Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2024)Volume 15, Issue 5
Purpose: Marfan Syndrome (MFS) is a congenital systemic connective tissue disorder. It is caused by mutations in the fibrillin-1 gene, a structural protein found in many tissues. The defects lead to widespread clinical manifestation, particularly ocular symptoms. The most common ophthalmic manifestation is Ectopia Lentis (EL), which occurs in up to 75% of patients with Marfan Syndrome. This article describes a novel surgical technique used at the Department of Ophthalmology of the Military Institute of Medicine-National Research Institute. The method involves fixation of the capsular bag-intraocular lens complex with iris retractors. This surgical technique applies to treating lens dislocations of various etiologies, including Marfan syndrome.
Case presentation: An 18-year-old female patient with Marfan syndrome was admitted to the clinic due to deterioration of visual acuity. The patient was diagnosed with lens subluxation in both eyes. Preoperative visual acuity was 20/1000 in both eyes. The novel surgical technique was performed. A binocular visual acuity of 20/20 was achieved. The patient has been followed up for about 3 years after the surgery.
Conclusion: Patients with Marfan syndrome are at a much higher risk of lens subluxation than the general population. Therefore, prompt detection and appropriate treatment are essential. In this case, a novel, minimally invasive and effective technique was used to treat lens subluxation. This technique reduces the risk of postoperative decentration of the capsular bag-intraocular lens complex.
Marfan syndrome; Ectopia lentis; Management; Capsular bag-intraocular lens complex; Iris retractors
Marfan Syndrome (MFS) is a systemic connective tissue disorder affecting mainly the musculoskeletal system, heart, circulatory system, eyes or skin [1]. The prevalence of MFS is variable due to different diagnostic criteria and the location of the studies. The prevalence of MFS is estimated at 1.5 to as high as 17.2 per 100,000 and it is as common in women as in men [2,3].
MFS is congenital in about 75% of cases and inheritance is often autosomal dominant with high gene penetrance [4]. In about 90% of cases, MFS is caused by mutations in the Fibrillin-1 (FBN1) gene, located on chromosome 15 in locus 15q21.1 [5,6]. FBN1 is a structural protein polymerizing into microfibrils in arteries, skin, sclera, cornea and other tissues. Due to the wide occurrence of Fibrillin-1 (FBN1) polymers in human tissues, the clinical manifestations are differentiated. Nevertheless, some ocular disorders are characteristic of MFS and occur more frequently [7]. The diagnosis of MFS is based on the widely used 2010 Ghent-2 nosology [8].
This case report focuses on the most common ocular disorder-Ectopia Lentis (EL).
Ectopia Lentis (EL)-surgical technique
Ectopia Lentis (EL) is the most common ocular manifestation in patients with Marfan syndrome. EL is the abnormal position of the lens within the eyeball. Lens subluxation is the incomplete displacement of the lens in its natural location. On the other hand, lens luxation displaces the lens into the anterior chamber or vitreous cavity. It occurs in MFS with varying frequency from about 30% to about 75% [9-12].
When the lens capsule can be preserved in cases of lens subluxation, iris retractors are used in the Department of Ophthalmology, Military Institute of Medicine-National Research Institute for long-term capsular fixation. It is a technique using a Capsular Tension Ring (CTR) with cauterized iris retractors to stabilize the lens capsule at the site of ligament weakness. This method is minimally invasive and allows the operation to be performed efficiently. It allows the supply of significant lens subluxation with extensive ligament damage. Furthermore, the method provides a predictable surgical course, with a low risk of postoperative decentration of the capsular bag-intraocular lens complex. So, when using a toric lens, it allows simultaneous correction of corneal astigmatism [13,14].
The operation was performed by the experienced surgeon in the case described below.
An 18-year-old woman with MFS was admitted to the clinic, complaining of deteriorating Visual Acuity (VA) for many years. A physical examination revealed subluxation of the native lenses of both eyes. The preoperative Best Corrected Visual Acuity (BCVA) of the right and left eyes was 20/1000. In autokeratorefractometry, the patient presented with significant corneal astigmatism, which was 3.34 diopters in the right eye and 3.25 diopters in the left eye. Table 1 shows the other keratometry and biometry data (Table 1).
| Characteristics | Right eye | Left eye |
|---|---|---|
| AL (mm) | 22.80 | 22.81 |
| ACD (mm) | 3.56 | 2.75 |
| LT (mm) | 4.13 | 4.82 |
| K1 (D) | 37.14 | 37.22 |
| K2 (D) | 40.48 | 40.48 |
| Kmed (D) | 38.81 ± 1.67 | 38.85 ± 1.63 |
| ∆ K (D) | -3.34 | -3.25 |
| CCT (µm) | 570 | 564 |
Note: AL: Axial Length; ACD: Anterior Chamber Depth; LT: Lens Thickness; K1: Flat-axis keratometric value; K2: Steep-axis keratometric value; Kmed: Mean corneal curvature; CCT: Central Corneal Thickness.
Table 1: Characteristics of biometry and keratometry (before surgery).
Sutureless fixation of the capsular bag-intraocular lens complex was performed using a Capsular Tension Ring (CTR) and iris retractors with toric lens implantation. Surgery was first performed in the right eye and after 4 months, in the left eye. In the right eye, fixation was performed with 4 retractors and in the left with 3. An expected result was achieved with both operations. Postoperative BCVA was 20/20 in both eyes. After surgery, the residual astigmatism was 1.0 and 0.5 diopters, respectively. The patient has been followed for about 3 years after the surgery (Figures 1a-1d).
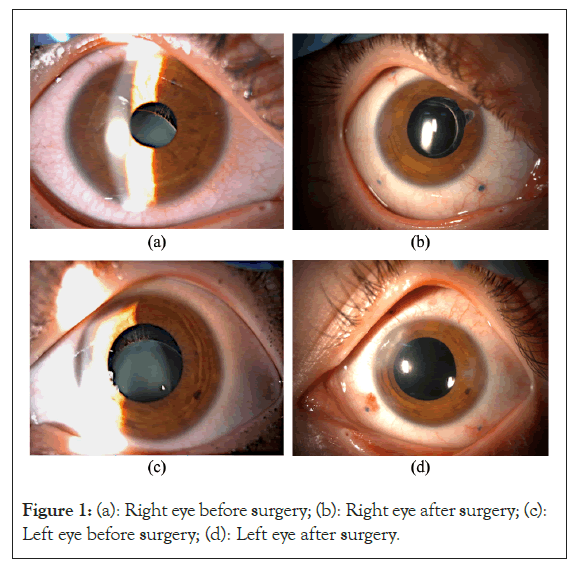
Figure 1: (a): Right eye before surgery; (b): Right eye after surgery; (c): Left eye before surgery; (d): Left eye after surgery.
Corneal flattening occurs more commonly in Marfan syndrome than in the general population. Additionally, authors usually describe not only lower corneal curvature but also more frequent corneal astigmatism in MFS [15-17]. In our patient, we also observed binocular corneal astigmatism, which averaged 3.30 diopters.
Salchow, et al., [7] showed that corneal flattening in MFS is more significant than in the control group (537.35 μm ± 40.64 μm vs. 552.95 μm ± 39.57 μm). In addition, the mean corneal curvature (Kmed) in patients with Marfan syndrome is significantly lower (40.86 μm ± 2.13 μm vs. 42.55 μm ± 1.55 μm). On the other hand, corneal astigmatism was 1.50 Dcyl ± 1.22 Dcyl, while the control group had 0.88 Dcyl ± 0.49 Dcyl.
Konradsen, et al., [18] reached similar conclusions and showed that the corneal thickness in patients with Marfan syndrome was 485 μm ± 54.5 μm, which was statistically significantly lower than that of the control group. In addition, the mean corneal curvature (Kmed) was 42.2 μm ± 1.9 μm and corneal astigmatism was 1.1 Dcyl ± 0.9 Dcyl, respectively.
Patients with MFS have significantly increased eyeball Axial Length (AL). Gehle, et al., [17] showed that the mean AL was 24.25 mm ± 1.74 mm. Similar results were presented by Konradsen, et al., [18] in which the mean AL was 24.73 mm. The elongation of the eye contributes to significant myopia in these patients. Myopia ≥ 3 diopters occur in about 34% to 44% of MFS and is one of the systemic criteria in the 2010 Ghent-2 nosology [19]. According to Suwal, et al., [11] the mean Spherical Equivalent (SE) was -12.34 D ± 8.85 D. We also observed significant myopia in our patient, which was -15 D in both eyes before surgery. Nevertheless, our patient AL was 22.80 mm in the right eye and 22.81 mm in the left eye, respectively.
Ocular elongation in Marfan syndrome can also lead to retinal tension and the risk of Retinal Detachment (RD). Some authors estimate the incidence of RD in MFS to be 10%-15%. According to Nemet, et al., [20] the risk of retinal detachment in patients with MFS correlates with the eyeball Axial Length (AL). Patients with RD had an average AL of 28 mm.
Glaucoma is more common in MFS than in the general population. The prevalence is estimated to be as high as 30% in patients with MFS. The most common type is open-angle glaucoma. Lens dislocation into the anterior chamber can result in secondary glaucoma in about 8% of cases. Nevertheless, most MFS patients have lower Intraocular Pressure (IOP) than controls. In the study by Salchow, et al., [7] the mean IOP in patients with Marfan syndrome was 14.41 mmHg ± 3.51 mmHg.
One of the surgical treatment methods is removing the subluxated lens. This method leads to aphakia, which contributes to high refractive error. Therefore, it is mandatory to use spectacle correction or contact lenses. In other cases, removal of the subluxated lens and implantation of an Intraocular Lens (IOL) can be conducted. If the posterior lens capsule is damaged, Anterior Chamber Intraocular Lenses (ACIOL) or Posterior Chamber Intraocular Lenses (PCIOL) can be implanted. Due to the significant risk of side effects (such as glaucoma or corneal damage), ACIOLs usually are eliminated by PCIOLs. These lenses are fixated on the Iris Fractal Intraocular Lens (IFIOL) or the Sclera Fractal Intraocular Lens (SFIOL) [21].
In cases where the lens capsule is intact, lens dislocation surgery using the Modified Capsular Tension Ring (MCTR) by Cionni, et al., [22] is a standard surgical procedure. In 2003, Cionni, et al., [22] described using a Modified Capsular Tension Ring (MCTR) and Posterior Chamber Intraocular Lens (PCIOL) in patients with Weill-Marchesani syndrome, idiopathic lens ectopia and Marfan syndrome. It has significantly improved visual acuity (BCVA ≥ 20/40) in almost 89% of patients. Also, it resulted in better centration of the capsular bag and PCIOL.
Nevertheless, the presented method used in the Department of Ophthalmology, Military Institute of Medicine-National Research Institute, is an alternative means of lens dislocation surgery. This method is used in our clinic for patients with different etiologies of ectopia lentis. In addition to patients with MFS, it is also successfully used in patients with post-traumatic lens subluxation.
In summary, this case report provides a comprehensive overview of Ectopia Lentis (EL) within the context of Marfan Syndrome (MFS), highlighting its significance as the most prevalent ophthalmic manifestation associated with this condition. The detailed examination underscores the critical role that recognizing and addressing EL plays in both the diagnostic and treatment processes for MFS patients. The introduction of a novel surgical technique in the presented case demonstrates promising effectiveness and offers a potential advancement in the management of lens subluxation. Given the complexity and variability of MFS, future research should focus on a comparative analysis of various surgical approaches to optimize treatment outcomes. Such studies would contribute valuable insights into the most effective strategies for lens stabilization, ultimately improving patient care and quality of life for those affected by Marfan Syndrome (MFS). Comprehensive evaluations and continued innovation in surgical methods remain crucial in advancing ophthalmic treatment protocols for this condition.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mazurek W, Rekas B, Krix-Jachym K, Blagun N, Rekas M (2024) Fixation of the Capsular Bag-Intraocular Lens Complex as a Surgical Treatment of Lens Subluxation in Marfan Syndrome. J Clin Exp Ophthalmol. 15:987.
Received: 26-Aug-2024, Manuscript No. JCEO-24-32444; Editor assigned: 28-Aug-2024, Pre QC No. JCEO-24-32444 (PQ); Reviewed: 11-Sep-2024, QC No. JCEO-24-32444; Revised: 18-Sep-2024, Manuscript No. JCEO-24-32444 (R); Published: 27-Sep-2024 , DOI: 10.35248/2155-9570.24.15.987
Copyright: © 2024 Mazurek W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.