Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Research Article - (2021)Volume 10, Issue 5
Objectives: To study the impact of loupe assisted subinguinal varicocelectomy on semen quality, serum testosterone level, and spontaneous pregnancy rate.
Methods: The data were prospectively collected for 102 infertile men with clinical varicoceles. The preoperative values of semen analysis parameters and serum testosterone level were compared with postoperative values at 6 months. Spontaneous pregnancy was assessed at 6 months.
Results: The mean age of patients was 31.56 ± 4.31 years. Primary infertility was reported in 86 patients, while 16 had secondary infertility. Bilateral varicoceles were seen in 79 patients while 23 had unilateral varicoceles. The total sperm concentration (x106/ml) before and after varicocelectomy was 12.82 ± 3.91 and 20.06 ± 2.13 respectively (p<0.0001). The total sperm motility (%) before and after varicocelectomy was 37.67 ± 7.23 and 55.46 ± 4.51 respectively (p<0.0001). The sperm morphology (Kruger/Strict morphology criteria %) before and after varicocelectomy was 3.11 ± 0.80 and 3.70 ± 0.78 respectively (p<0.0001). The serum testosterone level (ng/dl) before and after varicocelectomy was 323.90 ± 67.81 and 396.74 ± 40.88 respectively (p<0.0001). The Spontaneous pregnancy rate in couples with primary and secondary infertility was 18.60% and 31.25% respectively. The difference in their rates was not significant (p=0.251). The overall spontaneous pregnancy rate was 20.5 %.
Conclusion: Loupe-assisted subinguinal varicocelectomy is effective in treating male infertility. It leads to significant improvement in semen quality and serum testosterone level. Despite the absence of definitive studies on the impact of varicocelectomy and fertility outcomes, it is reasonable to consider it as an option in selective varicocele patients with semen abnormalities.
Varicoceles; Pampiniform plexus; Valsalva manoeuvre; Oligoasthenospermia
Varicoceles are abnormally dilated veins of the pampiniform plexus. For a long, it has been linked with male infertility. It is commonly observed in infertile men and has been associated with abnormalities in semen analyses. It is the most commonly seen, correctable cause of male infertility. It has an incidence of 4.4- 22.6% in the general population [1].
Varicoceles cause a duration-dependent decline in semen quality and serum testosterone level. Varicocelectomy prevents further testicular damage, improves semen quality and testosterone production [2,3]. After varicocelectomy, semen quality is expected to improve in 60% to 80% of the men [4-6]. Bilateral varicocelectomy in men who have large unilateral with small contralateral varicoceles and in younger men has a greater beneficial impact on semen quality and testosterone production [7-10].
The impact of varicocelectomy on the pregnancy rate of infertile couples is still not clear. Only a few studies exist, with adequate experimental design to completely assess the role of varicocelectomy in the treatment of male infertility [11,12].
Based on current evidence, it is the practice guideline of both the American Urological Association and the American Society for Reproductive Medicine that correction of varicoceles should be offered to infertile men who have palpable varicoceles and one or more abnormal semen parameters [11]. However, the European Association of Urology (EAU) guidelines on male infertility cautioned, that the impact of varicocele treatment on pregnancy rates in infertile couples is uncertain [12,13]. It also stated that although varicocele treatment in adolescents is effective, there is a significant risk of overtreatment in this group of patients [12].
Many studies have analyzed the impact of varicocelectomy on semen quality in infertile men. A Cochrane review [14] reported the effect of varicocelectomy or embolization in subfertile men. It concluded that there is insufficient evidence to indicate varicocele repair, for improvement of spontaneous pregnancy rate in couples. An Italian study group [15] in their meta-analysis reported a significantly higher pregnancy rate in the treatment group than in controls. Both these studies were criticized due to their limitations. Matthews GJ et al. and Gat Y et al. reported a significant increase in sperm concentration after varicoceles repair in men with non- obstructive azoospermia and severe oligoasthenospermia [16,17]. The spontaneous pregnancy rate in these studies was 31% and 34% respectively.
The data were prospectively collected from 102 patients, who underwent varicocelectomy for infertility in our hospital, from August 2016 to August 2018. Diagnosis of varicoceles was made by clinical examination and Colour Doppler. In patients with clinical varicocele, grading was done using classification proposed by Dubin and Amelar [18]. Diagnosis on doppler study was based on detection of two to three venous channels with at least one >3 mm in diameter and presence of reflux during the Valsalva manoeuvre. Venous dilatation of 2.7 mm diameter or less was graded as subclinical varicoceles (grade I).
Inclusion criteria adopted were age range 20 -40 years, grade II/ III varicoceles, primary infertility, and secondary infertility cases of less than 3 years duration. Patients with subclinical varicoceles were excluded from the study. But those with bilateral varicoceles with grade I varicoceles on one side were included in the study and underwent bilateral varicocelectomy. Patients having endocrine imbalances and obstructive azoospermia were excluded from the study. The spouse of the patient was evaluated by an infertility specialist to rule out possible infertility causes, for the inclusion of couples within this study.
Patients were instructed to observe abstinence for one day before submitting a semen sample. Semen analysis was performed twice at an interval of 7 days and the average of two values was recorded. All semen samples were analyzed using the standardization of WHO (2010 criteria). Semen analysis and serum testosterone level were repeated postoperatively at 6 months for comparative analysis.
All patients were treated by subinguinal varicocelectomy under spinal anesthesia. SurgiTel micro prism (Micro EVK 350) 3.5x magnification loupes were utilized. The spermatic cord was accessed through 3 cm sub-inguinal incision. All veins within the cord except vasal veins were ligated (with 4-0 vicryl) and divided. The testicular artery was identified and preserved using microvascular doppler. All the patients were discharged on the next day of surgery. Patients were advised not to use any form of contraception and abstain from smoking for the duration of the study.
Continuous variables were presented as mean ± SD. Categorical variables were expressed in frequency and percentages. Semen parameters were compared before and after varicocelectomy by performing paired t-test. Categorical variables were compared by performing the chi square test. For small numbers, Fisher’s exact test was applied wherever required. P-value<0.05 was considered statistically significant. Statistical software STATA version 14.0 (StataCorp) 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP) was used for statistical analysis.
The mean age of patients was 31.56 ± 4.31 years. Primary infertility was noted in 86 (84.31%) patients, while 16 (15.69%) patients had secondary infertility. Unilateral varicoceles were found in 23 (22.55%) patients, while 79 (77.45%) patients had bilateral varicoceles. All the patients underwent bilateral varicocelectomy. After varicocelectomy, significant improvement was noted in sperm density, total progressive motility, and morphology. The mean ± SD of sperm density (x 106/ml) before and after varicocelectomy was 12.82 ± 3.91 and 20.06 ± 2.13 respectively (P<0.0001) (Table 1) (Figure 1a). The mean ± SD of total motility (%) before and after varicocelectomy was 37.67 ± 7.23 and 55.46 ± 4.51 respectively (P<0.0001) (Table 1) (Figure 1b). The mean ± SD of sperm morphology as per Kruger/Strict morphology criteria (%) before and after varicocelectomy was 3.11±0.80 and 3.70±0.78 respectively (P<0.0001) (Table 1) (Figure 1c). The improvement in sperm density, motility, and morphology at 6 months post-op was by 56.45%, 47.23%, and 18.97% respectively.
| Before varicocelectomy | 6 Months after varicocelectomy | t-value | p-values | % improvement | |
|---|---|---|---|---|---|
| Sperm density( millions/ml) | 12.82 ± 3.91 | 20.06 ± 2.13 | 23.14 | <0.0001* | 56.45 |
| Total sperm motility (%) | 37.67 ± 7.23 | 55.46 ± 4.51 | 28.5 | <0.0001* | 47.23 |
| Sperm Morphology (%) | 3.11 ± 0.80 | 3.70 ± 0.78 | 14.58 | <0.0001* | 18.97 |
| Serum testosterone level(ng/ml) | 323.90 ± 67.81 | 396.74 ± 40.88 | 16.42 | <0.0001* | 22.49 |
Values are represented as mean ± standard deviation
*P < 0.05- statistically significant
Table 1: Semen parameters and serum testosterone level 6 months after varicocelectomy (Paired t- test).
The mean ± SD of serum testosterone level (ng/dl) before and after varicocelectomy was 323.90 ± 67.81 and 396.74 ± 40.88 respectively (P<0.0001) (Table 1) (Figure 1d). Baseline serum testosterone level was noted to improve by 22.49% at 6 months after varicocelectomy.
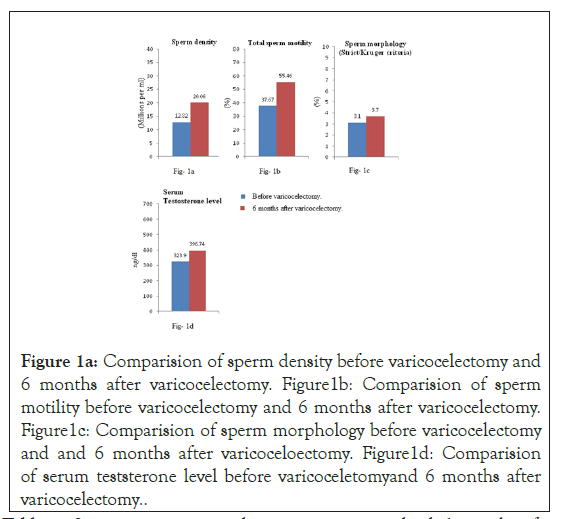
Figure 1a: Comparision of sperm density before varicocelectomy and 6 months after varicocelectomy. Figure1b: Comparision of sperm motility before varicocelectomy and 6 months after varicocelectomy. Figure1c: Comparision of sperm morphology before varicocelectomy and and 6 months after varicoceloectomy. Figure1d: Comparision of serum teststerone level before varicoceletomyand 6 months after varicocelectomy.
The spontaneous pregnancy rate at 6 months follow up in couples with primary infertility and secondary infertility was 18.60% and 31.25% respectively. The difference in their rates was insignificant (P value 0.25) (Table 2). The overall spontaneous pregnancy rate at 6 months was 20.5 %.
| Total cases | Spontaneous pregnancies 6 months after varicocelectomy | p-values | |
|---|---|---|---|
| Primary infertility | 86 (84.31%) | 16 (18.60%) | Chi2=1.3194 |
| Secondary infertility | 16 (15.69%) | 5 (31.25%) | *P=0.251, NS |
Values are represented as number (%).
*P > 0.05- statistically insignificant, NS- Not significant
Table 2: Spontaneous pregnancy rates at 6 months after varicocelectomy. (Chi square test).
It is evident that varicocelectomy results in improvement of semen quality and serum testosterone level in infertile men. Although subinguinal varicocelectomy using an operating microscope is the gold standard (due to its low complication and recurrence rates), loupe- assisted procedure with microvascular Doppler to spare testicular artery is a more feasible option, in terms of outcomes, cost, and availability. None of our study patients had any complications or recurrence following the procedure. Although varicocele treatment results in improvement of semen quality, its impact on pregnancy rate is still ambivalent. We observed a spontaneous pregnancy rate at 6 months after varicocelectomy of 20.5%. This is less than that reported by previous studies. Ficarra et al. reported a spontaneous pregnancy rate of 36.4% while Marmar et al. reported a rate of 33% at a follow-up of 12 months [15,19]. The main reason for this is possibly the shorter follow-up (of 6 months) of our study. We found that the spontaneous pregnancy rate at 6 months after varicocelectomy was higher in men with secondary infertility (31.25%) compared to those with primary infertility (18.60%). But the difference in rates was not significant.
Significant improvement was noted in semen quality and serum testosterone level at 6 months follow-up. This is in conformity with the results of previous studies. (Figure 2) Abdel Meguid et al. reported improvement in all semen parameters and a spontaneous pregnancy rate of 32.9% in the treatment arm vs. 13.9% in the control arm (Table 3) [20]. Elbendary and Elbadry et al. (Table 3) claim that patients with unilateral grade II/III varicoceles and contralateral subclinical varicoceles who underwent bilateral varicocelectomy had significantly higher improvement in semen quality and spontaneous pregnancy rate (Table 3) (of 61.6 % at 9 months) than those who underwent unilateral varicocelectomy [21]. The semen parameters improvement reported in the bilateral varicoclectomy group is in accordance with our study. Nieschlag et al. reported improvement in sperm density at 9-12 months after varicocele repair (Figure 2) [22]. However, they did not find any significant improvement in other semen parameters and serum testosterone level after varicocele treatment. The difference in spontaneous pregnancy rate was not significant between the intervention and control groups, in their study. They reported a spontaneous pregnancy rate of 29% in the intervention group (Table 3). The main limitation of their study was a high dropout rate of 38.4%. Madgar et al. reported significant improvement in all semen parameters after varicocelectomy (Figure 2), even their study was flawed due to a high dropout rate. It also had an exceptionally high pregnancy rate of 60% in the early intervention group (Table 3) [6]. There was no dropout from our study group at 6 months follow-up.
| Study (year) | Sample size | Pregnancy rate (%) | Follow up at (months) |
|---|---|---|---|
| Madgar et al. (1995) | 45 | 60 | 12 |
| Nieschlag et al. (1998) | 125 | 29 | 12 |
| Elbendary and Elbadry (2009) | 145 | 61.6 | 28.3 ± 7.1 |
| Abdel-Meguid et al. (2011) | 73 | 32.9 | 12 |
| Mansour Ghanaie et al. (2012) | 68 | 44.1 | 12 |
Values are represented as number
Table 3: Spontaneous pregnancy rate reported by different studies after varicocele treatment.
Mansour Ghanaie et al. reported a more significant improvement in sperm concentration compared to other parameters after varicocele repair (Figure 2) [23,24]. The mean improvement in sperm concentration, motility, and morphology was by 75%, 15.9% and 14.3% respectively, at 12 months. They reported a spontaneous pregnancy rate of 44.1% in the varicocele repair group at 12 months (Table 3). Varicocelectomy resulted in the highest improvement of sperm density, which improved by 56.45%, at 6 months follow-up in our study. Sperm motility and morphology improved by 47.23% and 18.97% respectively, at 6 months follow-up.
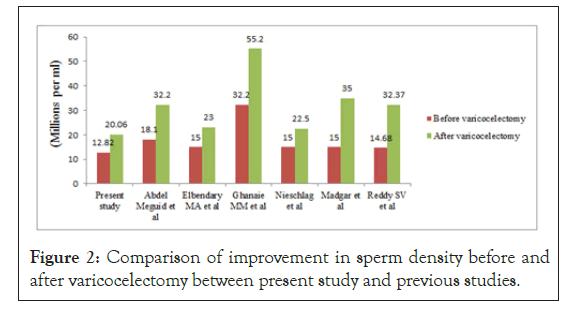
Figure 2: Comparison of improvement in sperm density before and after varicocelectomy between present study and previous studies.
Evers and Collins found no difference in spontaneous pregnancy rates among patients who received varicocele treatment and those who received no treatment, suggesting no fertility merit of varicocele repair [14]. However, in their meta-analyses, they included patients with subclinical varicoceles and also those having normal semen parameters. The spontaneous pregnancy rate was not a primary outcome variable in this study, which added to its shortcomings. Tanrikut et al. (Table 4) (Figure 3) reported a lower level of mean serum testosterone in men with varicoceles than in those without varicoceles [25]. They observed improvement in serum testosterone from 358 ng/dl to 454 ng/dl in men who had undergone bilateral varicocelectomy. Sathya et al. (Table 4) (Figure 3) reported significant improvement in mean serum testosterone levels following varicocelectomy [26]. Abdel-Meguid (Table 4) (Figure 3) reported mean serum testosterone level improvement after varicocelectomy by 44.7 ng/dl (12.9%) [27]. They also reported more significant improvement in men with hypogonadism than in eugonadal men which were 40.1% and 2.01% respectively. In our study mean serum testosterone level improvement at 6 months after varicocelectomy was by 72.84 ng/dl (22.49%). Hsiao et al (Table 4) (Figure 3) reported an increase in mean serum testosterone level after varicocelectomy from 308.4 ng/dl to 417.5 ng/dL with a mean increase of 109.1 ± 12.8 ng/dl. Zohdy et al. (Table 4) (Figure 3) reported improvement in mean serum testosterone level from 379±250.8 ng/dl to 405.1 ± 170.2 ng/dl [28]. In our study, the mean serum testosterone level was noted to improve from 323.90 ± 67.81 to 396.74 ± 40.88 ng/dl at 6 months after varicocelectomy.
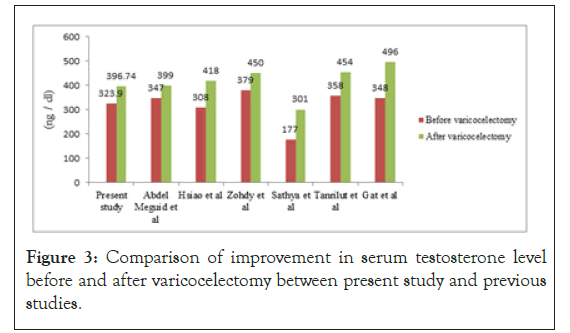
Figure 1: Comparison of improvement in serum testosterone level before and after varicocelectomy between present study and previous studies.
| Study (year) | Mean age of patients(years) | Sample size | P Values | |
|---|---|---|---|---|
| Gat et al. (2004) | 35.1 | 83 | *P<0.001 | |
| Hsiao et al. (2011) | 35.6 | 106 | *P<0.001 | |
| Tanrikut et al. (2011) | 36 | 325 | *P<0.001 | |
| Sathya et al. (2011) | 30 | 100 | *P<0.001 | |
| Zohdy et al. (2011) | 33.8 | 103 | *P<0.001 | |
| Hsiao et al. (2013) | 36.4 | 59 | *P<0.001 | |
| Abdel-Meguid et al.(2014) | 31.7 | 66 | *P=0.004 |
alues are represented as number.
*P <0.01 significant
Table 4: Studies reporting significant improvement in serum testosterone level after varicocele treatment.
Varicocele remains the commonest treatable cause of male factor infertility. It results in a progressive decline of semen quality and serum testosterone levels. Loupe-assisted subinguinal varicocelectomy is an effective option in treating male factor infertility. Varicocelectomy results in induction or enhancement of spermatogenesis and testosterone secretion in men with clinical varicoceles and abnormal semen parameters. Despite the absence of definitive studies on the fertility outcome of varicocelectomy, it is a reasonable treatment option in selective infertile men with semen abnormalities.
Citation: Kale S, Rashid T, Dineshan KM, Cardoza F (2021) Feasibility of Loupe Assisted Subinguinal Varicocelectomy in Treatment of Male Infertility. Andrology . 10:222.
Received: 10-May-2021 Accepted: 24-May-2021 Published: 30-May-2021 , DOI: 10.35248/2167-0250.21.10.222
Copyright: © 2021 Kale S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.