Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Review Article - (2020)
Anal cancer is a serious health problem in HIV-positive Men who have Sex with Men (MSM), and precursor lesions like anal intraepithelial neoplasia; are well defined. Anal intraepithelial neoplasia (AIN), a human papillomavirus (HPV)- associated anal cancer precursor lesion, is frequent among human immunodeficiency virus (HIV)-positive men who have sex with men and women (MSMW). There is a paucity of data published on the progression of high-grade AIN to invasive cancer as well as on clinical and virological characteristics comparing anal margin and anal canal carcinoma. Men who are infected with HIV and MSM are at particularly high risk for persistent HPV infection and HPV-induced lesions. The treatment of high-grade squamous intraepithelial lesions (HISL) in HIV positive MSM associating the adjuvant vaccine against HPV is likely to be cost-effective, with benefits reported in the age group above 38 years. It is convenient to design large controlled studies that enroll the MSM population infected with HIV, as in our patient; to evaluate the benefits of the HPV vaccine.
Anal intraepithelial neoplasia (AIN); Men who have sex with men (MSM); Men who have sex with men and women (MSMW); High-grade squamous intraepithelial lesions (HISL); ELISAP; HIV; HPV
A 38-year-old Venezuelan migrant was admitted to our hospital. He was a resident in a rural zone of Antioquia, he used to work as a street vendor, he was a single man with no children, he was a man who had sex with men and women (MSM); and he was newly diagnosed with HIV infection with a viral load of 70,144 copies / ml (Log 4.85) and a CD4 count of 272 cells / μl undergoing treatment with ABC / 3TC + EFZ (Table 1).
| Study | Technique | Report |
|---|---|---|
| CD4 count | Flow cytometry | 272.0 cells/Ul |
| HIV viral load. | Immunoassay Chemiluminescent Microparticles (CMIA). | 70,144 copies/ml (Log 4.85). |
| Perianal lesion biopsy. | Anatomy pathological, immunohistochemistry. | Squamous epithelium hyperplastic with acanthosis and koilocytic changes in the upper strata. Squamous papilloma. |
Source: Social Enterprise Reference Laboratory of La Maria Hospital.
Table 1: Relevant studies technique and report of laboratories released during hospital estancy.
At the time of admission, he reported approximately 6 monthold extensive verrucous lesions in the perineal and genital region and 1 week of fever, purulent discharge from the lesions and unquantified weight loss.
He presented with a perianal verrucous appearing lesion on the left buttock, approximately 12 cm long, 4 cm wide and 2.5 cm thick (Figure 1); with satellite lesions in the intergluteal groove. Suggestive of giant perianal condylomatosis and associated superinfection.
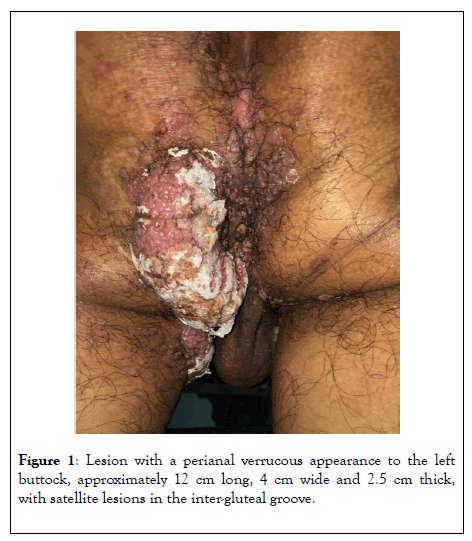
Figure 1: Lesion with a perianal verrucous appearance to the left buttock, approximately 12 cm long, 4 cm wide and 2.5 cm thick, with satellite lesions in the inter-gluteal groove.
Flexible rectosigmoidoscopy was performed which did not report any visible lesions in the rectal mucosa or anal canal, a biopsy of the perianal lesion was taken, which reported cytopathic changes due to HPV (Figure 2) classified as squamous papilloma. The patient was treated with topical podophyllin solution with slight improvement in further controls, but a transient discharge colostomy was required prior to complete surgical resection of the perianal lesion.
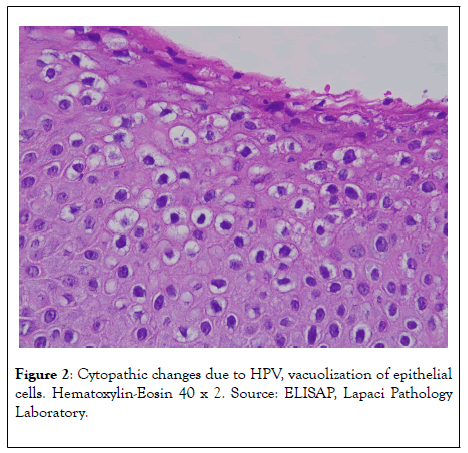
Figure 2: Cytopathic changes due to HPV, vacuolization of epithelial cells. Hematoxylin-Eosin 40 x 2. Source: ELISAP, Lapaci Pathology Laboratory.
The human papilloma virus (HPV) is an infectious agent of worldwide distribution whose importance in health lies fundamentally in that it is the main causative agent of cervical cancer in women and cancer of the anal and oropharyngeal canal in men. In 1994, Zur Hausen and de Villiers described the malignancy of cells infected with HPV after having hypothesized years ago that the latter was responsible for uterine cervical cancer [1].
Secondarily, infection by some serotypes of this virus is also responsible for genital and skin warts, with different degrees of oncogenic potential. According to CDC statistics, in the United States there are 79 million people infected with HPV and the incidence is 14 million cases per year, this same entity has established that the serotypes associated with the majority of cancer cases attributable to HPV infection are related to serotypes 16 and 18, with cervical and anal canal cancer being the most frequent in women and that of the oropharynx and anal canal in men [2,3]. In Colombia, a study was carried out in 2009 with 217 women in 2 large cities in the country that included characterization of the HPV serotypes that were causing abnormalities in biopsies of the cervix. In these women, serotype 16 was determined to be the most highly prevalent followed by 18, which is particularly important because cervical cancer continues to be an important cause of mortality, in middle-income countries like ours [4,5].
As for the properties of papilloma viruses, these are naked viruses with a double circular DNA chain genome, there are 5 genera of the papilomaviridae family, which are linked to infections in humans, of these the genus Alfapapillomavirus groups are those of greater clinical interest, since species 7 and 9 include serotypes 18 and 16, causing intraepithelial neoplasms and invasive carcinoma, and species 10 includes serotypes 6 and 11, causing condylomata acuminata. Papilloma viruses as a whole have tropism for squamous cells of mucosae and skin. The infection is acquired by close contact between an uninfected mucosa or skin and a papillomatous lesion [6]. The virus enters through any microlaceration on the skin or mucosa and attaches to the heparan sulfate proteoglycan sulfate (HSPG), from there it is transferred to HSPG present in the cell membrane of basal layer cells, and by mechanisms not yet well elucidated, it is endocytosed by mechanisms mediated by clathrin and caveolin, protein replication and synthesis occurs in an ascending way in the cells of the upper strata, those that are more differentiated, until reaching the most superficial keratinocytes where the final maturation and virion release occurs [7,8].
In HIV positive people, HPV infection is of particular importance, because the immunodeficiency state favors the formation or unfavorable evolution of condylomatous lesions and also favors persistent infection and malignant transformation of squamous and glandular cells in infected areas [9]. It has been described that in men who have sex with men there is a strong association between the low-risk serotypes causing condyloma and the high-risk serotypes of squamous cell and glandular cell carcinoma in the anal canal, this implies that lesions that are generally benign, still carry a risk of malignancy due to coinfection with low and high risk serotypes, furthermore, since ART increases patient survival and prevents immune deterioration, non-AIDS-defining diseases such as anal canal cancer in In relation to HPV infection, have gained ground as causes of morbidity and mortality in HIV positive patients [10,11].
Condylomatous lesions usually present an evolution of 2 to 3 months from the time the infection is acquired to the development of the lesions. On the genitals these are exophytic with a rough surface similar to cauliflower texture and are usually located in the perineum, on genitals and in the anus. Containment of infection is linked to cellular immunity, which would explain why in patients who are immunosuppressed by HIV or as part of a transplant protocol, recurrent lesions or a more morbid course appear, unlike the simple acuminate condyloma, giant condylomas tend to deepen and displace the surrounding tissues respecting the basement membrane, due to this more aggressive behavior, giant acuminate condyloma is considered a lesion with a greater oncogenic potential than simple condylomas [12-14].
Regarding the treatment of established lesions, surgical resection has been considered the first option, traditionally it has been proposed to leave a free margin around the lesion, since giant condylomata acuminata is a rare disease, there is no consensus regarding the ideal surgical treatment [14,15]. It has also been proposed that treatment with imiquimod or podophyllin are very safe options with cure rates of up to 77% in the first to 45 to 77% for the second, however, the first drug has not been extensively studied on immunosuppressed people, thus its use is not generally recommended [16,17]. In patients with risk behaviors for contracting HPV infection, or with established condylomatosis, an active search should be made for malignant intraepithelial lesions, a standard periodicity has not been established, but it is accepted that, in people with risk factors, mainly Pap smear and anoscopy are performed in men receptive of anal intercourse, other authors recommend pap smear and HPV typing [18,19]. In women, it has been proposed that cervical cytologies be performed annually, after performing 2 within the first year after the diagnosis of HIV [20]. Currently there is evidence that studies the possibility of extending the pap smear intervals by performing the HPV DNA test as a co-test after the diagnosis of HIV, other authors propose that women with CD4 T lymphocyte counts greater than 350 cells / ml are screened the same as the general HIV negative population [21].
More studies and consensus are required to better elucidate the evolution of condylomatous lesions in HIV-positive people, and the establishment of treatment protocols aimed at improving functionality and aesthetic implications and requiring the malignant component to be ruled out in patients affected by condylomatous lesions; like the ones we present in this text. The greatest threat of papillomavirus infections will always be the malignant transformation of the lesions they cause, which is why studies in the male population in HIV positive patients are required, since the use of the HPV vaccine and the reduced rates of grades 2 and 3 intraepithelial neoplasia among men who have sex with men with a favorable safety profile and could help reduce the risk of anal cancer [22].
In our patient, an anatomopathological differential diagnosis was established with entities such as: Buschke-Lowenstein tumor: due to the benign nature of the squamous papilloma and not having penetrated deep tissues, and with the epidermoid tumor: due to respecting the basement membrane and not metastasizing [23].
Giuliano et al. reported a 90.4% efficacy for the quadrivalent vaccine (HPV) for external genital lesions (condylomata acuminata) associated with HPV-6, 11, 16 or 18 serotypes; in healthy subjects and predominantly men who have sex with women (MSW) [24].
The vulnerable population should be counseled, initially considering an acceptance survey for mass immunization, as a German study on 33 MSM infected with HIV and born to Latin American migrants; found that the only limitation to undergo the immunization schedule was the Lack of knowledge about the safety of the vaccine in relation to HIV infection and its high costs. The countries of origin were: Chile: 1(3.0%), Colombia: 4(12.1%), Cuba: 17(51.5%), Dominican Republic: 1(3.0%), Honduras: 2(6.1%), Mexico: 4(12.1%), Venezuela: 4(12.1%) [25].
It is the task of the medical community to be alert to the presence of condylomatous lesions, especially in immunosuppressed patients; since besides the serious, extensive and aesthetically disfiguring affectation; they may be infected by high-risk serotypes that carry neoplastic potential for this population.
No additional negative effects of the vaccine were found in the HIV positive population, when compared to the general population [26].
Citation: Martinez LLR, Berlinghieri JDP, Matute GT (2020) Giant Acuminated Condyloma in a HIV Positive Migrant Patient: Is There a Benefit on Giving the HPV Vaccine To the Men Who Have Sex With Men Population? Case Report and Literature Review. J Antivir Antiretrovir. 12:203. DOI: 10.35248/1948-5964.20.12.203
Received: 20-Jul-2020 Accepted: 05-Aug-2020 Published: 12-Aug-2020
Copyright: �© 2020 Martinez LLR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.