Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2024)Volume 14, Issue 2
Background: The aim of this pilot study is to explore the feasibility, acceptability and effectiveness of group Metacognitive Therapy (g-MCT) as a treatment for individuals primarily diagnosed with Generalized Anxiety Disorder (GAD) who are on sick leave or at risk. Given the high comorbidity between GAD and depression and the transdiagnostic nature of Metacognitive Therapy (MCT), the study will also investigate changes in depressive symptoms.
Methods: The study cohort consists of patients referred to the "Poliklinikk psykisk Helse og Arbeid" (PHA), an outpatient clinic at Diakonhjemmet Hospital in Oslo, Norway. Feasibility was assessed based on treatment completion rates, dropout rates and the number of potential candidates for this group treatment. Treatment effectiveness was measured using self-report questionnaires that assessed anxiety, depression, metacognitive beliefs, and work-related self-efficacy.
Results: 27 patients (71%) met the eligibility criteria and started treatment. Only one patient (3.7%) dropped out, resulting in 26 patients completing g-MCT. These 26 patients attended an average of 9.3 sessions. The two therapists spent an average of 3.1 hours each per patient on the therapy, which is less than would be required for an individual MCT. Using the Jacobson-Truax method for clinically significant change, 95.2% of patients were classified as either recovered (57.1%) or improved (38.1%) from their GAD post-treatment, and 47.6% achieved recovery from their depressive symptoms post-treatment.
Conclusion: The findings suggest that g-MCT is a feasible, acceptable, and effective treatment for GAD.
Generalized anxiety disorder; Group metacognitive therapy; Metacognition; Preliminary effectiveness; Depression; Cognitive behavioral therapy
Generalized Anxiety Disorder (GAD) is a common disorder characterized by excessive, uncontrollable worry and physical symptoms such as sweating, hot flashes, tremors, and more [1]. found that 51% of GAD patients reported that their symptoms interfered with daily life [2]. GAD often co-occurs with major depression and an increased risk of self-harm [3], so effective treatment is required. Cognitive Behavioral Therapy (CBT) is the best underpinned psychotherapeutic approach for GAD [4], demonstrated the effectiveness of group CBT (g-CBT) [5], which achieved significant symptom reduction compared to a waiting list group, even after a follow-up period of 2 years [6], found a 70% success rate in the reduction of GAD-specific symptoms with CBT. However, points out that more research is needed to accurately assess the effectiveness of CBT for anxiety disorders [7]. A recent meta-study [8], found only a medium to large effect size (g=0.76) of empirically supported psychotherapeutic interventions for GAD, indicating the need for alternative treatments.
When comparing the effectiveness of Metacognitive Therapy (MCT) and CBT for GAD, found that both therapies resulted in a significant reduction in GAD-related worry compared to the waitlist using the Penn State Worry Questionnaire (PSWQ) [9]. MCT achieved better results, with 65% of the MCT group recovering after treatment compared to 38% in the CBT group. This discrepancy was also found at 2-year follow-up [10], also compared MCT with Applied Relaxation (AR) in GAD patients and found that MCT was more effective than Augmented Reality (AR) in reducing GAD symptoms (n=20, 10 in MCT and 10 in AR). Sessions lasted 45-60 minutes weekly for 8-12 weeks. This study also used the Jacobson-Truax method for clinically significant change [11], and showed that patients receiving MCT had an 80% recovery rate compared to 10% in the AR group [10]. These figures remained unchanged after a 12-month follow-up. The large effect size within the group (d=3.41) combined with a high recovery rate suggests that MCT is an effective treatment for GAD.
Few studies have examined the feasibility and efficacy of group-based MCT (g-MCT) for GAD, although one study found that g-MCT was associated with significant reductions in rumination, anxiety, depression, dysfunctional metacognitive beliefs and maladaptive coping strategies in GAD patients, with a 78.3% recovery rate at three months [12]. This study was an open-label study (n=23) using the PSWQ, Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) questionnaires to assess changes in symptoms during the 10-week treatment. To assess feasibility, the study evaluated the number of patients who discontinued treatment, who were unable to attend pre-scheduled appointments, and the number of patients who declined g-MCT in favor of individual MCT [12]. The results showed that g-MCT is indeed an acceptable treatment for GAD, with recovery rates and effect sizes indicating that g-MCT could be just as effective as individual MCT and CBT [12]. The effectiveness of g-MCT on GAD [12], supports the results of a study by [13], one of the first known studies on g-MCT for GAD [13]. Good outcomes in terms of clinical significance were also found (d=1.23 on State-Trait Anxiety Inventory (STAI-T) with 47 considered recovered, and d=1.86 on PSWQ, with 71 considered recovered) [13]. However, the dropout rate was reported to be higher with g-MCT than with individual MCT, and accordingly, the study tentatively concluded that g-MCT was considered effective when delivered in a setting with heterogeneous clinical practice [13].
Patients with common mental illnesses often struggle with participation in working life, and how they rate their work-related self-efficacy is strongly related to their own perceptions and beliefs about their own problems [14]. The Return to Work- Self Efficacy (RTW-SE) questionnaire has been shown to be a significant predictor of return to work [15]. A higher score could therefore increase the likelihood of patients returning to work and prevent them from taking sick leave in the first place, as their work-related self-efficacy increases. The questionnaire has been shown to be useful for both research and clinical practice, as the scale predicts full return to work [16].
Together, these studies suggest that g-MCT could be as effective as individual MCT in the treatment of GAD. Further research is needed to establish a more comprehensive evidence base for this approach, particularly across different patient groups, in order to generalize treatment implementation. By assessing patients who are on sick leave or at risk of being on sick leave, focusing on work becomes an important goal of treatment.
The aim of the current study is to assess whether g-MCT is a feasible and acceptable treatment approach for patients with GAD, as well as to assess the preliminary effectiveness of g-MCT on GAD symptoms, metacognitions and work-related self-efficacy. The following research questions was assessed:
• What is the feasibility and acceptability of g-MCT for GAD in terms of recruitment, retention/engagement and drop-out rate?
• What is the preliminary effectiveness of g-MCT on anxiety and depression for patients with GAD?
• What is the preliminary effectiveness of g-MCT on metacognitions and work-related self-efficacy for patients with GAD?
Participants
The data was collected as part of a quasi-experimental pre-post study conducted from 2021 to 2023. The participants in the study were individuals who are diagnosed with GAD who participated in metacognitive group therapy and work focus at the outpatient mental health clinic «Poliklinikk psykisk helse og arbeid» (Polyclinic mental health and work) at Diakonhjemmet Hospital in Oslo, Norway.
A total of 26 patients were included in this study. Further characteristics of the sample can be found in Table 1. Inclusion criteria for the study was to meet the requirements for GAD in International Classification of Disease-Tenth Revision (ICD-10) as a primary diagnosis and a symptom score of 8 or more on the GAD-7 before treatment. The diagnosis of GAD was made after completion of an individual preliminary clinical interview with a psychologist using the Mini-International Neuropsychiatric Interview (M.I.N.I) [17], combined with an assessment of the patient's medical history and current symptoms. Additional criteria included proficiency in Norwegian, expectation of functioning well in a group, and excessive worry as their main challenge. Patients were required to complete several self-report questionnaires, which were selected based on our research questions: Measures of Anxiety (GAD-7), Depression (PHQ-9), Metacognition (MCQ-30), and Work-Related Self-Efficacy (RTW-SE). Patients completed the GAD-7 and PHQ-9 self-report questionnaires before each treatment session and before and after treatment. Patients also completed the MCQ-30 and the RTW-SE before and after treatment.
Four patients had comorbid depression as a secondary diagnosis. Depression is one of the most common psychiatric disorders [18], and is highly comorbid with GAD. Due to this comorbidity, it is relevant to assess possible changes in the PHQ-9 questionnaire, as MCT is a transdiagnostic model and has implications for both GAD and depression outcomes Figure 1 [19].
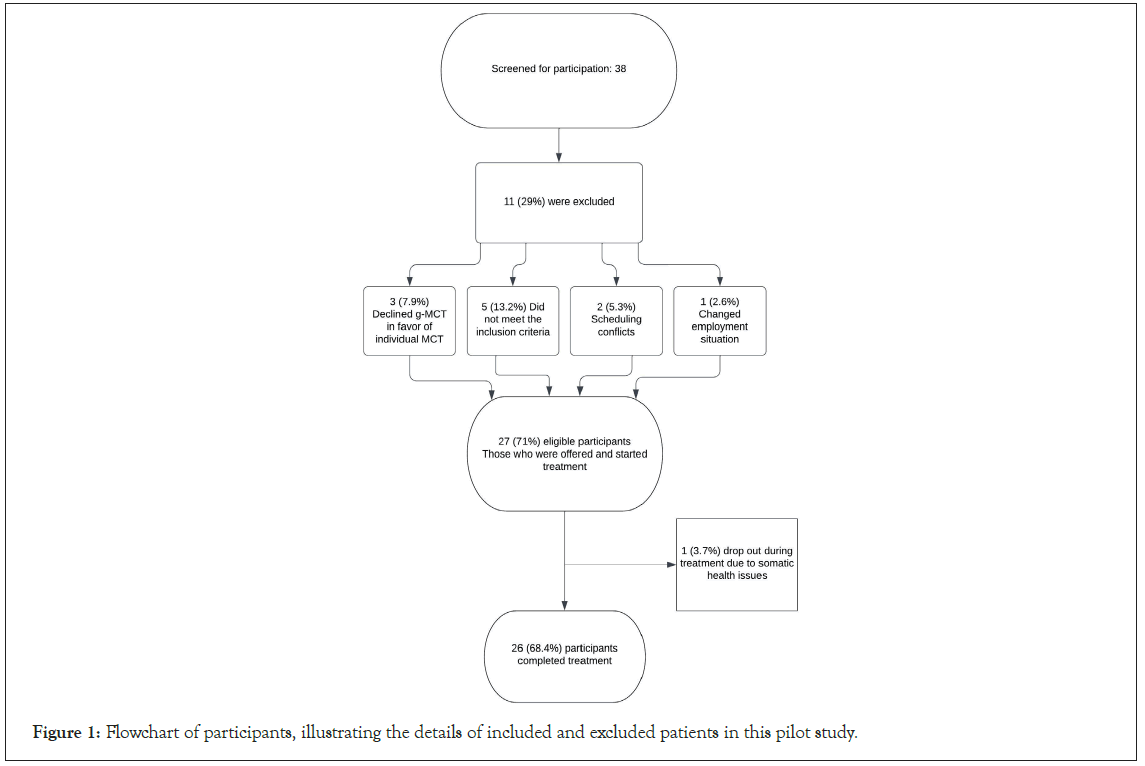
Figure 1: Flowchart of participants, illustrating the details of included and excluded patients in this pilot study.
Treatment
The treatment is based on a manualized treatment protocol with a clear structure. The manual opens up for an active collaboration between the patient and the therapist, focusing mainly on how the problems manifest themselves to the patient. In the work-focused part, the patients acquire new strategies to cope with psychological problems at work, at school and in everyday life. For those on sick leave, the possibility of a gradual return to work will be an important topic. A common element of treatment is therefore work focus, and consequently work-related worries become an important topic in the group treatment.
Metacognitive Therapy (MCT) suggests that the actual content of thoughts is not what creates a psychological disorder, because most people have negative thoughts. Instead, MCT suggests that it is the patient's responses to his/her own thoughts which constitutes the source of mental suffering [20]. In MCT, the set of pathological responses driving psychological disorders is called the Cognitive Attentional Syndrome (CAS). The CAS includes perseverative thinking patterns like worry and rumination, as well as threat monitoring and other maladaptive coping strategies [20].
The metacognitive model of GAD is derived from the Self- Regulatory Executive Function (S-REF) model, and centers around the patients’ metacognitions (their beliefs about their own worries, rumination and threat monitoring) [20,21]. Negative metacognitive beliefs are cognitions related to worrying being out of the patient’s control, and/or worrying representing danger, e.g., “My worry is uncontrollable” or “Worrying is bad for my heart and might give me a heart attack” [22]. These negative metacognitive beliefs related to worry are especially prominent in GAD according to MCT, as the model states that GAD itself develops because of the activation of a person's negative metacognitive beliefs [20]. It is when the negative meta-beliefs are activated and the patient develops a “type 2 worry” that they are considered having a pathological anxiety pattern, resulting in GAD. A type 2 worry is characterized by the patient worrying about his/her worrying, leading to increased anxiety and an inability to stop his/her train of thoughts [20]. Along with the negative metacognitions patients frequently have positive metacognitions. They are linked to beliefs about the potential benefits of e.g., worrying, “Worrying will keep me prepared.” The patients are thus often locked into a perseverative pattern of worrying as they both see it as an advantage and something that is out of their control [20].
The MCT sessions were held once a week over a period of 10 weeks. There were 10 sessions in total, each lasting two hours, including a 10-minute break. The ideal number of patients was 7+/-2, with two therapists present. In terms of work focus as part of treatment, common experiences of worry or rumination considering work- related situations were exemplified and emphasized if the patients themselves brought it up and would also be thematized by the therapists. An example of this could be activation of the Cognitive Assessment System (CAS) in terms of excessive worrying about e.g. “What if I am never able to return to work?”
In this pilot study, the analyses were based on four groups, with a total of 26 patients participating across all four groups. For research purposes, patient data from all four groups were merged in the analyses as they all received the same treatment from the same two therapists. The g-MCT was conducted in accordance with the GAD treatment plan [20].
Measures
The primary outcome measure Generalized Anxiety Disorder-7 (GAD-7) is a self-report questionnaire that measures the symptoms of GAD using seven items [23]. Patients report on their symptoms over the past two weeks. The total GAD score is calculated by assigning the response categories for each item the values 0 (“not at all”), 1, 2 and 3 (“nearly every day”). There are different ways to define the cut-off values. In this study [24], the cut-off score was set at 8. A score of ≥ 8 indicates a GAD diagnosis. The internal consistency of the GAD-7 is excellent (Cronbach's α =0.92) [23]. The test-retest reliability is also good (r=0.83). The validity in terms of construct, criterion, factorial and procedural validity is also sufficient [23,25]. Other studies have supported the excellent internal consistency of the scale [24]. In this study, the GAD-7 has an alpha value of 0.86.
Secondary outcome measures: The Patient Health Questionnaire-9 (PHQ-9) [26], is part of the Patient Health Questionnaire (PHQ) [27], and consists of nine items that measure symptoms of depression in the past two weeks and are directly related to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnostic criteria. The total PHQ score is calculated by assigning the response categories for each item the values 0 (“not at all”), 1, 2 and 3 (“nearly every day”). Questions 1 and 2 of the scale must be scored as either 2 (“more than half the days”) or 3 (“almost every day”) according to the DSM-IV diagnostic system to indicate depression. In addition, the patient must indicate that they experience a loss of function in daily life [26]. The following cut-off points for the PHQ-9: 5-9=mild symptoms of depression, 10-14=moderate symptoms of depression, 15-19=fairly severe symptoms of depression, 20-27=severe symptoms of depression. In accordance with [26], a cut-off value of 10 was used in this pilot study. Research indicates that the PHQ-9 is a reliable and valid measure of the severity of depression [26,28]. Kroenke [26], state that the scale has an internal consistency between 0.86 and 0.89 and a 48-hour test-retest reliability of 0.84. The high reliability of the PHQ-9 has also been established in various countries and languages [29-31]. In this study, the PHQ-9 has a Cronbach’s alpha value of 0.75, which is acceptable.
The Metacognitive Questionnaire-30 (MCQ-30) is a shorter version of the MCQ-65 [32]. The MCQ-30 maps metacognitive assumptions with a self-report questionnaire containing 30 questions divided into five subscales. The metacognitive assumptions are rated on a four-point scale from 1-4. Higher scores indicate higher levels of maladaptive metacognitive assumptions. Research suggests that the subscales are responsive to metacognitive therapy [10], and the subscales have a Cronbach’s alpha between 0.72 and 0.93 [32]. Furthermore, the factor structure of the items and the construct validity have been confirmed by research [33,34]. In this pilot study, all items were considered together and not the outcomes of the individual subscales. The MCQ-30 had a Cronbach’s alpha value of 0.93 in the current pilot study.
The Return-to-Work Self-Efficacy Questionnaire (RTW-SE) was originally developed by Lagerveld [35]. It was translated from English into Norwegian by an expert panel of clinical psychologists at Diakonhjemmet Hospital and consists of 11 items ranging from 1 (completely disagree) to 6 (completely agree) [16]. It measures people's expectations and confidence for work (self-efficacy) if they were to go to work tomorrow with their current physical and mental health. Research has shown that the psychometric properties of the scale are good that [16], assessed the reliability and validity of the scale. The scale had a Cronbach's alpha of 0.91, indicating excellent internal consistency. Pre-and post-treatment scores on the scale predicted full return to work at either 3,6 or 12 months, indicating predictive validity. In this study, Cronbach's alpha value for this scale was 0.94, which is excellent. Patients were also asked to complete an anonymous evaluation form after the final session, mainly describing their subjective experience of the group-based treatment. This evaluation form served as an exploration of the quality of the project. The evaluation forms were submitted anonymously and neither the forms nor the statements can be linked to individual patients.
Statistical analysis
Feasibility was assessed based on the number of patients who completed the treatment, the number who dropped out, in addition to the number considered as possible candidates for this group treatment, as shown in the flowchart. Paired-samples t-tests were performed to compare patients´ mean scores on GAD-7, PHQ-9, MCQ-30, and RTW-SE pre- and post- treatment [11]. The GAD-7 was the primary outcome measure, and the PHQ-9 was the secondary outcome measure. The threshold value is<8 on the GAD-7 and is based on a Norwegian psychometric study [24]. The post-treatment score had to be below the cut-off point on GAD-7 (8 points) and the PHQ-9 (10 points) and there had to be a reliable 6-point change in score on the PHQ-9 and a 4-point change on the GAD-7 to be considered recovered. Only a 4- and 6-point change (without scoring below the cut-off value) on GAD-7 and PHQ- 9, respectively, represents an improvement. The effect sizes were calculated using Cohen’s d [35]. The guidelines for determining the strength of the effect are as follows: small effect=0.2, medium effect=0.5, large effect=0.8 [36]. There were only a few missing variables (0.10% missing variables in the analysis of research question 2 and 1.22% missing variables in the analysis of research question 3). Missing values were handled by mean imputation.
Each patient was informed and asked to sign a written informed consent in accordance with the Declaration of Helsinki [37], before participation. This study was conducted in accordance with Good Clinical Practice (GCP), including the current version of the Declaration of Helsinki, and Norwegian laws and regulations. The study was approved by the Regional Committees for Medical and Health Research Ethics in Norway (REK) under application number 602141 (Figure 2).
Figure 2: Average score GAD-7, for 4 individual groups every group session with error bars.
In results we discussed about the feasibility and acceptability of g-MCT for GAD in terms of recruitment, retention/engagement and drop-out rate.
As shown in the flowchart in Figure 3, 11 patients were excluded because they ultimately did not meet the inclusion criteria. As shown in the flowchart (Figure 1), 27 patients were offered treatment. All patients, except for one patient who dropped out of the study, attended an average of 9.3 sessions (n=26). On average, the two therapists spent 3.1 hours each per patient on therapy. An overview of the sample characteristics of the patients who completed the g-MCT treatment is shown in Table 1.
| Characteristics | Number | Percentage of sample (%) | |
|---|---|---|---|
| Gender | Male | 9 | 35 |
| Female | 17 | 65 | |
| Age | 20-29 yrs | 9 | 35 |
| 30-39 yrs | 13 | 50 | |
| 40-49 yrs | 3 | 12 | |
| 50-59 yrs | 1 | 4 | |
| Marital status | Single | 6 | 23 |
| Married/cohabiting | 19 | 73 | |
| Separated/divorced | 1 | 4 | |
| Education level | Primary school | 1 | 4 |
| High school | 1 | 4 | |
| University and college 1-4 yrs | 16 | 62 | |
| University and college ≥ 4 yrs | 8 | 31 | |
| Years of suffering | 1-5 yrs | 6 | 20 |
| 6-10 yrs | 4 | 20 | |
| 11-15 yrs | 5 | 25 | |
| 16-20 yrs | 4 | 15 | |
| 21-25 yrs | 1 | 5 | |
| 26-30 yrs | 0 | 0 | |
| 31-35 yrs | 1 | 5 | |
| No answer | 5 | 10 | |
| Sick leave | 0% | 16 | 62 |
| 30% | 1 | 4 | |
| 40% | 1 | 4 | |
| 50% | 4 | 15 | |
| 60% | 1 | 4 | |
| 100% | 2 | 8 | |
| Long time benefit | 1 | 4 | |
| Diagnosis | F41.1 Generalized anxiety disorder | 26 | |
| F32.0 Mild depressive episode | 2 | ||
| F33.0 Recurrent depressive disorder, current episode mild | 2 | ||
| F32.1 Moderate depressive episode | 1 | ||
| F41.2 Mixed anxiety and depressive disorder | 1 | ||
| F1x.7 Residual and late-onset psychotic disorder due to hallucinogens | 1 | ||
Table 1: Sample characteristics of patients who were included in the study (n=26).
The patients filled out an evaluation form post-treatment. The overall feedback was that the treatment had been useful for the patients. The practical assignments were highlighted as particularly important. Table 2, below shows statements from patients about their experiences from the group therapy. The evaluation forms were submitted anonymously and neither the forms nor the statements can be linked to each individual patient (Table 2).
| Did you benefit from the treatment? | “Very useful” |
| “Useful tools” | |
| “Positive impact on my work life” | |
| “Practical assignments were important” | |
| Which experiences were most important throughout the treatment? | “Being in a group is more useful/effective than individual treatment” |
| “To not avoid feelings” | |
| “Anxiety/worry is not dangerous/cannot hurt you or make you go crazy” | |
| “Worrying is controllable” | |
| “More insight” | |
| “More aware of triggers” | |
| “Worry is not useful and can be postponed” | |
| “There are others who also struggle with GAD” | |
| How will you use what you have experienced in the treatment facing upcoming challenges? | “Stick to my new plan” |
| “Not avoid things/situations” | |
| “Postpone worry” | |
| “Accept feelings and thoughts. They can exist without worry” | |
| “Focus on actual problems and not problems that have not happened yet” | |
| What was it like for you to join the group? | “Diversity” |
| “Good therapists” | |
| “Feels safe to share experiences” | |
| “Challenging in the beginning, but more comfortable with time” | |
| “Educational” | |
| “It is nice to be a teamplayer” | |
| How did you experience the therapists? | “Very skilled and professional” |
| “Coordinated” | |
| “Empathetic” | |
| “Challenges us in a safe way” | |
| “Good balance between theory and practice” | |
| What do you think about your own efforts in the treatment? | “Good job” |
| “My effort produced results” | |
| “I felt that I contributed to all tasks in a good way” | |
| “I was engaged in the treatment and did my homework” | |
| “I shared experiences with others” | |
| “Satisfied” | |
| “I am all in” | |
| “I have challenged my thinking style every day” | |
| Are there any topics you missed in the treatment? | “Exposure” |
| “More about social anxiety” | |
| “Research articles” | |
| “Pictures, illustrations” | |
| Do you have any other feedback you would like to share with us? | “Happy I could participate” |
| “Reflections in the last group session was nice” | |
| “Grateful” | |
| “Could have lasted longer than 10 weeks” | |
| “Thank you for this excellent treatment and tools we have learned. The exercises were great” |
Table 2: Feedback from the patients regarding their treatment.
In results we discussed about the preliminary effectiveness of g-MCT on anxiety and depression for patients with GAD.
Results from Table 3, show that there was a significant decrease in anxiety scores (GAD-7) from pre-treatment (M=13.81, SD=3.17) to post-treatment (M=6.66, SD=4.13), t(20)=8.72, p<.001. The mean decrease in GAD-7 scores was 7.15. The effect size was large (d=1.90). There was also a significant decrease in depression PHQ- 9 scores from pre-treatment (M=13.16, SD=4.05) to post-treatment (M= 7.14, SD=4.03), t(20)=5.00, p<.001. The mean decrease in PHQ-9 scores was 6.02. The effect size was large (d=1.09) (Table 3).
| Pre-test | Post-test | 95% CI for Mean Difference | Paired differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | N | SD | t | df | Sig.(two-tailed) | |||
| GAD-7 | 13.81 | 3.17 | 6.66 | 4.13 | 21 | 5.44 | 8.86 | 3.76 | 8.72 | 20 | <.001 |
| PHQ-9 | 13.16 | 4.05 | 7.14 | 4.03 | 21 | 3.50 | 8.53 | 5.52 | 5.00 | 20 | <.001 |
Note: GAD-7: Generalized Anxiety Disorder-7; PHQ-9: Patient Health Questionnaire-9.
Table 3: Paired samples t-test results for GAD-7 and PHQ-9.
Table 4, presents a summary of recovery rates based on the Jacobson- Truax method of clinical significant change. To be considered recovered from GAD patients must have a score below the cut-off value for GAD-7, and there must be a change of 4 or more in the scores. To be considered recovered from depression, patients must score below the cut-off on the PHQ-9 and have a change in scores of 6 or more. In this pilot study, 57% of patients were considered recovered from GAD post-treatment, 38.1% were considered improved and 4.8% were deteriorated. 47.6% were considered recovered from depression, 9.5% were improved and 42.9% were unchanged. Overall, 95.2% of patients were considered either improved or recovered post- treatment.
| Studies conducted (Questionnaires used) |
Cut-off in this study | This study GAD-7 |
This study PHQ-9 |
Haseth et al (2019) PSWQ |
Haseth et al (2019) GAD-7 |
Haseth et al (2019) PHQ-9 |
van der Heiden et al (2013) PSWQ |
van der Heiden et al (2013) STAI-T |
|---|---|---|---|---|---|---|---|---|
| Recovered | 4 or 6 points1 | 57.1% | 47.6% | 65.3% | 87.0% | 52.2% | 71.0% | 47.0% |
| Improved | 4 or 6 points2 | 38.1% | 9.5% | 30.4% | 8.7% | 39.1% | 17% | 35.0% |
| Total | 95.2% | 57.1% | 95.7% | 95.7% | 91.3% | 88.0% | 82.0% | |
| Unchanged | No change3 | 0% | 42.9% | 4.3% | 4.3% | 8.7% | 0% | 0% |
| Deteriorated | Increase in score4 | 4.8% | 0% | 0% | 0% | 0% | 0% | 0% |
Table 4: Summary of recovery rates post-treatment based on the Jacobson-Truax method of clinically significant change.
• Change of 4 (GAD-7) or 6 (PHQ-9) or more and score below cut-off, 8 on GAD-7 and 10 on PHQ-9.
• Change equals 4 (GAD-7) and 6 (PHQ-9) or more, without scoring below the cut-off value.
• No change in scores.
• An increase in scores of 4 or 6.
Figure 2, illustrates the average score on GAD-7 for the whole group from session to session with a maximum score of 13.81 and a minimum score of 6.65. The group is considered recovered. The graph shows that g-MCT is associated with reduction in symptoms from session to session. The error bars represent the variability in patients’ scores (Figure 2).
Figure 3, illustrates the average score on PHQ-9 for the whole group each group session. The maximum average total score is 13.16 for the group while the minimum score is 7.14. The group is thus considered recovered. In results the preliminary effectiveness of g-MCT on metacognitions and work-related self- efficacy for patients with GAD. Results in Table 5, show that there was a statistically significant decrease in MCQ-30 scores from pre-treatment (M=65.19, SD=10.99) to post-treatment (M=45.16, SD=9.39), t(22)=7.70, p<0.001. The mean decrease in MCQ-30 scores was 20.03. The effect size was large (d=1.6). Furthermore, there was also a statistically significant increase in RTW-SE scores from pre-treatment (M=3.48, SD=0.94) to post-treatment (M=4.35, SD=0.80), t(22) =-5.60, p < 0.001. The mean change in scores was 0.87. The effect size was large (d=1.16).
| pre-test | post-test | 95% CI for Mean Difference | Paired differences | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | N | SD | t | df | Sig.(two-tailed) | |||
| MCQ-30 | 65.19 | 10.99 | 45.16 | 9.39 | 23 | 14.63 | 25.42 | 12.48 | 7.70 | 22 | <.001 |
| RTW-SE | 3.48 | 0.94 | 4.35 | 0.80 | 23 | -1.20 | -0.55 | 0.75 | -5.60 | 22 | <.001 |
Table 5: Paired samples t-test results for MCQ-30 and RTW-SE.
Figure 3: Average score using PHQ-9 for 4 individual groups every group session with error bars.
The main purpose of this pilot study was to investigate whether g-MCT is a feasible, acceptable and effective method of treating patients diagnosed with GAD. The results indicate that g-MCT is indeed feasible and acceptable for the treatment of GAD. Patients gave positive feedback on the treatment in an anonymous self- evaluation form. The study also examined the preliminary effectiveness of g-MCT on anxiety, depression, metacognitions, and work-related self-efficacy using self-report questionnaires and found a significant reduction in symptoms of anxiety, depression and metacognitions, as well as a significant increase in work-related self-efficacy. The results suggest that g-MCT is an effective treatment for this patient group due to the large effect sizes and high recovery rates. For benchmarking purposes, the results of this study were compared with the results of Haseth [12], and van der Heiden. [13], which also found significant preliminary effectiveness of g-MCT on GAD.
Feasibility and acceptability of g-MCT for GAD
Comparing our pilot study to Haseth et al [12], pilot feasibility trial, we observed similar results. In our study, 13.2% of patients were excluded and not offered treatment. Additionally, one patient dropped out due to somatic health issues during our study, while no patients dropped out in this study [12]. This highlights the feasibility and acceptance of g-MCT as a treatment method for GAD in our findings, with a focus on recruitment, retention/ engagement, and dropout rates.
The preliminary effectiveness of g-MCT on anxiety and depression
In this pilot study, a total of 95.2% of patients were either recovered from their GAD diagnosis (57.1%) or improved (38.1%) post treatment. The studies by Haseth et al [12], and van der Heiden et al [13], were the two studies considered most appropriate for benchmarking in terms of symptom reduction as a result of g-MCT on GAD, and as shown in Table 4, their results are consistent with the results of our study.
In terms of assessing effect sizes, our study found an effect size of d=1.9 for GAD-7 and d=1.09 for PHQ-9. van der Heiden found an effect size of d=1.86 for the PSWQ and d=1.23 for the State-Trait Anxiety Inventory (STAI-T), while Haseth found a within-group effect size of the PSWQ of d=1.67 post treatment [12,13]. The similarities between these two studies further confirm the results of the effect sizes in our study. In summary, the large effect sizes in this study combined with a high recovery rate are strong indicators that g-MCT is effective in the treatment of GAD. The consistency of the results found in this study with previous studies in this field, supports the use of g-MCT as an effective form of therapy for patients with GAD.
Scores of comorbid depressive symptoms were also greatly reduced for patients in our study, with 47.6% of patients reporting a ≥ 6-point reduction in depressive symptoms, ultimately scoring below the clinical cut-off for PHQ-9 and were thus considered recovered from their depressive symptoms post-treatment.
The preliminary effectiveness of g-MCT on metacognitions and work-related self-efficacy
A statistically significant decrease in metacognitions was found post- treatment, with a 20-point decrease in reported metacognitions and a large effect size of 1.6. Although this study cannot be said to show a causal relationship between metacognitive beliefs and GAD symptoms, it is nevertheless an interesting observation that the observed data show an overall significant reduction in both areas. As for the RTW-SE, this study found a significant increase in these scores from pre (M=3.48) to post (M=4.35) treatment. With a mean change of 0.87 points and a large effect size of 1.16, these results indicate increased work-related self-efficacy in the patients who participated in the current study. As increases in RTW-SE questionnaire scores have been shown to predict actual return to work [15,16], these results are part of the growing body of evidence that reducing metacognitions and symptoms can contribute to improving work-related self-efficacy which may possibly contribute to patients' return to work.Strengths and limitations
The two therapists were trained in MCT and received supervision from a MCT level 2 therapist every two weeks in all three groups. The fact that these implemented GAD groups at Diakonhjemmet were part of a new treatment offer at the hospital and were not created for research purposes also provides a high level of ecological validity. An important focus of the treatment was to reduce the risk of sick leave and to help patients who were on sick leave to return to work. As work-related self-efficacy has been shown to significantly predict actual return to work [15,16], the RTW-SE assessment provides valuable information on patients' expected work status post-treatment and thus provides further data on this specific patient group.
Although this study has many strengths, it also has a few limitations. One of the obvious limitations is the number of patients included in the study. A small sample size increases the possibility of error and makes the study sensitive to potential dropouts and missing values, creating the possibility of a potentially biased result [38]. The therapists in this study spent an average of 3.1 therapy hours each per patient, which is less than in individual MCT. However, this does not include the time spent on recruiting patients, planning sessions and supervision with a level 2 MCT therapist. It is unclear which costs one should include in terms of assessing whether g-MCT is more time consuming than individual MCT. However, it is an important topic for further studies.
Another limitation is the solely use of self-report questionnaires, which can be biased by how patients feel at the time they receive and complete the questionnaire [39]. Furthermore, as there is no control group, these results may be due to treatment or other variables, such as elapsed time [40]. Another limitation is the lack of follow-up data in this study. However, similar clinical studies for patients with Common Mental Disorders (CMD) either on sick leave or at risk of sick leave from “Poliklinikk Psykisk Helse og Arbeid” show a stable, significant effectiveness of treatment with 87.2% (n=540) of patients working full time one-year post- treatment [41].
G-MCT is a well-received, feasible and acceptable treatment option for GAD, with a low dropout rate. In the current study, there was a significant reduction in GAD and depression symptoms following treatment, with 95.2% of patients classified as either recovered or improved. The results are consistent with existing benchmarking studies. There was a significant decrease in metacognitive beliefs and an increase in work-related self-efficacy. Future research should include a control group to increase the robustness of the results presented. Exploring the comparative effectiveness of individual MCT versus g-MCT for these patients could lead to more cost-effective treatment options in the future, ultimately promoting functional improvement and potentially reducing sick leave and associated risk.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kanafa K, Strømmen L, Hjemdal O, Lending HD, Hodne K, Hammersmark AT, et al (2024) Group Metacognitive Therapy for Patients with Generalized Anxiety Disorder at Risk for Sick Leave: A Pilot Study. J Psychol Psychother.14:476.
Received: 04-Mar-2024, Manuscript No. JPPT-24-29943; Editor assigned: 06-Mar-2024, Pre QC No. JPPT-24-29943; Reviewed: 20-Mar-2024, QC No. JPPT-24-29943; Revised: 27-Mar-2024, Manuscript No. JPPT-24-29943; Accepted: 03-Apr-2024 Published: 03-Apr-2024 , DOI: 10.35841/2161-0487.24.14.476
Copyright: © 2024 Kanafa K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.