was given for possible left-sided maxillary sinusitis. Repeat labs obtained the following day demonstrated worsening thrombocytopenia to 81k per cmm. A blood smear demonstrated normochromic, normocytic red cells, lymphopenia and thrombocytopenia with normal platelet morphology. The patient’s PT corrected to within 0.5 seconds of normal on mixing study. He had a Factor VII level of 44% with reassuring Von Willebrand Factor Assays (VWF). Following the two-day admission, he was discharged with instructions to complete his vitamin K supplementation and augmentin therapy at home. Repeat lab work obtained 1 month following discharge showed normalization of Factor VII to 84%, PT to 14.3 seconds and platelets to 180k per cmm. As we seen in (Figure 1).
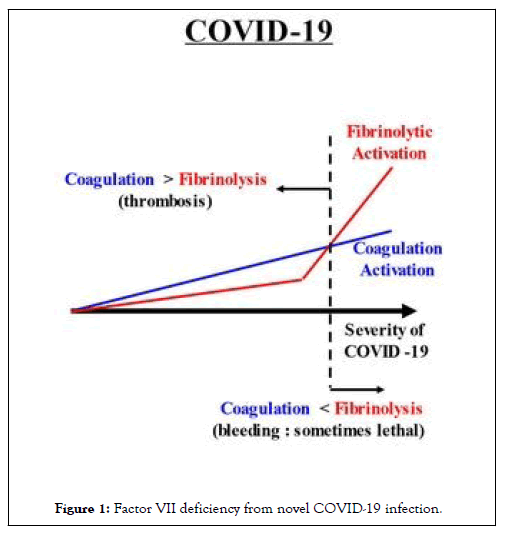
Figure 1: Factor VII deficiency from novel COVID-19 infection.
Prolonged PT, thrombocytopenia and mucosal bleeding in the setting of novel COVID-19 infection has been documented previously; however, the etiologies are yet to be fully elucidated [1]. Interestingly, our extensive literature search revealed no documented cases of Factor VII deficiency in the setting of novel COVID-19 infection. Factor VII is a vitamin K-dependent, non-enzymatic cofactor synthesized via the liver and plays an important role in the blood coagulation system. Tissue Factor (TF) is typically released from damaged endothelium, subsequently binding to Factor VII and resulting in the production of thrombin and fibrin which are essential for hemostasis [2,3]. Diminished Factor VII may result in mucosal bleeding, epistaxis and gastrointestinal bleeding as was seen in our patient. Congenital Factor VII deficiency is rare (less than one case per 500,000 individuals) and is inherited as an autosomal recessive trait [4]. Given normalization of our patient’s Factor VII following vitamin K administration; a congenital Factor VII deficiency is ruled out.
Our patient had a low Factor VII level of 44% (normal reference range 74-180) in the context of elevated PT and normal APTT, concerning for an acquired Factor VII deficiency contributing to clinical bleeding [5]. Acquired low Factor VII deficiency can be seen in patients with hepatic dysfunction, vitamin K deficiency and in patient taking warfarin. Low levels can also be observed in patients with specific factor VII inhibitors and in association with homocystinuria and aplastic anemia [4]. The most likely etiology for this patient’s low factor VII levels was vitamin K deficiency. Factor VII has the shortest half-life of all procoagulants, estimated to be about 3 to 6 hours [6]. Hence when there is a problem in synthesis, Factor VII is the first to decrease followed by decreases in other vitamin K dependent cofactors. Vitamin K is a fat-soluble vitamin and is needed for carboxylation of Factor VII. Typical causes of vitamin K deficiency include gastro-intestinal malabsorption, poor dietary intake, liver dysfunction or medications. Cases describing vitamin K deficiency secondary to gastrointestinal losses or malabsorption note profuse or profound diarrhea [7,8]. It would be very abnormal for a previously well patient to develop coagulopathy secondary to vitamin K deficiency in the setting of 3 days of mild diarrhea, as in this patient. We speculate that the acquired Factor VII deficiency from low vitamin K as seen with our patient was most likely secondary to widespread inflammation due to novel COVID-19 infection. Multiple studies done in both rat models and humans have time and again elucidated the importance of anti-inflammatory and anti-oxidative properties associated with vitamin K [9-13]. In the setting of ongoing inflammation, vitamin K is known to be depleted [14]. We came across two recent studies that were done in hospitalized COVID-19 positive adults which showed severe vitamin K insufficiency [15,16]. However there has yet to be sufficient research into the effects of COVID-19 infection on inducing vitamin K deficiency, especially in pediatric populations. Unfortunately, it is difficult to measure the direct vitamin K levels in plasma due to their low circulating levels, the non-polar characteristics of vitamin K and their interference with lipids [17]. Vitamin K status is usually assessed by indirect measurement when clinically indicated including prothrombin time or by measurement of under carboxylated proteins. Sample preparations for direct measure of vitamin K analysis remains difficult and requires highly specialized laboratories.
Regarding the patient’s mild thrombocytopenia of 100k per cmm, this was likely a consequence of viral suppression. In the absence of any dermatologic findings, spontaneous bleeding from mucosal surfaces would be rare. Internal bleeding is usually seen with severely low platelet levels below 50k per cmm [18]. The Factor VII deficiency due to vitamin K deficiency in the setting of active COVID-19 infection may have been the most important contributor to the bleeding given that after initiation of oral vitamin K, the patient had cessation of his mucosal bleeding despite a downtrend in his platelet count.
Factor VII deficiency should be considered in the setting of COVID-19 infection when a patient presents with excessive bleeding along with a prolonged PT and a normal APTT. The etiology of Factor VII deficiency is likely acquired due to a systemic consumption of vitamin K through inflammatory processes associated with COVID-19 infection. Further research should be directed towards the understanding of these intriguing and relevant pathologies. We postulate that due to widespread inflammation from active COVID-19 infection, our patient developed vitamin K deficiency resulting in acquired Factor VII deficiency. The mechanism of systemic inflammation causing vitamin K deficiency in the setting of COVID-19 infection should be explored in future studies.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Fincher A, Badding T, Agrawal H, Mignacca RC, Dokania G (2024) Factor VII Deficiency from Novel COVID-19 Infection. Clin Pediatr. 09:267.
Received: 09-Apr-2024, Manuscript No. CPOA-24-30711; Editor assigned: 11-Apr-2024, Pre QC No. CPOA-24-30711 (PQ); Reviewed: 25-Apr-2024, QC No. CPOA-24-30711; Revised: 02-May-2024, Manuscript No. CPOA-24-30711 (R); Published: 09-May-2024 , DOI: 10.35248/2572-0775.24.09.267
Copyright: © 2024 Fincher A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.