Orthopedic & Muscular System: Current Research
Open Access
ISSN: 2161-0533
ISSN: 2161-0533
Research Article - (2023)Volume 12, Issue 2
Background: Venous Malformations (VMs) are the most common vascular malformations which can be classified as focal, multifocal, or diffuse types. VMs have a higher incidence in muscle than skin, subcutaneous tissue. But the risk of focal venous malformations with muscle involvement is not well defined.
Objective: The aim of our study was to observe clinical features of focal VMs and make risk evaluation of them based on positions that are associated with invasion of muscle.
Methods: This is a single-center, retrospective review of patients treated for focal VMs between February 2021 and February 2022.
Results: We assessed 26 patients focal VMs with 47 lesions; 18 (69%) were unifocal, 3 (12%) were dual-focal and 5 (19%) were multifocal type VMs, and 29 (62%) were intramuscular VMs. Of all focal VMs, 32 (68%) lesions arose in the extremities, 10 (21%) in the head and neck region and 5 (11%) in the torso. The three groups were no statistical difference for the intramuscular VMs, 19 (68%) arose in extremities, 6 (21%) in the head and neck region and 3 (11%) in the torso. But the lower limbs intramuscular VMs had a significantly elevated risk of focal VMs Relative Risk (RR), 1.7; 95% Confidence Interval (CI), (1.148-2.394).
Limitations: Retrospective, single-institution study.
Conclusion: Intramuscular involvement of the body should be considered in focal VMs. The lower limbs intramuscular VMs had a significantly elevated risk of focal VMs.
Muscle; Intramuscular; Vascular anomaly; Vascular malformation; Venous; Venous malformation
Venous Malformations (VMs) are slow-flow vascular lesions and the most common vascular malformations. VMs can be classified as focal, multifocal, or diffuse types [1]. Common VMs are mostly sporadic and unifocal, and account for more than 90% of VMs [2]. Focal VMs are solitary, localized, and predominantly non-familial [3]. VMs are usually noted at birth, but they grow proportionally with the child and exhibit progressive ectasia with age [4].
Non-familial less than 1% of all venous malformations are intramuscular [5]. Intramuscular VMs are generally not evident at birth but manifest itself later in life [6]. The intramuscular VMs may be highly symptomatic and show a progressive enlargement which induces a gradual worsening of the symptoms. They typically present with swelling and pain and cause significant functional imitations [7].
The purpose of our study was to describe the clinical characteristics of focal VMs in children and the risk of muscle involvement.
This study was reviewed and approved by the children's hospital affiliated to Shandong university institutional review board. The Shandong provincial clinical research center for children's health and disease database was queried for all patients with a diagnosis of VMs from February 2021 and February 2022. Patients were included in the study if all 3 of the following criteria were met.
• A vascular anomalies specialist (general surgeon,
interventional radiologist, pediatrician) diagnosed focal VMs.
• Diagnostic (MRI) Magnetic Resonance Imaging or ultrasonic
was available.
• There were clinical photographs of focus. Diagnostic (DSA)
Digital Subtraction Angiography was obtained in cases with
equivocal imaging and for therapeutic purposes. Focal VMs
combined with unifocal, dual-focal and multifocal type. We
excluded multifocal VMs associated with (BRBNS) Blue
Rubber Bleb Nevus Syndrome and (CMVM) Cutaneo-Mucosal Venous Malformation (Figure 1).
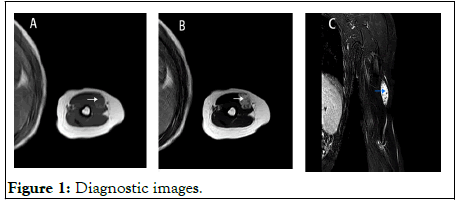
Figure 1: Diagnostic images.
MRI showed that the lesions are isolated, with smooth edges and clear boundaries. The lesions to be isointense or hypointense to surrounding muscle on T1-weighted sequences; A) And hyperintense on T2-weighted images; B) There are punctate hypointense on fat suppression T2-weighted images in hyperintense lesions; C) A, B and C are the same lesion.
Clinical data including name, Inpatient number, gender, age at presentation to our center, diagnostic imaging or ultrasonic, and combined focal VMs were collected from medical records by using standardized data abstraction forms by 2 reviewers (JZ and ZL).
Clinical photographs of focal VMs were reviewed by 1 pediatrician (JZ), 1 interventional radiologist (JL) and 1 general surgeon (LW) blinded to patient outcomes and categorized by subtype into unifocal, dual-focal, or multifocal VMs. Focal VMs were solitary and localized. Multifocal VMs were noncontiguous. Intramuscular VMs was determined by the presence of venous malformation on MRI and ultrasonic by 2 interventional radiologists (JL and ZL). A radiologist specialized in vascular malformations (LG) was blinded to clinical data and reviewed all focal VMs MRI studies that did not include a comment on intramuscular VMs.
Statistical analysis
Descriptive characteristics were compiled according to lesion type of VMs. Interquartile ranges and medians were reported for nonparametric data. Bivariate comparisons were performed with Chi-square or fisher’s exact tests for categorical variables, and Relative Risks (RR) were generated when appropriate. All tests were 2 sided, with P values less than or equal to 0.05 considered to be statistically significant. All statistical analyses were performed with IBM SPSS statistics 21.
Cohort characteristics
526 patients diagnosed with VM and vascular malformations were screened; 26 patients met the inclusion criteria with 47 lesions. 16 (62%) of these patients were female and 10 (38%) were male. 18 (69%) were unifocal, 3 (12%) were dual-focal and 5 (19%) were multifocal VMs. Of all focal VMs lesions, 32 (68%) lesions arose in the extremities, 10 (21%) in the head and neck region and 5 (11%) in the torso; 28 (60%) on the left and 19 (40%) on the right. The lesions of 5 multifocal VMs all arose in the extremities (Table 1).
| Characteristics | Unifocal | Dual-focal | Multifocal | P |
|---|---|---|---|---|
| n | 18 | 3 | 5 | |
| Gender, n (%) | 0.24# | |||
| Female | 11 (61) | 3 (100) | 2 (40) | |
| Age at VM onset, y, median (range) | 1.8 (0.4-7.5) | 2.5 (0-12) | 5.2 (0.4-13) | 0.085* |
| Age at VM diagnosis, y, median (range) | 4 (0.4-9) | 4.8 (3-12) | 5.3 (1-13) | 0.146* |
| Lesion location, n (%) | 0.068§ | |||
| Extremities | 8 (44) | 4 (67) | 20 (87) | |
| Head and neck | 7 (39) | 1 (17) | 2 (9) | |
| Torso | 3 (17) | 1 (17) | 1 (4) | |
| The reason of seeking medical services, n (%) | ||||
| The mass gradually increased | 7 (27) | 3 (12) | 3 (12) | |
| Pain | 4 (15) | 2 (8) | 0 (0) | |
| Dysfunction | 2 (8) | 0 (0) | 0 (0) | |
| #Chi-square test. *Wilcoxon rank sum test. § Fisher’s exact test. |
||||
Table 1: Characteristics of 26 patients with focal VMs according to type.
The lesions were noted before 1 year old in 36 percent of the patients; 60 percent presented at 0 years to 5 years, 40 percent at 6 years to 13 years. The most common presenting symptoms were swelling or mass (100%), pain (n=6, 23%), and functional limitations (n=2, 8%), which were often because of pain or the location of the mass. 13 patients (50%) had an growing gradually mass at presentation, occurring especially at motion or crying.
There was no significant difference in gender, age at diagnosis or lesion location based on VM subtype. The median age at diagnosis of VM was 4 years for unifocal and younger than 1.3 year for multifocal. Intramuscular VMs was diagnosed later than extra muscular VMs in focal VMs; the median age of intramuscular is 5.3 years and 4 years for extra muscular tissue.
Risk of intramuscular venous malformation
Of the 45 lesions (two were excluded because of lack of MRI), 28 (62%) were intramuscular VMs, 17 (38%) were located in extra muscular tissue. There was no significant difference in gender, age at diagnosis, lesion location or subtype based on lesion depth. In intramuscular focal VMs, multifocal VMs was the most common type (n=14, 50%), followed by unifocal VMs (n=11, 39%) and dual-focal VMs (n=3, 11%). For the intramuscular focal VMs, 19 (68%) arose were in the muscular of extremities, 6 (21%) in the head and neck region and 3 (11%) in the torso. But the lower limbs intramuscular VMs had a significantly elevated risk of focal VMs Relative Risk (RR), 1.7; 95% Confidence Interval (CI), (1.148-2.394) (Table 2). The lower limbs intramuscular VMs also had a significantly elevated risk of focal VMs in extremities Relative Risk (RR), 1.8; 95% Confidence Interval (CI), (1.109-2.922) (Table 3).
| Characteristics | Intramuscular | Extra muscular | p |
|---|---|---|---|
| n | 28 | 17 | |
| Gender, n (%) | 0.079# | ||
| Female | 14 (50) | 13 (76) | |
| Age at onset, y, median (range) | 4.4 (0-13) | 2.5 (0.4-10.5) | 0.454* |
| Age at diagnosis, y, median (range) | 5.3 (0.8-13) | 4 (0.4-11) | 0.482* |
| Lesion location, n (%) | 0.998§ | ||
| Extremities | 19 (68) | 11 (65) | |
| Lower limbs (9), upper limb(1) | Lower limbs (10), upper limb (10) | ||
| Head and neck | 6 (21) | 4 (23) | |
| Torso | 3 (11) | 2 (12) | |
| Type, n (%) | 0.753§ | ||
| Unifocal | 11 (39) | 7 (41) | |
| Dual-focal | 3 (11) | 3 (18) | |
| Multifocal | 14 (50) | 7 (41) | |
| #Chi-square test. *Wilcoxon rank sum test. §Fisher’s exact test. |
|||
Table 2: Characteristics of 45 lesions with focal VMs according to lesion location.
| Characteristics | Relative risk (95% CI) |
|---|---|
| Lesion location | |
| Extremities | 1.056 (0.644-1.731) |
| Head and neck | 0.955 (0.542-1.682) |
| Torso | 0.960 (0.451-2.042) |
| Lower limbs | 1.658 (1.148-2.394) |
| Type | |
| Unifocal | 0.971 (0.606-1.551) |
| Multifocal | 1.143 (0.726-1.799) |
Table 3: Risk of intramuscular involvement.
Here, we found that individuals with distinctive focal VMs, who have unifocal and multifocal, but do not satisfy the clinical criteria for BRBN and VMCM. Because there is less attention to focal VMs, so few papers specifically analyse focal VMs, while many papers merge together focal and diffuse VMs. In this study, we were exclusively considered focal VMs and intramuscular VMs.
Venous malformations occurred in every muscle group, most often in the head and neck and extremities. VMs have a higher incidence in muscle than skin, subcutaneous tissue, viscera, or intracranial vasculature. VMs tend to be in contiguous muscle groups, perhaps because they evolved during embryonic development along neurovascular pathways [8,9]. The focal VMs we studied are the same as their results, but more common in the extremities, 28 (62%) lesions in muscle. The partial lesions of 5 multifocal VMs are in contiguous muscle groups; other remaining lesions are distant. The most common intramuscular VMs locations were in the lower leg, upper leg, and upper arm [10]. But in focal VMs, the lower limbs intramuscular VMs had a significantly elevated risk. Unlike skin VMs, intramuscular VMs are generally not evident at birth but manifest itself later in life. As the dysmorphological features of VMs predispose to stagnant blood flow, these lesions can spontaneously thrombose and thus present with swelling and pain.
BRBN is a rare, sporadically occurring disorder characterized by multiple widely distributed cutaneous and internal VMs [11]. Patients have tens to hundreds of lesions that often increase in size and number with age. Cutaneous lesions are generally small, measuring less than 1 cm-2 cm, blue to purple in color, with a predilection for the skin, mucosae and gastrointestinal tract [12]. On our study suggests, the multifocal of focal VMs, measuring more than 1 cm-2 cm, involve the muscle, skin, subcutaneous and spaces between bone and muscles tissue, without viscera or intracranial vasculature.
The condition multiple CMVM is characterized by the presence of small, multifocal bluish cutaneous and/or mucosal venous malformations. They are usually present at birth, also increase in size and number with age. The malformations range in size from 1 mm to 1 cm. Larger lesions can invade subcutaneous muscles and cause pain. Family inspection is essential in this autosomal dominant disease, with an estimated penetrance of 90% by the age of 20 years. On our study suggests the multifocal of focal VMs involve the muscle, skin, subcutaneous tissue and spaces between the bone and muscles, without viscera or intracranial vasculature. Only 19% multifocal type VM, They are different from VMCM and BRBN. Given that no a large number of patients at our institution, as such, the characteristic of focal VMs involvement are likely underrepresented in this study. Because of the shorter follow-up and only a single evaluation in many patients, we cannot exclude the possibility of some patients developing more lesions later. Patients who are initially successfully managed medically must be followed closely, however, because they may develop new focus or symptoms that then warrant re-evaluation and procedural intervention. For all patients, we found that percutaneous sclerotherapy resulted in clinical improvement after only one procedure. We will present specific treatment details in the next article.
The authors declare that they have no competing interests.
Not applicable.
The data supporting the findings of this study are available within the article materials.
The authors want to express their gratitude for their support for patient data retrieval of the medical department, medical record room, information department and other management departments. The departments were not involved in the collection, analyses and interpretation of data, in the writing or in the decision to submit the manuscript.
The study protocol was approved by the ethics committees for children's hospital affiliated to Shandong university. All methods were carried out in accordance with relevant guidelines and regulations.
Informed consent to participate was obtained from the parents of the patients.
Informed consent was obtained from the participants or their guardians to publish their personal information in the study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhou J, Guo L, Wang L, Li J, Liu Z, Sun J (2023) Focal Venous Malformations and Risk of Muscle Involvement in Children. Orthop Muscular Syst. 12:356.
Received: 26-Dec-2022, Manuscript No. OMCR-22-21169; Editor assigned: 29-Dec-2022, Pre QC No. OMCR-22-21169 (PQ); Reviewed: 12-Jan-2023, QC No. OMCR-22-21169; Revised: 24-Mar-2023, Manuscript No. OMCR-22-21169 (R); Published: 31-Mar-2023 , DOI: 10.35248/2161-0533.23.12.356
Copyright: © 2023 Zhou J, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.