
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2020)Volume 11, Issue 2
Objective: In children, the grading of Bag-Mask Ventilation (BMV) difficulty and its association with difficult laryngoscopy/intubation has not been well established. This study aimed to evaluate the grading for BMV difficulty and determine its association with difficult laryngoscopy/intubation in a normal airway pediatric population.
Methods: This prospective cohort study was conducted in children aged ≤9 years who underwent general anesthesia and oroendotracheal tube intubation between September 2008 and December 2012. Difficult laryngoscopy was defined as a Cormack–Lehane laryngoscopic view grade of 3 or 4. Difficult intubation was defined as the occurrence of at least two of the following: 1) at least three intubation attempts using direct laryngoscopy by experienced personnel (excluding first intubation attempts); 2) intubation time >300 s; and 3) occurrence of desaturation (SpO2<95%). The use of open airway maneuvers, including continuous positive airway pressure (CPAP), oropharyngeal airway (OPA), and two-person ventilation (TPV), or unsuccessful BMV were also considered. The association between BMV difficulty and difficult laryngoscopy/intubation was assessed using multivariate logistic regression with adjusted odds ratios (OR), 95% confidence intervals (CIs), and area under the receiver operating characteristic curve (AUC).
Results: The incidence of difficult laryngoscopy/intubation was 6.4% (49/765). The categories of BMV difficulty were grade 0 (easy BMV without requiring an open airway maneuver, n=308), grade 1 (easy BMV after applying CPAP, n=368), grade 2 (successful BMV after inserting an OPA, n=16), grade 3 (successful BMV after applying TPV, n=71), and grade 4 (unsuccessful BMV after applying all airway maneuvers, n=2). Difficult BMV was defined as a BMV grade of 3 or 4 (v/s grades 0-2). After adjusting for age, body weight, history of snoring, type of operation, use of neuromuscular blocking agents, and first laryngoscopist, BMV difficulty was significantly associated with difficult laryngoscopy/intubation (adjusted OR [95% CI]=2.5 [1.1-5.5], sensitivity 0.59, specificity 0.74, AUC=0.70).
Conclusion: A BMV grade of 3 (requiring TPV) or 4 (unsuccessful BMV) was associated with difficult laryngoscopy/ intubation in a pediatric population.
Grading; Bag-mask ventilation difficulty; Open airway maneuver; Difficult laryngoscopy; Difficult intubation
The occurrence of a difficult airway during pediatric anesthesia is considered a critical complication, particularly in small children with airway abnormalities [1]. However, when this complication occurs unexpectedly, it is considered even more crucial. A difficult airway can arise from a number of factors, including the inability to obtain a mask seal, difficulty in visualizing the vocal cords (i.e. difficult laryngoscopy), or problems passing the endotracheal tube through the vocal cords (i.e. difficult intubation) [2].
The incidence of unexpected difficult laryngoscopy/intubation in children has been reported to vary from 1.2% to 4.8% and is higher in children with congenital heart disease [1,3-6]. Predictors of unexpected difficult laryngoscopy/intubation include infancy, associated syndromes or congenital abnormalities, and a diagnosis of obstructive sleep apnea [1,3-7]. The incidence of unexpected bag- mask ventilation (BMV) difficulty in children is around 6.6% [6], which is similar to that reported in adults [8,9].
The association between BMV difficulty and difficult laryngoscopy/ intubation has been well established in adults; however, this issue remains uncertain in the pediatric population [10,11]. Both BMV difficulty and difficult laryngoscopy/intubation share several common predictors, such as infancy and obstructive sleep apnea [6,7]. However, to our knowledge, no previous study has evaluated the grading and cut point of BMV difficulty to predict the occurrence of unanticipated difficult laryngoscopy/intubation in children. Therefore, in this study, we aimed to evaluate the grading of BMV difficulty and its association with unanticipated difficult laryngoscopy/intubation in a normal airway pediatric population.
This prospective cohort study was conducted after approval was granted by the Ethics Committee of the Faculty of Medicine at Prince of Songkla University (Chairperson Associate Professor Verapol Chandeying) on August 26, 2008 (EC 510020812, ClinicalTrials. gov: NCT02823392). For the study, we recruited children aged ≤ 9 years, with an American Society of Anesthesiologists physical status of 1-3, who presented for general anesthesia in conjunction with oroendotracheal tube intubation as part of elective surgery at Songklanagarind Hospital between September 2008 and December 2012. Written informed consent and assent were obtained from the children's parents or guardians. Patients were excluded if they were found to have difficult airways, airway anomalies or syndrome- related difficult airways, the occurrence of active pulmonary disease, or the incidence of preoperative oxygen saturation at room air <95%.
Study protocol and anesthesia practice
Patient demographic characteristics were recorded by a research assistant during the pre-induction period. Standard monitoring procedures, including non-invasive blood pressure, pulse oximetry, electrocardiography, and capnography, were performed for all patients prior to starting general anesthesia. All patients received general anesthesia using oroendotracheal tube intubation. Induction techniques included either the inhalation of an anesthetic agent, such as N2O-O2-sevoflurane, or the administration of an intravenous agent, such as thiopental (5-7 mg/kg) or propofol (2-3 mg/kg). The patient’s head was placed in a neutral position and under a small head ring to prevent head movement during induction. BMV was performed during induction with 100% O2. If BMV was possible, a non-depolarizing muscle relaxant (vecuronium/rocuronium/cisatracurium) was administered to facilitate the laryngoscopy procedure. If BMV was difficult or impossible, propofol or succinylcholine (1.5 mg/kg) was given to achieve deep anesthesia and to facilitate the intubation procedure. Anesthesia personnel who performed the BMV were also tasked with performing the first laryngoscopy. The Miller blade was used in infants, whereas the Macintosh blade was used in children aged >1 years or those with a body weight of >10 kg.
The laryngoscopists included anesthesia residents (with greater than 1 year experience), nurse anesthetists (with at least 1 year training), and anesthesiologist staff. The number of intubation attempts, the Cormack-Lehane laryngoscopic view, intubation time in seconds, and occurrence of desaturation (SpO2<95%) were recorded by a research assistant during the intubation procedure. The anesthesiologist staff routinely takes responsibility over anesthesia residents and nurse anesthetists for difficult BMV cases and for the second failed intubation attempt.
Adjuvant tools required if first intubation attempt failed: If the first intubation attempt was unsuccessful, several steps using various adjuvant tools were followed as detailed below.
Step 1: Apply the BURP (backward, upward, right, pressure) maneuver or endotracheal tube with a stylet if not yet applied.
Step 2: Change type of laryngoscope blade (from Miller to Macintosh or vice versa) or endotracheal tube size.
Step 3: Change laryngoscopist (nurse anesthetist, anesthesia resident, and anesthesiologist staff).
Step 4: Apply video laryngoscopy or supraglottic airway devices (laryngeal mask airway).
If the intubation by the anesthesiologist staff was not successful for three times (step 3), failed intubation would be declared and step 4 would be considered.
Open airway maneuvers required and the occurrence of adverse events during BMV
Open airway maneuvers were performed during BMV if chest rising could not be visualized or an organized waveform of end-tidal carbon dioxide could not be detected. Open airway maneuvers were performed under the supervision of the anesthesiologist in charge during the induction period and included the application of continuous positive airway pressure (CPAP) ≥ 5 cm H2O with the head-tilt/chin-lift or jaw-thrust maneuver; the use of an oropharyngeal airway (OPA); and the use of two-person ventilation (TPV). If the BMV procedure was unsuccessful or if desaturation (SpO2<95%) or severe desaturation (SpO2<90%) occurred, endotracheal intubation was attempted to secure the airway. There was no time limit for BMV. BMV was performed by following the Difficult Airway Society (DAS) protocol. If BMV was difficult, intubation attempts would be performed as soon as possible. Management of gastric distension depended on the discretion of the anesthesiologist in charge. All procedures and events were recorded by a research assistant.
Outcome of interest
The primary outcome was difficult laryngoscopy/intubation. Difficult laryngoscopy was defined as a Cormack-Lehane laryngoscopic view grade of 3 or 4 [5]. Difficult intubation was defined as the occurrence of at least two of the following: 1) at least three intubation attempts using a conventional laryngoscope blade by experienced anesthesia personnel (excluding first intubation attempts), either Miller or Macintosh [5]; 2) intubation time (the summation of all attempts from applying the laryngoscope to the endotracheal tube that passed the vocal cords) >300 s [6]; and 3) the occurrence of desaturation (SpO2<95%). Failed intubation was defined as failed intubation by a conventional laryngoscope blade after three attempts by anesthesiologist staff.
The secondary outcome was the grading of BMV performance status. This was modified from Han et al. [12] and defined as follows: grade 0 (easy BMV without requiring an open airway maneuver), grade 1 (easy BMV after applying CPAP), grade 2 (successful BMV after inserting an OPA), grade 3 (successful BMV after applying TPV), and grade 4 (unsuccessful BMV after applying all airway maneuvers). Difficult BMV was defined as a BMV grade of 3 or 4 [12].
Outcome of interest
Potential confounding variables were considered, including various patient factors, such as age, sex, body weight, obesity (>95 percentile weight for age), history of asthma/hyperreactive airway, and history of snoring; surgical factors, including the type of operation (e.g., cardiovascular–thoracic surgery, orthopedic surgery, eye surgery, ear–nose–throat surgery, and abdominal surgery); and anesthetic factors, such as induction of an anesthetic agent (sevoflurane/ intravenous agent), intubation agent (no neuromuscular blocking agent, non-depolarizing muscle relaxant [cisatracurium, vecuronium, and rocuronium], and succinylcholine), and the laryngoscopist (anesthesia resident, nurse anesthetist, and anesthesiologist).
Statistical analysis
Descriptive statistics of all normally distributed variables are presented as frequencies and means with standard deviations, whereas those for non-normally distributed variables are presented as medians with interquartile ranges (IQRs). To compare the continuous variables between groups, the Student’s t-test was performed for normally distributed variables and the Wilcoxon rank-sum test was performed for non-normally distributed variables. The χ2 test or Fisher’s exact test for categorical variables (obesity, history of snoring, history of airway disease, type of operation, use of neuromuscular blocking agent, the laryngoscopist, and BMV difficulty) was used to compare the potential variables with difficult laryngoscopy/intubation. BMV difficulty was determined by cross- tabulation and univariate logistic regression analysis. A directed acyclic graph (DAG) was used to represent the potential causal relationships among the covariates and the outcomes (DAGitty software version 2.3). Potential covariates were then selected for an initial multivariate logistic regression model [13]. Associations with BMV difficulty, as well as potential confounders, are presented as the adjusted odds ratios and 95% CIs for appropriate sets of adjustment variables as indicated by the DAG. The predictive ability of the final logistic regression model was evaluated by calculating the area under the receiver operating characteristic curve (AUC) and was considered statistically significant if the likelihood ratio test P value was <0.05.
Sample size calculation
We estimated that the incidence of BMV difficulty in children was 6.6% based on a previous study [6]. In addition, we assumed that the lowest prevalence of the outcome (difficult laryngoscopy/ intubation) among the unexposed group (non-difficult BMV) would be 10%. We then used a formula for comparing two independent proportions, with a ratio of the unexposed group to the exposed group of 14:1, to detect a risk ratio of at least 3.0. Considering a significance level of 0.05 and a power of 80%, the required sample size for cases of BMV difficulty was determined to be 41, along with 574 cases of non-difficult BMV. The total sample size was then increased to 684 to account for a 10% drop out rate.
The flow diagram for the study is shown in Figure 1. A total of 765 children were recruited after applying the exclusion criteria. Missing data were determined to represent 1.3%; these data points were edited and completed by reviewing the raw data from the anesthetic records and hospital information system. Since the setting of the study was a university hospital and a regional training center, first attempts at intubation were excluded. The incidence of unanticipated difficult laryngoscopy/intubation in our study was 6.4% (49/765).
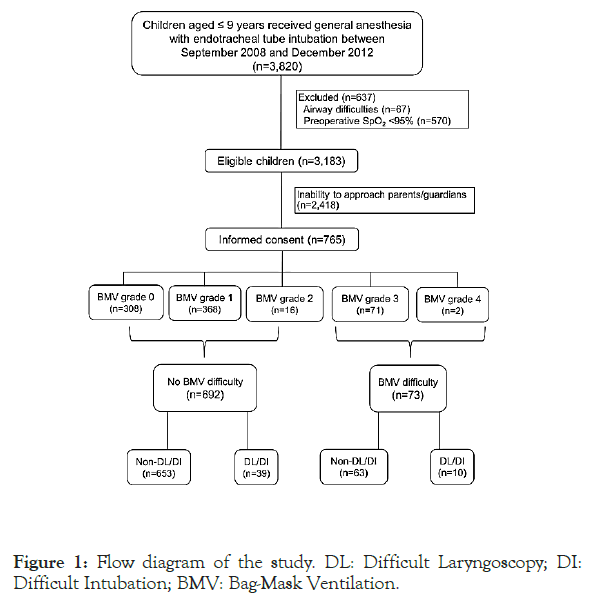
Figure 1. Flow diagram of the study. DL: Difficult Laryngoscopy; DI: Difficult Intubation; BMV: Bag-Mask Ventilation.
The incidence of “cannot ventilate” and/or “cannot intubate” and esophageal intubation in our study was 0%. The distribution of the 49 children with difficult laryngoscopy/intubation is shown as a Venn diagram in Figure 2. A laryngoscopic view grade of 3 or 4 was observed in 47 patients, of which seven experienced desaturation and two had both desaturation and at least three intubation attempts by experienced personnel (four intubation attempts overall). One child (a 9 month-old infant) had a laryngoscopic view grade of 4. In this child, the third and successful intubation attempt was performed by an anesthesiologist with the BURP maneuver, along with a reduction in the endotracheal tube size from 4 mm ID to 3.5 mm ID. All laryngoscopic view grade 3 intubations (46 children) were successful on the third attempt.
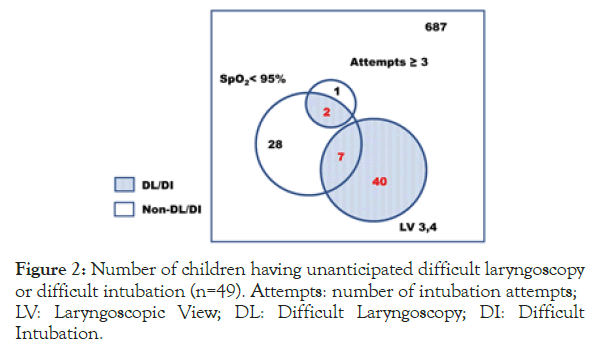
Figure 2. Number of children having unanticipated difficult laryngoscopy or difficult intubation (n=49). Attempts: number of intubation attempts; LV: Laryngoscopic View; DL: Difficult Laryngoscopy; DI: Difficult Intubation.
The distribution of the BMV grade is shown in Table 1. Difficult BMV (grades 3 and 4) was observed in 73 children. The distribution of open airway maneuvers or events during the BMV procedure are shown in Table 2. The most common open airway maneuver was the use of CPAP (54.8%), followed by assistance from a second person (9.3%). Two children had an unsuccessful BMV because of a cleft lip/cleft palate; however, the first intubation attempt, as performed by an anesthesiologist, was successful. BMV was performed before any muscle relaxant was given. A total of 683 of 765 children (89%) received muscle relaxant, of which 70 (10.2%) had a difficult ventilation. Of the 82 who did not receive muscle relaxant, 3 (3.7%) had a difficult intubation (p=0.09). Thus, according to our data, there was no significant association between use of muscle relaxant and BMV difficulty.
| Grading | Criteria | Number (%) |
|---|---|---|
| 0 | Easy bag-mask ventilation without requiring an open airway maneuver | 308 (40.3) |
| 1 | Easy bag-mask ventilation after applying continuous positive airway pressure | 368 (48.1) |
| 2 | Successful bag-mask ventilation after inserting an oropharyngeal airway | 16 (2.1) |
| 3 | Successful bag-mask ventilation after applying two-person ventilation | 71 (9.3) |
| 4 | Unsuccessful bag-mask ventilation after applying all open airway maneuvers | 2 (0.3) |
Table 1: Grading of bag-mask ventilation performance status (n=765).
| Adjunct airway tools and success rate | First attempt (n=765) | Second attempt (n=74) | Third attempt (n=14) | Fourth attempt (n=3) | Fifth attempt (n=1) |
|---|---|---|---|---|---|
| BURP maneuver | 102 (13.3) | 26 (35.1) | 9 (64.3) | 2 (66.7) | 1 (100) |
| Use of a stylet | 333 (43.5) | 34 (46.0) | 10 (71.4) | 1 (33.3) | 1 (100) |
| Change in blade type (Miller, Mcintosh) | 0 | 8 (10.8) | 4 (28.6) | 0 | 0 |
| Change in endotracheal tube size | 0 | 28 (39.4) | 7 (50.0) | 1 (33.3) | 0 |
| Change in laryngoscopist | 0 | 30 (40.5) | 7 (50.0) | 1 (33.3) | 1 (100) |
| Application of video laryngoscopy | 0 | 0 | 0 | 0 | 0 |
| Application of supraglottic airway devices | 0 | 0 | 0 | 0 | 0 |
| Success rate | 700 (91.5) | 62 (83.8) | 12 (85.7) | 2 (66.7) | 1 (100) |
Data are presented as the number (%). BURP: backward, upward, right, pressure.
Table 2: Adjunct airway tools to facilitate intubation.
The median (IQR) intubation time was 24 (15-35) s and the longest intubation time was 300 s, which occurred in two children. The various adjuvant tools/steps that were used to facilitate the additional intubation attempts are shown in Table 3. In the first attempt, the use of a stylet and the BURP maneuver occurred in 43.5% (333/765) and 13.3% (102/765) of patients, respectively. The use of a stylet was mostly applied in all attempts except the fourth. Two infants (a 4 month-old and a 10 month-old) who had difficult intubation (received first three attempts by the nurse anesthetist/ resident) but nondifficult laryngoscopy (a laryngoscopic view grade of 2) were successfully intubated by an anesthesiologist using the BURP maneuver. The use of a supraglottic airway device or video laryngoscope was not required in any cases evaluated in this study.
| Variable | Laryngoscopy/intubation | p value | |
|---|---|---|---|
| Non-difficult (n=716) | Difficult (n=49) | ||
| Age (months) | 34.0 (12.0, 60.0) | 13.0 (7.0, 57.0) | 0.017* |
| <12/12-36/>36 | 172/192/352 | 19/15/15 | 0.023† |
| Sex (M/F) | 387/329 | 30/19 | 0.414 |
| Body weight (kg) | 13.0 (8.5, 17.5) | 9.0 (6.8, 13.8) | 0.016* |
| Obesity (Y/N) | 34/682 | 2/47 | 1.000 |
| History of snoring (Y/N) | 148/568 | 10/39 | 1.000 |
| History of asthma/hyperreactive airway (Y/N) | 82/634 | 8/41 | 0.426 |
| Type of surgery (1/2/3/4/5/6)‡ | 93/143/154/113/92/121 | 9/15/9/6/5/5 | 0.348 |
| Induction agent (1/2/3)§ | 156/119/441 | 7/6/36 | 0.248 |
| Intravenous agent (thiopental/propofol) | 400/36 | 31/3 | 0.754 |
| Neuromuscular blocking agent (1/2/3/4)‖ | 75/551/38/51 | 7/32/4/6 | 0.210 |
| First BMV performer and laryngoscopist (1/2/3)¶ | 323/374/19 | 19/27/3 | 0.301 |
| Open airway maneuvers | |||
| Use of continuous positive airway pressure (Y/N) | 393/323 | 26 /23 | 0.920 |
| Use of oropharyngeal airway (Y/N) | 27/689 | 3/46 | 0.432 |
| Two-person ventilation (Y/N) | 63/653 | 8/41 | 0.119 |
| Events | |||
| Unsuccessful BMV | 0/716 | 2/47 | 0.004** |
| Desaturation (% SpO2) (≥95/90-94/<90) | 693/7/16 | 43/2/6 | <0.001†† |
| BMV difficulty (grades 0-2/grades 3 and 4) | 653/63 | 39/10 | 0.019** |
Note: Data are presented as the median (interquartile range) or number. * By Wilcoxon rank-sum test. † By Fisher’s exact test, ‡1: cardiovascular–thoracic, 2: orthopedic, 3: eye, 4: ear–nose–throat, 5: abdomen, 6: others. §1: incremental sevoflurane 2%–8%, 2: single breath sevoflurane, 3: intravenous agent. ‖: None, 2: cisatracurium, 3: amiosteroids, 4: succinylcholine. ¶1: nurse anesthetist, 2: resident, 3: anesthesiologist staff. ** By Fisher’s exact test. †† By chi-square test. BMV: Bag-Mask Ventilation.
Table 3: Comparison of patient characteristics and anesthetic data between children with difficult and nondifficult laryngoscopy/intubation.
Table 4 compares patient characteristics and surgical and anesthetic data between the 714 children who had a nondifficult laryngoscopy/ intubation and the 49 who had a difficult laryngoscopy/intubation. The only significant variables were age and weight. Children who had a difficult laryngoscopy/intubation were significantly younger, at less than 1 year of age (median age: 13.0 v/s 34.0 months), and weighed less (median weight: 9.0 v/s 13.0 kg) compared with children who had a nondifficult laryngoscopy/intubation.
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| Crude odds ratio (95% CI) | p value* | Adjusted odds ratio (95% CI) | p value* | |
| BMV difficulty | 2.66 (1.27, 5.58) | 0.017 | 2.46 (1.09, 5.54) | 0.04 |
| Age group (years) (Ref:>3) | 0.024 | 0.218 | ||
| 1-3 | 1.83 (0.88, 3.83) | 2.00 (0.82, 4.84) | ||
| <1 | 2.59 (1.29, 5.23) | 2.50 (0.88, 7.09) | ||
| Body weight (kg) | 0.96 (0.92, 1.01) | 0.083 | 1.01 (0.95, 1.06) | 0.804 |
| Obesity | 0.85 (0.20, 3.66) | 0.828 | 0.68 (0.13, 3.49) | 0.63 |
| History of snoring | 0.98 (0.48, 2.02) | 0.965 | 1.10 (0.46, 2.66) | 0.829 |
| Type of operation (Ref: CVT) | 0.366 | 0.513 | ||
| Orthopedic | 1.08 (0.46, 2.58) | 1.13 (0.39, 3.23) | ||
| Eye | 0.60 (0.23, 1.58) | 0.85 (0.27, 2.72) | ||
| Ear-nose-throat | 0.55 (0.19, 1.60) | 0.70 (0.18, 2.78) | ||
| Intraabdominal | 0.56 (0.18, 1.74) | 0.51 (0.14, 1.93) | ||
| Other | 0.43 (0.14, 1.32) | 0.44 (0.12, 1.61) | ||
| Use of NMBA (Ref: cisatracurium) | 0.333 | 0.173 | ||
| No | 1.61 (0.69, 3.78) | 1.87 (0.77, 4.55) | ||
| Aminosteriod | 1.82 (0.81, 5.08) | 2.10 (0.52, 8.47) | ||
| Succinylcholine | 2.03 (0.98, 5.55) | 2.51 (0.92, 6.86) | ||
| First laryngoscopist (Ref: nurse anesthetist) | 0.372 | 0.461 | ||
| Resident | 1.23 (0.67, 2.25) | 1.15 (0.60, 2.20) | ||
| Staff | 2.68 (0.73, 9.87) | 2.54 (0.64, 10.06) | ||
*p value by likelihood ratio test. CVT: cardiovascular-thoracic; BMV: Bag-Mask Ventilation; NMBA: Neuromuscular Blocking Agent; DL: Difficult Laryngoscopy; DI: Difficult Intubation; CI: Confidence Interval; Ref: Reference.
Table 4: Use of bag-mask ventilation grading to predict difficult laryngoscopy/intubation (n=765).
Potential causal relationships between the covariates and difficult laryngoscopy/intubation
Figure 3A shows the DAG used to determine the causal and/ or bias pathways between the exposure variables and outcome (difficult laryngoscopy/intubation). After adjusting for potential confounding variables (age, body weight, obesity, history of snoring, type of operation, and first laryngoscopist), the causal pathways between the exposure variables (BMV difficulty) and outcome (laryngoscopy/intubation and use of neuromuscular blocking agents) were left in the DAG (Figure 3B). Even though they were not significant, all potential confounders and exposure variables were selected into the multivariate logistic regression model and included in the final model to reduce bias.
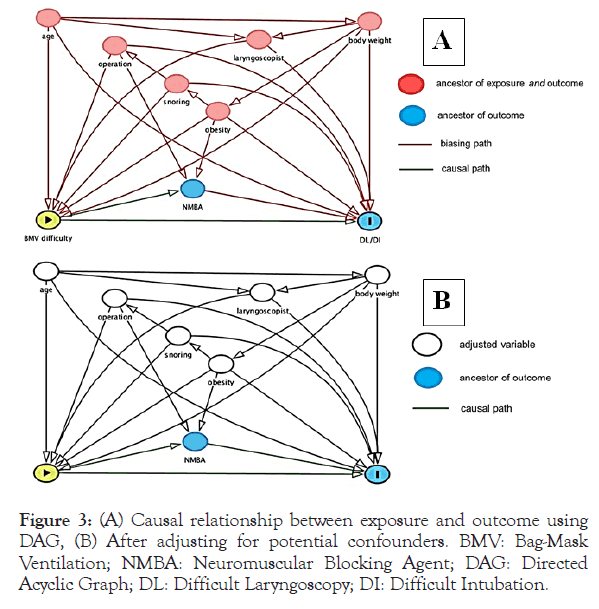
Figure 3. (A) Causal relationship between exposure and outcome using DAG, (B) After adjusting for potential confounders. BMV: Bag-Mask Ventilation; NMBA: Neuromuscular Blocking Agent; DAG: Directed Acyclic Graph; DL: Difficult Laryngoscopy; DI: Difficult Intubation.
Grading of BMV status and association with difficult laryngoscopy/intubation
Table 4 shows the association between BMV difficulty and difficult laryngoscopy/intubation by univariate analysis using a cut-point of BMV grades 3 and 4 (73 children) v/s grades 0-2 (692 children). The association was significant (p=0.02). Table 5 shows the results of the multivariate regression model predicting difficult laryngoscopy/intubation. After adjusting for age, body weight, history of snoring, type of operation, and first laryngoscopist, BMV difficulty was significantly associated with difficult laryngoscopy/intubation (adjusted odds ratios [95% confidence intervals]=2.5 [1.1-5.5]). The sensitivity and specificity were demonstrated to be 0.59 and 0.74, respectively, whereas the AUC was 0.70, as shown in Figure 4.
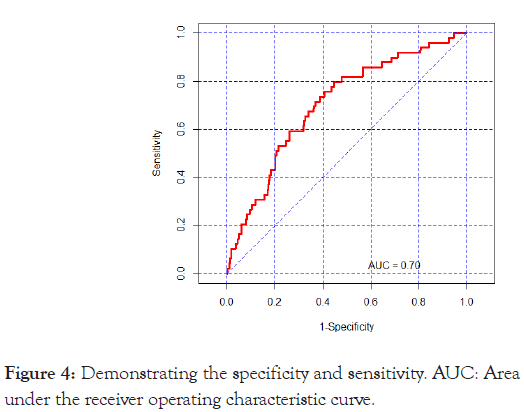
Figure 4. Demonstrating the specificity and sensitivity. AUC: Area under the receiver operating characteristic curve.
| Use of airway adjunct with CPAP | Use of oropharyngeal airway | Two persons required | Unsuccessful ventilation | Desaturation | Number of children | |
|---|---|---|---|---|---|---|
| √ | √ | 16 | ||||
| √ | √ | 43 | ||||
| √ | √ | 16 | ||||
| √ | √ | 14 | ||||
| √ | √ | 2 | ||||
| √ | √ | 6 | ||||
| √ | √ | 6 | ||||
| √ | √ | √ | 8 | |||
| √ | √ | √ | 2 | |||
| Total† | 419 | 30 | 71 | 2 | 31 | 464 |
CPAP=Continuous Positive Airway Pressure. † Number of children having at least one open airway maneuver or event.
Table 5: Airway maneuvers during bag-mask ventilation (N=765).
Criteria for diagnosing difficult laryngoscopy and difficult intubation
The incidence of difficult laryngoscopy (Cormack-Lehane laryngoscopic view grade 3 or 4) in our study was 6.14% (47/765), which was quite higher than those reported in previous studies [1,5]. The incidence of difficult intubation in our study was 0.26% (2/765), which was quite lower than those reported in previous studies [3-4,6].
Reports of difficult laryngoscopy and difficult intubation in pediatric anesthesia varied depending on the criteria used. Some studies reported only difficult laryngoscopy [5], only difficult intubation [3,4], both difficult laryngoscopy and difficult intubation using separate criteria [1], or only difficult intubation using the combined criteria of difficult laryngoscopy and difficult intubation [6]. We used separate criteria to diagnose difficult laryngoscopy and difficult intubation, but we combined both incidence of difficult laryngoscopy and difficult intubation.
Koh et al. [14] published modified Cormack-Lehane grading scores in an adult Asian population and found that a laryngoscopic view grade of 2B (only the arytenoids and epiglottis were able to be seen) was associated with a significantly higher incidence of difficult intubation (65% v/s 13.4%) compared with a grade of 2A (partial view of the vocal cords). In our study, we encountered two infants with laryngoscopic view grade of 2B, which caused difficult intubation and required four intubation attempts. Since laryngoscopic view grades of 2A and 2B may be difficult to assess in pediatric cases, we used laryngoscopic view grade of 3 or 4 to define difficult laryngoscopy, as this is considered to be the standard criteria [5,15].
For difficult intubation criteria, we used at least two criteria comprising the combination of at least three intubation attempts by experienced anesthesia personnel, intubation time more than 300 seconds, and the presence of desaturation (SpO2<95%). For the intubation time, we did not use a total intubation time of >10 minutes like previous study that included a preparation time for changing tube size or changing blade or personnel and BMV period while waiting for the next intubation attempts [16,17]. That extra time might vary depending on how well the equipment or the person are prepared, which might not represent a real time for difficult intubation. Therefore, we used an intubation time of >300 seconds (the summation of all attempts from applying a laryngoscope to the endotracheal tube that passed the vocal cords) according to our previous study [6]. For the criteria of difficult intubation, some studies used three [16,17] or more intubation attempts [18,19], the need for an alternative device to direct laryngoscopy [19], the presence of desaturation, or the combination of at least two criteria to diagnose difficult intubation [6]. In the current study, desaturation alone was not included as a criterion for difficult laryngoscopy/intubation since the occurrence of desaturation during the intubation period may have been the consequence of difficulties during BMV rather than difficult laryngoscopy/intubation.
In this study, the steps taken after the failed first intubation attempt following the induction of general anesthesia were in accordance with the Difficult Airway Society (DAS) guidelines for unanticipated difficult tracheal intubation in a child aged 1-8 years [20], in which adjuvant tools are recommended (Table 3).
According to these guidelines, a direct laryngoscopy should not be attempted more than four times; rather, supraglottic airway devices should be applied [20]. Smereka et al. [21] showed that the first intubation success rate was the same with both the Miller blade (97%) and UESCOPE® video laryngoscope (100%), as well as the median time of intubation (14 s v/s 13 s, respectively), in a normal pediatric airway simulation trial.
As a training center, the majority of the first laryngoscopists (97%) were not anesthesiologist staff but resident/nurse anesthetist who had more than one year of experience; therefore, the first intubation attempt was excluded, and only the second to fourth intubation attempts were counted as the first to third attempts, which were performed by experienced personnel. Usually an anesthesiologist staff will take over on the first or second intubation attempt if a laryngoscopic view of grade 3 or 4 is observed or if the BMV is difficult. However, two children who had difficult intubation (Figure 2) received first three-time intubation attempts by resident/ nurse anesthetist, anesthesiologist staff could successfully intubate in the next attempts in one child and next two attempts in another child. Therefore, a video laryngoscope or a supraglottic airway device had not been used in our study.
This situation was quite risky, even though it was under supervision. An anesthesiologist staff should have taken over intubation procedure sooner (first or second failed intubation attempt) to avoid adverse events. As a result, anesthetists’ non-technical skill program training to improve communication skill and promote situation awareness was implemented in our institute since 2016.
Grading of BMV difficulty and association with difficult laryngoscopy/intubation
We modified the grading of BMV difficulty in children to grades 0 to 4, which are the criteria used for adults [12]. While our grading of BMV difficulty in children was similar to that in adults, we classified CPAP as grade 1 since the incidence of desaturation was the lowest during open airway with CPAP compared with other maneuvers (Table 2).
The guidelines for the management of difficult mask ventilation, according to the Association of Pediatric Anesthetists of Great Britain and Ireland [22] and the DAS guidelines for children aged 1-8 years [20], suggest applying CPAP with 100% oxygen and increasing the depth of anesthesia. These procedures can increase the rate of successful mask ventilation if partial laryngospasm is suspected [20,22].
According to our protocol, if the BMV procedure was considered difficult, propofol was applied to deepen the anesthesia, with succinylcholine considered in the next step to facilitate the procedure as well as break through any potential laryngospasm. Step B of the DAS guidelines for difficult mask ventilation [20] suggests the use of a muscle relaxant to facilitate intubation if the procedure is not successful. This complication was encountered in two cases in our study. In these cases, intubation was performed immediately and successfully by an anesthesiologist on the first and second attempts, respectively, without the use of a supraglottic airway device (step C). However, we did not record gastric decompression in gastric distension cases during the management of the airway, which is an intervention dependent on the discretion of the anesthesiologist staff. Even though desaturation was highly associated with difficult laryngoscopy/intubation (p<0.001 in Table 4), it was not included in our grading criteria for difficult BMV since desaturation was one of the difficult intubation criteria. Collectively, our BMV difficulty criteria were found to be significantly associated with difficult laryngoscopy/intubation (p=0.02 in Table 4).
DAG to reduce potential confounders in the relationship between BMV difficulty and difficult laryngoscopy/ intubation
Because some risk factors may be associated with both BMV difficulty and difficult laryngoscopy/intubation, we used the DAG method to convert any biased pathways (Figure 3A) to unbiased pathways (Figure 3B) by including relevant risk factors (potential confounders) into the final model [13,23]. According to our results, none of the potential risk factors (age, body weight, obesity, history of snoring, type of operation, and first laryngoscopist) were associated with difficult laryngoscopy/intubation in the children studied.
According to Table 5, after adjusting for age, body weight, history of snoring, type of operation, use of a neuromuscular blocking agent, and the first laryngoscopist, we found that BMV difficulty was significantly associated with difficult laryngoscopy/intubation with a modest AUC (0.7). In addition, BMV difficulty had a modest specificity (74%) but low sensitivity (59%). Certain airway assessment results in children have been reported to be associated with difficult laryngoscopy, including a high frontal plane to chin distance, a high frontal plane to chin distance/weight ratio, the high grade of modified Mallampati test, and the upper-lip-bite test [24,25]. However, the assessment of these factors may not be possible in some situations, particularly those concerning uncooperative or frightened children. Apart from having a history of a difficult airway or using the general appearance of the child to screen cases of suspected difficult laryngoscopy/intubation, our results suggest that if children require TPV during BMV, airway equipment tools should be made available and anesthesia personnel should be prepared to manage unanticipated difficult airway should it occur. We believe our BMV difficulty criteria for predicting difficult laryngoscopy/intubation is useful because both events are known to occur in young infants (age<1 year) [6] and those with obesity and/or obstructive sleep apnea [7,26], even though age, obesity, and history of snoring were not significant factors in our study. Moreover, if CPAP or OPA could be applied successfully during BMV, the overall number of cases representing BMV difficulty, as well as difficult intubation, may diminish.
Strengths and limitations
The strengths of this study included that i) the study had a prospective cohort study design to ensure that the exposure (open airway maneuvers/events occurring during BMV) preceded the outcome (unanticipated difficult laryngoscopy/intubation), providing a higher incidence of difficult laryngoscopy/intubation compared with a retrospective study design [27]; ii) DAG was used to reduce the bias; iii) a large sample size with a low rate of missing data was used. However, there were some limitations to the current study. First, we could not control for the use of the same induction anesthetic agent and/or neuromuscular blocking agent for all patients, or certain steps that aided the intubation process, since it was an observational study. Second, because the study was conducted in the training center, the incidence of difficult laryngoscopy and difficult intubation in our study might be higher than non-training center even though the first intubation attempts were excluded. Third, the generalizability of the study may be limited since the study was conducted in a single university hospital.
In this study, the grading of BMV difficulty was well characterized, and our BMV difficulty criteria significantly predicted the risk for unanticipated difficult laryngoscopy/intubation. Collectively, our findings indicate that, when encountered with the requirement of a TPV procedure during the induction of anesthesia in pediatric cases, physicians should have appropriate tools available and prepare personnel to manage the occurrence of unanticipated difficult laryngoscopy or difficult intubation.
The authors would like to thank Glenn Shingledecker of Songklanagarind Hospital for proofreading the final manuscript and Enago (www.enago.jp) for the English language review. We would like to thank Dr. Teresa Valois-Gomez for her advice in the manuscript.
None to report.
This work was funded by the Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand.
Citation: Oofuvong M, Sangkaew T, Nuanjun K, McNeil EB (2020) Grading of Bag-Mask Ventilation Difficulty and Association with Unanticipated Difficult Laryngoscopy/Intubation in Children at a Training Center University Hospital: A Prospective Cohort Study. J Anesth Clin Res.11:937. DOI: 10.35248/2155-6148.20.11.937.
Received: 07-Feb-2020 Accepted: 21-Feb-2020 Published: 28-Feb-2020 , DOI: 10.35248/2155-6148.20.11.937
Copyright: © 2020 Oofuvong M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.