Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2022)Volume 7, Issue 3
Kawasaki disease (KD) is defined as a multi-system, medium-sized vessel vacuities that can lead to myocardial ischemia, infarction, and death. Knowledge of this syndrome’s presentation and pathophysiology is evolving as more cases are reported. This case identifies a two-year-old African American female that was diagnosed with KD and a preceding Group A Streptococcal (GAS) infection. KD may manifest after a variety of infectious etiologies and can present in a manner similar to Scarlet Fever or Multisystem Inflammatory Syndrome in Children (MIS-C). Streptococcal pharyngitis is rare in children under three years of age, but the preceding infection in this patient was suggested by associated symptoms and an elevated antistreptolysin O titer upon hospital admission. We document this case to contribute to understanding of infectious etiologies of KD and the importance of early diagnosis of GAS infections and KD and the early use of penicillin and intravenous immunoglobulin with high-dose acetylsalicylic acid.
Group A streptococcal infection; Kawasaki disease; Pediatrics; Multisystem inflammatory syndrome
Kawasaki Disease (KD) is a multi-system, medium-sized vessel vasculitis commonly seen in males under the age of five. The disease is most prevalent in children of Asian descent, with the highest incidence in Japan. KD is currently the main cause of acquired heart disease in children [1].
The cause of KD is unknown, but there is speculation that an infectious etiology potentiates an immune reaction. Studies have suggested that triggers for KD include Group A Streptococcus (GAS), Staph aureus, Yersinia Pseudotuberculosis, Epstein-Barr virus, human adenovirus, and Candida spp [2]. For GAS, the SpesC exotoxin has been shown to activate T-cells possessing the Vβ2 receptor [3]. GAS is the most common cause of bacterial pharyngitis in children five years and older.
Diagnosis of classic KD is based on the presence of a fever lasting ≥ five days and ≥ four of the following: [4]
• Bilateral bulbar conjunctivitis
• Changes in oral mucosa
• Changes in distal extremities
• Polymorphous rash
• Cervical lymphadenopathy in ≥ 1 node ≥ 1.5 cm
The Kawasaki Disease Scoring System (Table 1) is another diagnostic tool used by physicians to determine the presence of KD (Table 1) [5].
| Major clinical criteria | Points | Comments | |
|---|---|---|---|
| Fever duration | • >4 days | 1 | |
| • ≥ 5 days | 3 | ||
| Conjunctivitis | • If present | 2 | |
| Mucous Membranes | • Strawberry tongue or red internal mucosa | 1 | |
| • Bright red lips | 2 | ||
| • Red and fissured lips | 3 | ||
| Lymph Nodes | • One node 1.5-3 cm in size) | 1 | |
| Rash | • Any rash | 1 | |
| • Perineal | 2 | ||
| • Perineal desquamating | 3 | ||
| Hands/Feet | • Erythema | 2 | |
| • Swelling | 3 | ||
| • Desquamation | 4 | ||
| Lab values | • ESR ≥ 80 or CRP ≥ 2.5 | 1 | |
| • Albumin<2.5 | 1 | ||
| • Platelets>500K | 1 | ||
| Age | • <6 months | 2 | |
| • 6-12 months | 1 | ||
| • >6 years | 1 | ||
| Clinical sequela | • Hydrops of the gallbladder | 5 | |
| Total: | If total is ≥ 9, diagnosis is consistent with Kawasaki Disease and patient should be managed accordingly | ||
Table 1: Kawasaki disease scoring system.
Treatment of KD includes an intravenous immunoglobulin (IVIG) infusion and administration of high-dose acetylsalicylic acid (ASA) followed by daily low-dose ASA at discharge [6]. The most feared complications of KD are coronary artery abnormalities (CAAs), myocardial ischemia, infarction, and death. CAAs are often detected on echocardiography and are classified by a calculated Z-score, which is the coronary diameter adjusted for body surface area. Patients who receive IVIG treatment within 10 days of illness onset are less likely to suffer from CAAs [7].
A two-year-old African American female with no significant medical history and an appropriate vaccination record presented to the Emergency Department (ED) with the primary complaint of a productive cough and rhinorrhea for the last week. The patient was afebrile at presentation with a cough noted on physical examination. She was diagnosed with an upper respiratory infection and given prednisolone and cetirizine at discharge. This will be considered day 1 of presentation.
Three weeks later, on day 22, the patient’s mother called their pediatrician regarding her daughter’s fever of 102°F the night before. She reported that the fever had been on and off for six weeks and that the patient had a diffuse maculopapular rash on her chest, postauricular, and diaper areas. The patient’s mother denied any exposure to someone exposed to, or confirmed to have, Coronavirus Disease 2019 (COVID-19). The patient was taken to an urgent care where she was clinically diagnosed with streptococcal pharyngitis and given a prescription for penicillin VK.
On day 23, the patient returned to the ED because of a persistent temperature of 103°F. On examination, the temperature was 100.3°F with a pulse of 137 b pm, pharyngeal and tonsillar erythema, and extremity edema. The patient was discharged with prescriptions for acetaminophen, dexamethasone, and ibuprofen.
Within a week, on day 27, the mother called their pediatrician again stating that the rash had cleared up, but the patient was fussier with a decreased appetite. The patient refused to stand or allow anyone to touch her. An appointment was scheduled at the office for the following day.
At the office visit on day 28, the patient had a temperature of 100.3°F and a pulse of 126 bpm. The patient was described as thin, inactive, and lethargic with bright red lips and tongue. Physical examination noted bilateral cervical lymphadenopathy, 2+ tonsillar edema, mild edema of the fingers, and desquamation of the inguinal area. At this point the patient tested negative for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) antibodies. The preliminary diagnoses were lower extremity joint pain, fever, and dehydration and the patient was referred for hospital admission.
Upon arrival to the Pediatric Hospital Unit, the patient received a single dose of dexamethasone. She was soon transferred to the Pediatric Intensive Care Unit because of a pulse of 132 bpm, dehydration, and a diagnosis of KD. Points were awarded on the Kawasaki Disease Scoring System as shown in Table 2. The physical examination characteristics for which points were awarded can be seen in Figure 1. An urgent echocardiogram was ordered as well as ASA and an IVIG infusion (Table 2 and Figure 1).
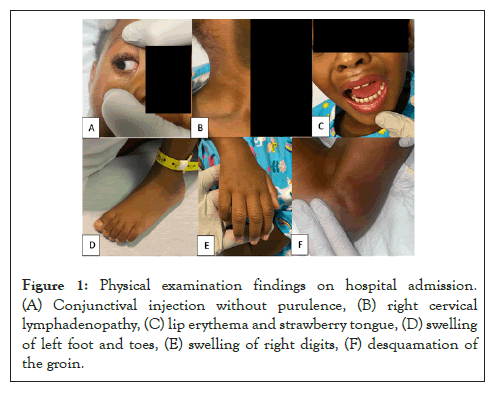
Figure 1: Physical examination findings on hospital admission. (A) Conjunctival injection without purulence, (B) right cervical lymphadenopathy, (C) lip erythema and strawberry tongue, (D) swelling of left foot and toes, (E) swelling of right digits, (F) desquamation of the groin.
| Major clinical criteria | Points | Comments | |
|---|---|---|---|
| Fever duration | • >4 days | 1 | Consecutive days |
| • ≥ 5 days | 3 | ||
| Conjunctivitis | • If present | 2 | Bilateral, non-purulent |
| Mucous Membranes | • Strawberry tongue or red internal mucosa | 1 | Exudates tend against Kawasaki Disease, but not as strongly as red and fissured lips rule it in |
| • Bright red lips | 2 | ||
| • Red and fissured lips | 3 | ||
| Lymph Nodes | • One node 1.5-3 cm in size) | 1 | Least important |
| Rash | • Any rash | 1 | |
| • Perineal | 2 | ||
| • Perineal desquamating | 3 | ||
| Hands/Feet | • Erythema | 2 | |
| • Swelling | 3 | ||
| • Desquamation | 4 | ||
| Lab values | • ESR ≥ 80 or CRP ≥ 2.5 | 1 | Consider giving 2 points if >650? |
| • Albumin<2.5 | 1 | ||
| • Platelets>500K | 1 | ||
| Age | • <6 months | 2 | |
| • 6-12 months | 1 | ||
| • >6 years | 1 | ? vs. >8 years | |
| Clinical sequela | • Hydrops of the gallbladder | 5 | ? vs. 7 points |
| Total: 19 | If total is ≥ 9, diagnosis is consistent with Kawasaki Disease and patient should be managed accordingly | ||
Table 2: Patient’s scoring on the Kawasaki Disease scoring system.
An abdominal ultrasound was done the morning of day 29 showing no ascites and an unremarkable liver, spleen, and gallbladder. The Transthoracic Echocardiogram (TTE) showed dilations of the Left Anterior Descending Artery (LAD) and Right Coronary Artery (RCA) and a normal sized Left Main Coronary Artery (LMCA) (Figure 2). Normal biventricular systolic function was noted with no sign of pericardial occlusion and an ejection fraction of 60%. The calculated Z-scores were -0.93 for the LMCA, 7.9 for the LAD, and 9.26 for the RCA [8]. The values for the LAD and RCA suggest coronary artery disease.
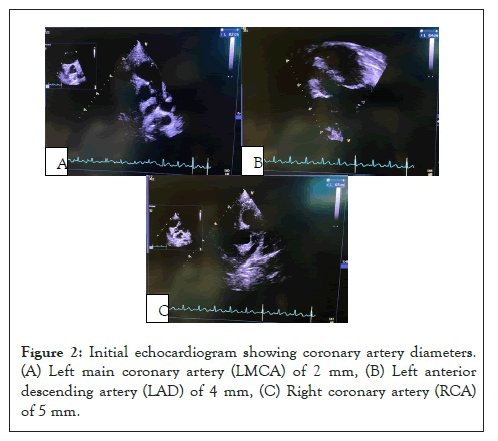
Figure 2: Initial echocardiogram showing coronary artery diameters. (A) Left main coronary artery (LMCA) of 2 mm, (B) Left anterior descending artery (LAD) of 4 mm, (C) Right coronary artery (RCA) of 5 mm.
On day 30, full range of motion of the extremities had returned and the patient was afebrile and stable. Resolution of the conjunctive injection and mucosal erythema can be seen in Figure 3.
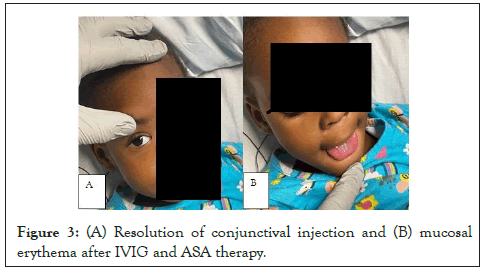
Figure 3: (A) Resolution of conjunctival injection and (B) mucosal erythema after IVIG and ASA therapy.
Figure 3 After three days of receiving the IVIG infusion and high dose ASA regimen, the patient was discharged home with the primary diagnosis of Kawasaki Disease following a GAS infection. This marked day 31 since the initial presentation to the ED. At her outpatient cardiology follow-up two weeks later, a repeat TTE showed coronary artery diameters within normal limits as well as normal cardiac function.
KD is diagnosed using a points system based on symptomatic presentation for which a score of 9 or greater is indicative of KD. This patient scored a 19, reinforcing the diagnosis of KD. Her laboratory values that suggest an active immune response include an ESR ≥ 80 mm/hour (NR 0-20 mm/hour) or CRP ≥ 2.5 mg/ dL (NR 0.0-0.6 mg/dL), Albumin<2.5 g/dL (NR 3.1-4.8 g/dL), Platelets>500 x 103/microL (NR 141-359 x 103/microL).
After reviewing published KD cases, this case is one of few cases to suggest GAS pharyngitis triggering KD. A similar case published in Archives of Disease in Childhood highlights a case of streptococcal pharyngitis preceding KD in a six-year-old boy [9]. What makes this case unique is the patient herself as she is not representative of the usual patient population to suffer from KD. KD is 10 to 30 times more common in Northeast Asian countries than in the United States [10]. KD also occurs more often in males than in females, yet this case is in a female African American [11]. Additionally, GAS is typically seen in children over the age of five, making this patient relatively young for this type of infection [12]. This highlights the significance of GAS infection as the potential trigger for this patient’s KD.
Future studies should be aimed at understanding how KD can be prevented after diagnosis of streptococcal pharyngitis, like prevention of its progression to rheumatic fever. Once the patient’s infection had progressed to KD, early diagnosis would have led to earlier treatment and is pertinent in the prevention of cardiac complications. The rareness of KD following GAS and the uncommon patient presentation may be why there were so many encounters before this patient was diagnosed with KD. It is also important to note that there is hesitation to treat pediatric patients with high-dose ASA because of the risk of inducing Reye’s syndrome [13]. A definite diagnosis of KD is one of few occasions for which the benefits outweigh the risks.
During the COVID-19 pandemic, Multisystem Inflammatory Syndrome in Children (MIS-C) is the primary differential diagnosis for KD, as both conditions present with a skin rash, lymphadenopathy, strawberry tongue, and elevation of inflammatory biomarkers. MIS-C is most commonly in children ages 5 to 11 years old and may present with systolic dysfunction in the left ventricle and abdominal symptoms [14-16]. The patient in this case lacked these additional symptoms and was also negative for SARS-CoV-2 antibodies. We can be confident KD was her primary diagnosis because she met all the diagnostic criteria for KD and effectively responded to treatment with IVIG and ASA.
KD affects 9-20 per 100,000 children under five-years-old and is the leading cause of acquired heart disease in the United States. Although the current understanding of the disease's pathophysiology is incomplete, it is hopeful that the understanding will improve with additional reports and research on the subject. The potential limitations of this study were the subjectivity of the Kawasaki Disease Scoring System and the absence of confirmatory streptococcal pharyngitis testing by rapid antigen test or bacterial culture. This patient was not a member of the usual gender, age, or ethnic group most likely to suffer from KD. For this reason, an abnormal patient presentation should not exclude KD from the differential diagnosis.
This case exemplifies why it is crucial to consider diseases outside of their normal patient profile to ensure efficient and successful treatment. Given that we are still learning what conditions may predispose a patient to KD, an increased index of suspicion is critical for rapid recognition and diagnosis. It is important to attempt to differentiate KD from MIS-C as each disease has serious complications. If KD goes untreated, the patient may suffer from coronary artery disease, myocardial infarction, or death.
Katherine Bohn conducted substantial background research, drafted a significant portion of the article, contributed to article layout and prepared the article for publication. Madison Capotosti also conducted substantial background research, drafted a portion of the article, and revised it critically for important intellectual content. Hanna Sahhar gave final approval of the version of the article to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Cross ref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Sahhar HS, Bohn K, Capotosti M (2022) Group A Streptococcal Infection Potentially Triggering Kawasaki Disease in a Two-Year-Old African American Female. Clin Pediatr. 7:210.
Received: 02-May-2022, Manuscript No. CPOA-22-16568; Editor assigned: 04-May-2022, Pre QC No. CPOA-22-16568 (PQ); Reviewed: 19-May-2022, QC No. CPOA-22-16568; Revised: 23-May-2022, Manuscript No. CPOA-22-16568 (R); Published: 02-Jun-2022 , DOI: DOI: 10.35248/2572-0775.22.7.210
Copyright: © 2022 Sahhar HS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.