Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2021)
A multimodal strategy for perioperative analgesia after a complex orthopedic surgical course is essential in preventing protracted hospital stays, minimizing opioid requirements and allowing for early return to baseline mobility. Peripheral nerve blocks are beneficial to elderly patients, not only reducing intraoperative opioid use, but also minimizing postoperative opioid consumption. There is a significant gap in literature reporting on perineural administration of corticosteroids in acute pain management perioperatively in patients with rheumatoid arthritis. We present a case of a combination of single injection fascia layer blockade in an octogenarian woman with severe rheumatoid arthritis, total knee arthroplasty and subsequent multiple revisions, presenting for antibiotic spacer removal, bone graft, and joint arthrodesis. By combining single administration ultrasound guided adductor canal, iPACK (infiltration of the interspace between popliteal artery and the capsule of posterior knee) and obturator nerve blocks, with motor sparing local anesthetic low concentration ropivacaine and a combination of adjuvants, hydrophilic dexamethasone sodium phosphate and lipophilic methylprednisolone acetate, the patient had no additional postsurgical opiate requirements and was able to participate in physical therapy on POD 1. Postoperatively her opioid requirement exhibited an inverted “V” shape progression, slowly increased to the peak on POD 4 (comparable to her preoperative baseline), then continued to drop for the remainder of the admission. On POD 7 she was discharged to a rehabilitation facility with a lower opioid regimen than her previous baseline. In summary, the adoption of chronic pain management modality such as lipophilic glucocorticoid in peripheral nerve block is promising and understudied in the perioperative management of acute on chronic pain patients.
Ophoid; Knee arthrodesis; Chronic pain; Blockade
Perioperative multimodal analgesia strategies are essential for effective pain control, minimizing opioid requirements, reducing hospital length of stay, and early return to baseline mobility and rehabilitation. Peripheral Nerve Blocks (PNB) have been shown to reduce opioid consumption and patients reported pain scores and are widely used in knee procedures. An elderly patient requiring complex knee arthrodesis with an extensive orthopedic surgical history, severe Rheumatoid Arthritis (RA) and high baseline opioid requirement presented a challenging case for the anesthesia and orthopedic teams planning perioperative pain management, Physical Therapy (PT), Occupational Therapy (OT), and disposition. There is a paucity of research on the use of PNB among patients with RA despite the perioperative challenges this systemic autoimmune disorder presents. We present an effective perioperative multimodal analgesic strategy that lasted for one week in an opioid tolerant elderly female via utilizing ultrasound-guided triple fascia plane peripheral nerve blockade using low concentration motor-sparing local anesthetic ropivacaine and perineural adjuvants of different onset time and duration of action, hydrophilic dexamethasone sodium phosphate and lipophilic methylprednisolone acetate. A written informed consent was obtained from the patient for publication of this case report and accompanying images.
80 years-old female from a rehabilitation facility with a past medical history significant for severe RA on chronic prednisone and opioids, coronary artery disease, atrial fibrillation, hypertension, and gastroesophageal reflux disease was admitted for right knee arthrodesis after a complex orthopedic surgical course [1]. She underwent a right Total Knee Arthroplasty (TKA) 10 years ago, which was followed by recent right knee arthroplasty explant, placement of antibiotic spacer, distal femur fracture from a complication from the antibiotic spacer, and now presented for bone grafting and right knee arthrodesis to attempt limb salvage [2]. Upon presentation for surgery, she was mostly wheelchair bound, ambulating with a walker when pain control permitted. At preoperative baseline, her ongoing right knee pain, rated as worst at 5/10 on patient reported Visual Analogue (VAS) pain scale Figure 1, was controlled by a narcotic regimen for years including oxycontin 15 mg BID and oxycodone 5 mg immediate release q4 hours PRN for breakthrough pain, in addition to acetaminophen 650 mg q6 hours as needed Figure 2. The orthopedic team informed her that the first several postoperative days after arthrodesis and the bone graft region are very painful in general and the pain medication will alleviate, but not eliminate the pain.
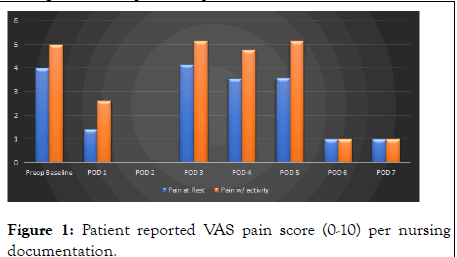
Figure 1: Patient reported VAS pain score (0-10) per nursing documentation.
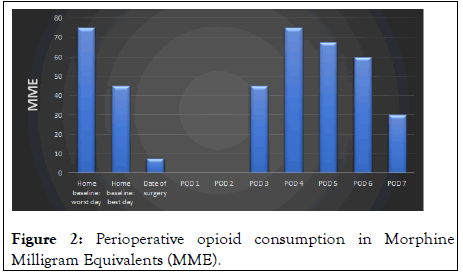
Figure 2: Perioperative opioid consumption in Morphine Milligram Equivalents (MME).
Preoperatively, with a total of 60 mL 0.2% ropivacaine, 10 mg dexamethasone sodium phosphate (DEX) and 80 mg methylprednisolone acetate (Depo-Medrol, MPA), she received a combination of fascia plane blocks, including an adductor canal block (30 mL of the above), an infiltration of the interspace between popliteal artery and the capsule of posterior knee (iPACK) (20 mL) and an obturator nerve block (10 mL). These blocks were placed under ultrasound guidance with direct visualization of the needle and local anesthetic spread at all times and without immediate complications including blood aspirate, pain or resistance with injection, or paresthesia. Intraoperatively, she tolerated the surgery well under general anesthesia with an endotracheal tube, minimal opioid requirements (50 mcg of fentanyl) and received 1 unit of packed red blood cells with estimated blood loss of 1 L with postoperative hemoglobin maintained at 9.7 g/dL without further need for transfusion [3]. Perioperative laboratory data throughout her postoperative hospital stay was monitored with daily complete blood counts and basic metabolic panels Figure 3. Postoperative pain regimen was PO analgesics supplemented with IV opioids for breakthrough pain. Her pain was controlled solely with acetaminophen 650 mg TID with VAS pain scores 0 on the day of surgery, and overnight on day of surgery, her only opioid requirement was one 5 mg oxycodone IR tablet. She did not require further opioids until Postoperative Day (POD 3). She was tolerating PT/OT from POD 1 to POD 3 and described having no right knee pain during all of those therapy sessions. Postoperatively her opioid requirement exhibited an inverted “V” shape progression, slowly increased to the peak on POD 4 which was comparable to her preoperative opioid baseline, then continued to decrease for the remainder of the hospital stay. On POD 6 the day prior to discharge, she reported right knee pain with standing as a 5/10 and at rest 2-3/10 during PT/OT. She stated that her mobility limitations during PT had been due to hip pain, not right knee pain (the arthrodesis device was inserted through the proximal femur). She was discharged to a rehabilitation facility on POD 7 with a newly decreased oxycodone regimen (lower than her preoperative baseline) and reported a 10/10 satisfaction with her surgical knee pain management after this knee arthrodesis. Notably, she did not receive stress dose steroids intraoperatively [4]. She continued her preoperative home prednisone regimen of prednisone 5 mg BID during her postoperative hospital stay and upon discharge. She did not show any signs of complications such as delayed wound healing, surgical wound infection or severe hyperglycemia. On a scale of satisfaction with surgical knee pain management, the patient reported a 10/10 on a numeric scale, rated as “very satisfied”. A written informed consent for publication and HIPAA authorization was obtained from the patient. This work has been reported in line with the PROCESS Criteria [5].
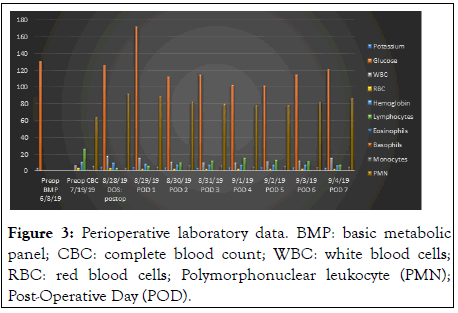
Figure 3: Perioperative laboratory data. BMP: basic metabolic panel; CBC: complete blood count; WBC: white blood cells; RBC: red blood cells; Polymorphonuclear leukocyte (PMN); Post-Operative Day (POD).
PNB are beneficial to elderly patients, not only reducing intraoperative opioid use, but also minimizing postoperative opioid consumption. Local anesthetic is used to block the sensory input that induces central nervous system sensitization in the setting of acute injury or surgical pain, therefore PNB has been implicated as an opportunity to diminish or prevent the development of persistent post-surgical pain. Perineural glucocorticoids as adjuvants to local anesthetics are extensively used to improve the quality and duration of nerve blockade. Although it is unclear whether the primary mechanism of action for perineural glucocorticoids is via systemic absorption or local effect on nerve fibers, multiple mechanisms have been proposed for the analgesic effects of perineural glucocorticoids. These mechanisms include attenuation on the release of inflammatory mediators at the site of nerve injury, such as decreased prostaglandin synthesis, decreased ectopic neuronal firing, and suppression of unmyelinated C-fibers transmission of dull pain. Glucocorticoids such as DEX and MPA are among the most commonly used local anesthetic adjuvants in peripheral and neuraxial nerve blocks respectively, although off label. When used in combination with local anesthetics, hydrophilic DEX can prolong analgesia by a mean period of 6-8 hours with instant onset, as evidenced by a recent systematic review and meta-analysis. Hydrophobic MPA is an extensively used adjuvant in chronic pain therapy that can provide prolongation of nerve blockade for weeks to months but is associated with a delayed onset time up to 24 hours [5-7].
Limitations of this case report include generalizability for two reasons. First, being an elderly RA and chronic pain patient, her post-operative opioid requirements may have been elevated artificially by pain in other locations. For example, per the medical charting, she also complained of abdominal pain throughout her post-operative hospital course, sometimes at higher VAS pains scores than knee pain. Secondly, to achieve a more complete analgesia without additional risk of motor blockage, an obturator nerve block was added to the current standard practice of regional anesthesia technique, i.e., adductor canal back and iPACK block, in the context of multimodal analgesic strategy for knee surgery [8,9] Although ultrasound guided obturator nerve block is known to provide additional analgesia when added to the standard of care adductor canal and iPACK blocks in knee procedures, at this moment it is not commonly performed by practitioners. The combined perineural administration of glucocorticoids of different physical properties and associated differential onset time and duration of action such as DEX and MPA have been shown to effectively prolong the duration of perioperative analgesia [10].
Yet in general there is a significant gap in literature reporting on the roles of lipophilic or particulate glucocorticoids such as MPA in acute pain management. More studies on the use of long-acting glucocorticoids in PNBs for RA patients would be beneficial in both acute and sub-acute pain management after a complex orthopedic procedure. In addition, there are a multitude of knee arthrodesis devices and the one used in this case required insertion through the proximal femur. Therefore, prior knowledge of the operative plan and the specific medical device may warrant the use of nerve blocks around the proximal femur or the hip joint for complete analgesia, highlighting the significance of communication between surgeons and anesthesiologists for effective perioperative management.
Patients with severe RA can have joint destruction, deformity, and pain leading to chronic opioid pain therapy and major joint replacement surgeries, thus presenting significant challenges for perioperative pain management. By combining an obturator nerve block with routine adductor canal block/iPACK, and utilizing a combination of glucocorticoids of different properties, DEX and MPA, as adjuvants, adequate pain control was achieved for this elderly patient with chronic knee pain due to rheumatoid arthritis with history TKA complicated by multiple revisions. The patient was able to tolerate surgery with minimal intraoperative opioid use, and postoperatively she was eager to start PT/OT on POD 1, merely 15 hours after a complex arthrodesis procedure. She maintained lower than preoperative opioid requirement for one week by the time of discharge and was very satisfied with her knee pain management.
Citation: Mejia AB, Wiznia D, Li J (2021) Fascia Plane Blockade with Dexamethasone Sodium Phosphate and Methylprednisolone Acetate for Knee Arthrodesis in an Opioid Tolerant Patient with Rheumatoid Arthritis. Rheumatology (Sunnyvale). 11:296.
Received: 05-Aug-2021 Accepted: 19-Aug-2021 Published: 26-Aug-2021 , DOI: 10.35248/2161-1149.21.s16.004
Copyright: © 2021 Mejia AB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.