Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research Article - (2023)Volume 12, Issue 2
Background: Detection of pulmonary nodules has a significant impact on people's lives and mental health. The 2020 NCCN guidelines recommend follow-up visit treatment for nodules ≤ 8 mm; however, many patients with small nodules choose surgery. We aimed to explore why these patients underwent surgery and the cause of their anxiety.
Methods: We cross-sectionally surveyed patients with small nodules who had undergone surgery at a local grade 3 hospital.
Results: 338 patients who responded, 234 were included in the final analysis. A total of 68.81% of patients reported clinically significant anxiety about pulmonary nodules, as measured by the IES-R. Poor performance in Activities of Daily Living (ADL) (P=0.022, 95% CI: 1.237-15.857) was associated with the highest positivity rate (92.31%). Other factors such as the presence of solid nodules (P=0.015, 95% CI: 1.26-8.335), multifocal disease (P=0.006, 95% CI: 1.317-5.373), and family history of lung cancer (P=0.048, 95% CI: 1.015-21.307) were also associated with distress.
Conclusion: Current ability to perform activities of daily living, presence of solid and multiple nodules, and family history of lung cancer make patients who choose surgery more likely to experience pain.
Pulmonary nodules; Clinically significant anxiety; Surgical choice
Each year, millions of patients are diagnosed with pulmonary nodules, and as the numbers of people screened with Computed Tomography (CT) screening grows, more and more patients will be spotted with nodules [1]. Although Ground Glass Nodules (GGN) is mostly early non-invasive or slightly invasive adenocarcinomas, they place a tremendous burden on patients, particularly in terms of psychological distress [2]. Given the serious impact of pulmonary nodules, clinicians should have a better understanding of the experiences and concerns of patients with pulmonary nodules and be well prepared to discuss these issues [3,4]. According to the 2020 NCCN guidelines, long-term follow-up is recommended for pulmonary nodules ≤ 8 mm, and surgical treatment is not a good recommendation. However, some patients still choose to have surgery.
Anxiety disorders are a cluster of psychiatric disorders that manifest primarily as symptoms of pathological anxiety. The clinical performance and pathogenesis mainly include Generalized Anxiety Disorder (GAD), atopic phobia, panic disorder, and anxiety disorders caused by other illnesses. In recent years, the percentage of patients with somatic diseases accompanied by anxiety disorders has markedly increased. Psychological abnormalities caused by somatic diseases can impair social functioning and require prompt intervention. Currently, pulmonary nodules are now considered to be a somatic anxiety disorder that cannot be ignored [5].
Almost everyone with nodules is at high risk of suffering psychological harm and anxiety about nodule excision surgery. In recognition of the growing attention to patient-centered care, the American Thoracic Society has recently called for more research to explore the implications of nodule monitoring on patients [6]. Patients with small nodules generally choose conservative treatment and persistent follow-ups. Only a limited number of patients chose surgical therapy. Therefore, we designed to explore the factors influencing preoperative anxiety and the reasons why people choose surgery for nodules locally smaller than 8 mm. We sought to describe the psychosocial implications of nodular implications and estimation by surveying patients with small pulmonary nodules at locally treated sites. We hypothesized that patients would experience anxiety due to their condition, nature of the nodules, and other factors when facing surgical treatment. To understand why patients choose surgery.
Study population
We enrolled patients selected from a local area as subjects for the study. Inclusion criteria for participants were: 1) ASA grade ≤ III; 2) being aware and able to properly express properly information; 3) Age 18-90; 4) nodules less than 8 mm; and 5) and were hospitalized for surgery. Exclusion criteria: 1) not giving consent to be part of the study; 2) patients with a confirmed lung cancer diagnosis; and 3) history of psychotropic drugs (including opioids, NSAIDs, sedatives, and antidepressants) and the abuse of alcohol.
Survey instrument
We devised a self-management questionnaire which covered four aspects: (1) patient characteristics, (2) nodule-specific knowledge, (3) patient-clinician communication, and (4) nodule-specific distress. A battery of pilot tests was conducted at a local hospital to determine the content, validity, reliability, relevance, and understandability of the questionnaire. Five patients were randomly selected for an in-depth investigation to ascertain factors that may have affected their choice of surgical treatment and perioperative anxiety. Furthermore, reference was made to the trial conducted by Freiman et al. at Dartmouth-Hitchcock Medical Centre. The final survey tool comprised 28 items including validated scales and new issues [4].
Survey administration
Data were collected from inpatients at a local hospital between February 2023 and March 2023. Professionals collected the data using a questionnaire. The patients were capable of scanning a QR code and interviewing its content (Figure 1).
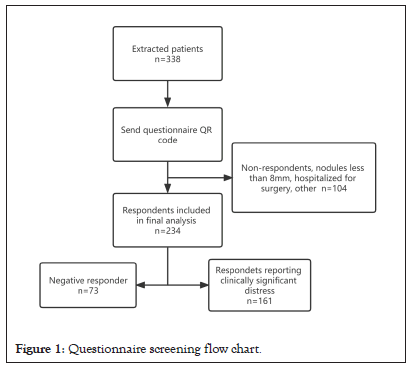
Figure 1: Questionnaire screening flow chart.
Outcome measures
The principal outcome of this pilot was lung nodule-specific distress, as gauged by the Impact Event Scale-Revised (IES-R). The scale consists of two subscales: the avoidance scale (actively staying away from the reminders of the nodule) and intrusion scale (intrusive thoughts). The severity of metastatic trauma can be determined by summing the avoidance scale and the intrusion scales [7,8]. IES-R consists of 16 questions, each with a score of 0 to 4 and an overall score of 0 to 64, with 0 to 8 being subclinical; 9-25 mild; 26-43 moderate; and over 44 severe. Moderate or severe nodular distress was characterized as being statistically significant [4].
On the basis of the patient-centered communication pattern, we assumed that high-quality doctor-patient communication and positive lung nodule test-induced psychological stress would have a significant impact on the choice of surgical treatment for patients with small nodules. Our experience was that many patients overestimate their risk of cancer, and these patients seem to suffer more than those who think they are at a low risk. Therefore, we aimed to understand the reasons why patients choose surgical methods from the perspectives of clinical communication and nodular monitoring [1].
Statistical analyses
All of the analyses were conducted using the IBM SPSS Statistics 26 software. The chi-squared test was used to estimate the correlation between patient characteristics and nodule-specific distress. All significance tests were two-tailed. The multivariate logistic regression model included variables that are identified as potential confounders (self-care ability, nodule nature, presence of multiple lesions, and family history of lung cancer). Odds Ratios (OR) were calculated and 95% Confidence Intervals (CIs) are reported.
Collected data was from 338 patients and 234 patients with nodules smaller than 8 mm. Their mean age was 59.3 (SD=12.3) years. There was no statistically significant difference between male and female patients, with women accounting for 54.70%. Most patients (68.80%) were non-smokers, and approximately one-third (31.62%) earned enough money to pay for the procedure (Table 1). This reflects the low social economic status of our sample and high levels of financial insecurity.
| Characteristics of patients | Value |
|---|---|
| Mean age ± SD, y | 59 ± 12 |
| Gender | |
| Male | 45.30% |
| Female | 54.70% |
| Highest level of education | |
| Primary and below | 57.26% |
| junior high school | 23.08% |
| High school/technical secondary school | 9.83% |
| Junior college/Bachelor | 9.83% |
| Enough money on your own salary to cover expenses | |
| Wasn't Enough | 47.01% |
| Enough | 31.62% |
| Secrecy | 21.37% |
| Fere | |
| Yes | 94.87% |
| No | 5.13% |
| Quantity of children | |
| 0 | 2.14% |
| 1 | 26.92% |
| 2 | 49.15% |
| ≥ 3 | 21.79% |
| ADL | |
| All depend on | 1.71% |
| Some rely on | 14.96% |
| A little rely on | 22.65% |
| Don't need to rely on | 60.68% |
| Current or past smoking history | |
| Smoking, never quit | 16.67% |
| Quit smoking | 14.53% |
| No smoking | 68.80% |
| CT examination demonstrates the nature of pulmonary nodules | |
| Solid nodule | 35.90% |
| Part-solid nodule | 50.00% |
| GGN | 14.10% |
| Pulmonary nodule morphology | |
| Round, quasi-round | 34.19% |
| Having irregular, polygonal or flat, straight edges | 35.04% |
| Be unaware of | 30.77% |
| Number of lesions | |
| Single lesion | 70.51% |
| Multiple lesions | 29.49% |
| Family history of lung | |
| Yes | 10.26% |
| No | 89.74% |
Note: ADL, Activity of Daily Living; SD, standard deviation.
Table 1: Characteristics of survey respondents (n=234).
Distress related to nodules is common. A total of 8.97% of patients had both distress and anxiety of a subclinical kind. The majority of patients reported nodular distress: 22.22% mild and 68.81% clinically significant (52.14% moderate and 16.67% severe). Several factors were significant in both bivariate and multivariate analyses, including difficulty in performing ADL (P=0.022, 95% CI: 1.237-15.857), with the highest positive rate (92.31%). People who lose the capability to take care of themselves in daily life are more vulnerable to have anxiety, and not only need to face the pressure of life but also face the trouble of disease. The presence of solid nodules (P=0.015, 95% CI: 1.26-8.335), multifocal disease (P=0.006, 95% CI: 1.317-5.373), and family history of lung cancer (P=0.048, 95% CI: 1.015-21.307) were also important (Tables 2 and 3). Other characteristics were not appreciably associated with clinically significant distress in bivariate analysis and were not included in the primary analysis.
| Characteristics | Clinically significant distress | Positive rate | P value | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Gender | Female | 41 | 87 | 67.97% | 0.762 |
| Male | 32 | 74 | 69.81% | ||
| Age | <60 | 30 | 83 | 73.45% | 0.138 |
| ≥ 60 | 43 | 78 | 64.46% | ||
| BMI | <24 | 41 | 89 | 68.46% | 0.9 |
| ≥ 24 | 32 | 72 | 69.23% | ||
| Education bakeground | Junior high school and above | 35 | 65 | 65.00% | 0.278 |
| Junior high school the following | 38 | 96 | 71.64% | ||
| ADL | Yes | 70 | 125 | 64.10% | 0.001 |
| No | 3 | 36 | 92.31% | ||
| Nodules nature | GGN | 15 | 18 | 54.55% | 0.003 |
| Part-solid nodule | 43 | 74 | 63.25% | ||
| Solid nodule | 15 | 69 | 82.14% | ||
| Smoking history | No | 52 | 109 | 67.70% | 0.589 |
| Yes | 21 | 52 | 71.23% | ||
| Multiple lesions | No | 58 | 107 | 64.85% | 0.043 |
| Yes | 15 | 54 | 78.26% | ||
| Partner | No | 3 | 9 | 75.00% | 0.634 |
| Yes | 70 | 152 | 68.47% | ||
| Family history of lung cancer | No | 71 | 139 | 66.19% | 0.011 |
| Yes | 2 | 22 | 91.67% | ||
Note: ADL: Activity of Daily Living.
Table 2: Univariate analysis of clinical pain of pulmonary nodules.
| P value | OR | OR 95% CI | ||
|---|---|---|---|---|
| ADL | Yes | 1 | ||
| No | 0.022 | 4.429 | 1.237-15.857 | |
| Family history of lung cancer | No | 1 | ||
| Yes | 0.048 | 4.65 | 1.015-21.307 | |
| Nodules nature | GGN | 1 | ||
| Part-solid nodule | 0.691 | 1.18 | 0.522-2.671 | |
| Solid nodule | 0.015 | 3.241 | 1.26-8.335 | |
| Multiple lesions | No | 1 | ||
| Yes | 0.006 | 2.66 | 1.317-5.373 | |
Note: OR-Odds Ratio; CI-Confidence Interval; ADL- Activity of Daily Living.
Table 3: Factors associated with clinically significant distress in patients with pulmonary nodules.
Moreover, the majority of patients (about 60%-80%) who decided to have the procedure said they clearly remembered their doctors' clinical communication. The remainder said that they did not understand or recall what the doctor said (Table 2). Of the issues related to pulmonary nodules, the perceived risks of cancer (51.78%), surgery (41.72%), and death (53.83%) had a substantial psychological impact on the majority of patients (Figure 2 and Table 4). This shows that the sample population was highly similar in terms of possible cancer and death. Through years of clinical experience the majority of patients equate cancer with death. What they do not know is the very real possibility of immobile tumors (tumors that grow slowly and are unlikely to present problems in their lifetime). Some patients are disturbed by the lung nodules (23.96%) and overall lack of medical knowledge (29.29%) (Figure 3). Therefore we suspect that a significant number of patients do not fully understand what doctors are trying to convey to them, that not all nodules will develop into cancer, that most nodules are benign, and that patients with small nodules support conservative treatment. However, patients' disproportionate fear of death and cancer suggests a lack of effective doctor-patient communication.
| Whether the indicated size of the nodules is mentioned | Whether to mention the results of CT scan | Whether to mention the possibility of cancer | Whether it provides specific information about cancer risk | Whether to mention this diagnostic uncertainty | Whether to mention this reported nodules is common |
|---|---|---|---|---|---|
| 17.46% | 20.12% | 27.81% | 28.70% | 28.70% | 26.63% |
| 78.04% | 75.15% | 65.50% | 63.91% | 6.80% | 68.34% |
| 4.14% | 4.73% | 7.69% | 7.40% | 4.14% | 5.03% |
Table 4: Percentage of patients to choose surgical treatment after the detection of pulmonary nodules.
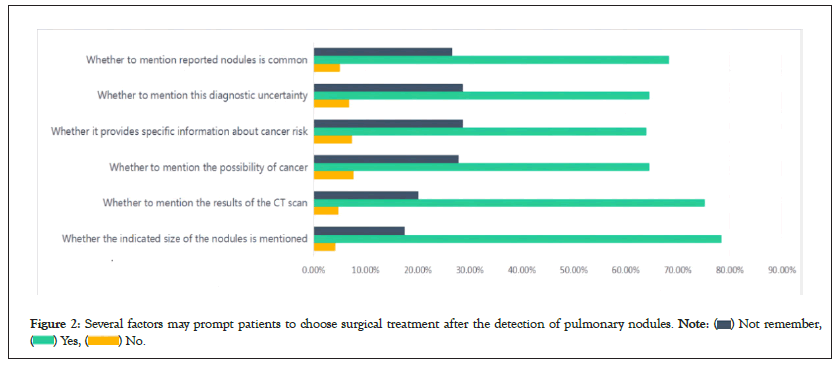
Figure 2: Several factors may prompt patients to choose surgical treatment after the detection of pulmonary nodules. 
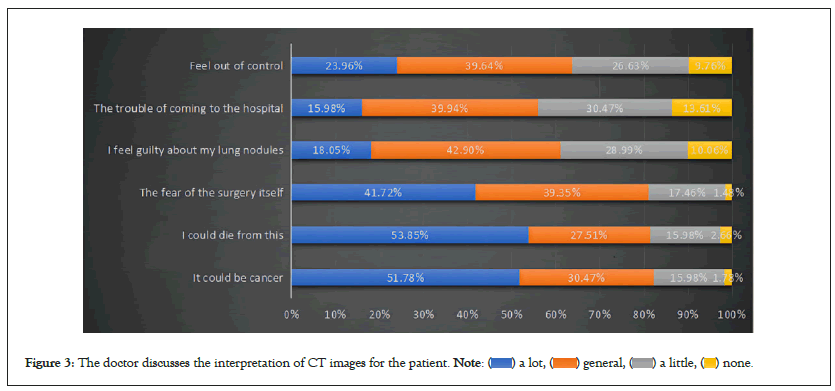
Figure 3: The doctor discusses the interpretation of CT images for the patient. 
To the best of our knowledge, patient evaluation and misinterpretation nodules are commonly seen. Patients' perceptions of cancer risk are more strongly associated with pain than actual disease risk [1]. This underlines the value of improvements clinical communication to rectify patients’ mis-estimations of pulmonary nodules. Validation of these data helps to quantitate the impact of nodule detection on the physical and emotional health of patients [9,10]. However, our findings are different from those of Professor Freiman et al. who showed that patients older than 65 years, current smokers, and those with a high school diploma or less significantly affected anxiety. This study found that poor performance in ADL, the existence of solid and multiple lung nodules, and a strong family history of lung cancer influenced patients' emotions of the patients to varying degrees. In our study, the mean age of the subjects was about 60 years, falling into the older group, which had more primary diseases than the younger age group. Patients who were unable to care of themselves showed greater anxiety following the unexpected discovery of a pulmonary nodule [4,11]. Although most patients knew little about nodules, they understand that the presence of solid and multiple nodules means more likelihood of malignancy. These aspects may cause more psychological pressure to patients in the face of surgery. It is also well known that patients with lung cancers have a family history. Therefore, patients with a family history of lung cancer are more stressed when facing pulmonary nodules, and may have more obvious clinical anxiety when facing surgery. It was surprising that there was no significant association between smoking, non-smoking, and anxiety [12,13].
In our own experience, patients often misjudge the risk of nodules, and although patients know the reasons of their distress, the unpredictable and uncharted nature of their nodules is the chief cause of their anxiety [14]. This indicates the significant gains to be made in helping patients through the nodule surveillance period. A relatively recent study by Slatore et al. demonstrated that this distress can be minimised by high-quality clinical communication. As pointed out in studies of communication about Papanicolaou tests abnormalities, doctors may not bring up cancer since they want to refrain from causing concerns that might not be present, but patients were inclined to fear cancer whether the doctor brought it up or not [15]. For this reason, doctors should discuss cancer risks in a clear manner, unless the patient specifically requests not to be informed. The American College of Chest Physicians suggests a shared decision-making approach for all patients with lung nodules. A clear explanation the process of treatment assists patients to understand and reduce their apprehension [16]. The introduction of nine-year compulsory education in China, so there was no local compulsory education for patients above 50 years of age. Therefore, the majority of patients could make the decision to opt for surgery by consulting their children. Therefore, communication with the younger members of the patients' families often has unexpected results.
As more and more pulmonary nodules are being identified, this emphasises the critical importance of clinical communication. Explaining the risks of pulmonary nodules to patients and enlightening them from a professional perspective is an important component of being a good clinician. These brief communication strategies could help in improving the lives of countless patients with pulmonary nodules each year. The current ability to carry out activities of daily living, the existence of solid and multiple nodules, and a family history of lung cancer make it more likely that patients who opt for surgery will experience pain.
This study did not have a longitudinal dimension and lacked followup data on the dynamics of patients who presented with peak pain at the beginning of nodule discovery. In addition, as the study area was limited to Linhai City, the conclusions may not apply to the general population. Although we selected small nodules, these were also the patients who decided to undergo surgery. This suggests that nodule testing seriously impact on the physical and mental health of patients, and perioperative anxiety is very frequent in this patient group.
This research was approved by the Taizhou Hospital Research Ethics Committee. All experimental procedures were approved by designated agencies and licensing committees. Informed consent was obtained from all subjects and/or their legal guardians. All methods were performed according to relevant guidelines and regulations. The ethics approval number is K20230213.
Hongbin Qiu: Conceptualization, Writing–original draft. Yingqiao Lou: Visualization, Investigation. Congcong Xu: Conceptualization, Methodology, Software. Pasan Witharana: Writing–reviewing and editing. Dong Chen: Software, Validation. Sikai Wu:Writing– review and editing. WuKanghao Zhu: Conceptualization, Software. Jiawei Li: Conceptualization, Methodology. Baofu Chen: Supervision. Jianfei Shen: Project administration.
None
The authors declare that they have no competing interests.
The data used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Qiu H, Lou Y, Xu C, Witharana P, Chen D, Wu S, et al. (2023) Factors Influencing Surgical Choice and Surgical Anxiety in Patients with Pulmonary Nodules Smaller than 8 mm. J Dep Anxiety.12:508.
Received: 22-May-2023, Manuscript No. JDA-23-24314; Editor assigned: 26-May-2023, Pre QC No. JDA-23-24314 (PQ); Reviewed: 09-Jun-2023, QC No. JDA-23-24314; Revised: 16-Jun-2023, Manuscript No. JDA-23-24314 (R); Published: 23-Jun-2023 , DOI: 10.35248/2167-1044.23.12.508
Copyright: © 2023 Hyland P, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.