Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2020)Volume 9, Issue 2
Background: The presence of both depression and diabetes is linked to poor compliance with diabetes care practices, lesser medication observance, rising incidence of complications thereby increasing the risk of emergency visits, hospitalization, and medical costs. It is therefore imperative to screen early and intervene timely this problem. However, information is limited to this problem in Ethiopia. So, this study assessed the magnitude of depression as well as its related factors in diabetes patients.
Methods: This survey was done at a diabetic clinic of Felegehiwot referral hospital, May to June 2017. The PHQ-9 tool has been implemented to screen depression. Systematic sampling was applied to recruit 58 types 1 and 363 types 2 diabetes respondents. Representativeness of sample for diabetes type 1 and 2 was assured with proportional allocation. We used an internal comparison to designate depression in diabetes types 1 and 2. Binary logistic regression was fitted to identify factors. Odds ratio (OR) with 95% CI was computed and variables with a p-value of<0.05 in the final model were declared significant.
Results: The participant’s response rate was 421 (96.3%). The overall prevalence of depression was 163 (38.7%) with moderate, moderately severe and severe depression being 100 (23.75%), 39 (9.25) and 24 (5.7%) respectively. The magnitude of depression among type 1 diabetes mellitus (Type 1 DM) was 29 of 58 (50%) and it was 134 of 363 (36.9%) in type 2 diabetes mellitus (Type 2 DM). Age of 45- 54 years (AOR=2.64, 95%CI: 1.38, 8.95), poor medication adherence (AOR=1.35, 95% CI: 1.18, 5.85), poor social support (AOR=1.21, 95% CI: 1.06, 4.34) and coexistence of medical illness (AOR=2.52, 95% CI: 1.28, 6.39) were the factors associated with depression.
Conclusion: Overall, nearly four in ten diabetes patients (38.7%) had depression. Depression was higher in type 1 DM patients (50%) than type 2 DM patients (36.9%). Age, poor social support, poor medication adherence and coexistence of medical illness were associated with depression. Therefore, the system of care for diabetes patients should focus on routine screening and management of depression and its associated factors.
Depression severity; Diabetes; Ethiopia
AOR: Adjusted Odds Ratio; BDI: Beck Depression Inventory-II; BMI: Body Mass Index; CI: Confidence Interval; COR: Crude Odds Ratio; DF: Degree of Freedom; DM: Diabetes Mellitus; FBS: Fasting Blood Sugar; FHRH: Felege Hiwot Referral Hospital; HTN: Hypertension; OR: Odds Ratio; PHQ-9: Patient Health Questionnaire-9; SD: Standard Deviation; SPSS: Statistical Package for Social Science; Type 1 DM: Type 1 Diabetes Mellitus; Type 2 DM: Type 2 Diabetes Mellitus; USA: United States of America
Diabetes mellitus is an abnormality in the metabolic pathways of carbohydrates and lipids because of either decreased insulin secretion or increased resistance to insulin action [1]. Global statistics indicate millions of people across the world had been influenced by this illness and by the year 2013, 382 million people were living with this illness (DM) and projections estimated that 592 million people will be influenced by 2035 [2,3] in which most will resides in low and middle-income countries.
Twenty-eight percent of burden of disease globally is due to neuropsychiatric disorders and the share to depression is onethird as reported from World health organization (WHO) implying that of mental illness, it is among the top burden causing illness with 10% of disability-adjusted life years in relatively less-developed nations [4] and with this rapid shift in epidemiologic transition projections indicates that it will rank second as disability cause in 2020 with estimated burden of 5.7% [4]. The biggest depression burden in the African continent resides in Northern Africa [5]. A survey at the national level in Ethiopia found that 9.1% of the population was depressed [6]. Besides, a meta-analysis of depression in Ethiopia among the general population provided a pooled prevalence of 20.5% [7]. Since DM is a psychologically challenging medical condition [8,9] due to the intricacy of its pathophysiology and chronicity of its management, emotional disorders are highly prevalent; it might reach 84% and 80% for mood and anxiety disorders respectively [10,11]. Bidirectional relation existed between depression and diabetes; the presence of one will predispose to the other [12,13].
Prior studies implied that depression amongst DM patients was 18% [14], 30.2% [15] and 59.8% [16] in three united states of America (USA) studies, 50–60% in Asia [17,18], 54.1% in Nepal [19], 45.2% in Bangladesh [20], 40.3% in Malaysia [21], 43.5% in Pakistan [22], to (25.3–35.4%) in India [23,24], 27.8% in Nigeria [25], 15.4% [26] at Gondar, Ethiopia, 61% [27] and 44.7% [28] in two studies at Addis Ababa, Ethiopia. This implied that depression is highly prevalent [29-31], even though it is under-diagnosed in 50-75% of occasions and not well managed especially in sub-Saharan African countries [32,33].
Research articles published previously suggested that sociodemographic variables such as being single [12,34], unemployment [35-37], poor social support [12,28,36-38]; clinical variables like poor glycemic control [39-41], medication non adherence [42-44], diabetic complications [27,38,40,42,45,46], being overweight [1,36,40,42,44,47], length of stay with diabetes [26,27,42], Presence of other medical conditions [27,45] and cigarette smoking [36,37,42,48,49] from substance related variables were contributing factors to depression.
Presence of depression in DM population had a huge impact on life quality due to its multidimensional effect on medication compliance, and outcomes of treatment [50-52], causing blood sugar fluctuation [53], cost complications due to excessive health care utilization [54], impairment in patients functioning [55], and an overall elevated risk of early death [56]. Besides, a pooled estimate study in the USA concluded that depression increases the risk of both macrovascular as well as microvascular complications of DM and sexual dysfunction [57]. Also, depression affects the self-efficacy of DM patients [58] which is important for diabetic self-care [59]. Moreover, important healthy behaviors would be adversely affected by depression that may results in substance use, physical inactivity and poor cognitive functioning [60].
Although depression is among the leading causes of disability and burden of disease and its high prevalence in diabetes patients, much is not investigated and timely information in this regard is limited. This problem is much pronounced in unindustrialized countries including Ethiopia. Despite, few studies are present in Ethiopia they were only descriptive [38], conducted on only type 2 diabetes mellitus (Type 2 DM) [28,38].
Our hypothesized goal in this study is to assess the magnitude and related factors for depression among both Type 1 and 2 DM patients in North West Ethiopia. To that end, the assessed the hypothesized objectives and the results obtained from this study would be beneficial evidence in early detection of depression which will be essential in the early initiation of intervention for depression as well as the related factors for occurrence of depression in diabetes mellitus patients.
Study setting and design
This survey was implemented over one month from May to June 2017 at FHRH outpatient diabetic clinic, Bahirdar. Bahirdar is the central city of Amhara Regional State, with an approximate distance of 578 km from the capital city of Ethiopia. Data from a census conducted by a central statistical agency of Ethiopia in 2007 found that the catchment population of the city was 221,991 [61] and a catchment population of larger than 5.5 million people has been getting service in the hospital. So far higher than 1984 DM clients have been listed in the clinic documentation book. On average the outpatient diabetic therapeutic attendance of the clinic per month and week is 1384 and 346 respectively.
Study participants
We used the single population proportion formula to estimate the magnitude of sample considering the prevalence of 44.7% for depression [28], 5% margin of error, 95% confidence level and 15% non-response rate and it was computed to be 437. We used patients register book to decide the amount of DM patients to have a follow up in the month of study period and by taking the average of past consecutive three months follow up and it was found that 1200 type 2 DM and 184 types 1 diabetes mellitus (Type 2 DM) patients have an appointment in the data collection time. To assure the representativeness of both types of DM, a proportional allocation method was implemented to obtain 63 types 1 and 374 types 2 DM patients to be incorporated in the survey. The sampling interval was computed to be 3 for both type 1 and 2 DM subjects.
The first patient has been nominated using a lottery method and every third of patients were included until the final sample size was achieved. All adult diabetic patients aged 18 years and older who attend with follow up visits during the time of the study were invited to take part. However, newly diagnosed DM patients, diabetic patients with a serious acute complication that makes the interview situation unethical and difficult were skipped.
Data collection procedures and instruments
Amharic translation of questionnaires was performed before the data collection process since the Amharic language is the working language for participants. A pre-test was also done among twenty-one diabetes mellitus patients (5%) of sample size at Abaymado Hospital; a hospital located about 5 km away from the study area. Three BSc nurses were involved in the data collection. The data collectors and supervisors were given short term training about study aims, procedures, ethical issues, and data quality control methods. Continuous supervision was done by supervisors and principal investigators throughout the data collection process.
Depression was assessed using the Patient Health Questionnaire-9 screening instrument the Amharic version of which had been validated in Ethiopia. The PHQ-9 asses depressive symptoms in past 2 weeks and consisted of 9 questions each of which can be scored from 0 (not at all), 1 (several days), 2 (more than half of the days), or 3 (nearly every day) with an overall score ranging from 0 to 27 in which scores of 1-4, 5-9, 10-14, 15-19 and 20-27 representing absence of depression, mild depression, moderate depression, moderately severe depression and severe depression in respective order [62]. This tool had been used in plenty of studies formerly in Ethiopia [26,28,38].
The level of adherence to diabetic medication was assessed as poor, medium and high adherence using the Morisky-8 medication adherence scale. Poor-adherence was defined as a score of less than 6, medium adherence with a score of 6-7 and high adherence with a score of 8 [64-66]. Furthermore, social support was assessed using the Oslo-3 item social support scale. Poor social support, moderate social support, and good social support were defined at cut-off points 3-8, 9-11 and 12-14 points respectively [67]. Current substance use was defined as nonmedical use of the mentioned substances (chat, cigarette, and alcohol) in the last 3 months [68]. We utilized Fasting blood sugar (FBS) level of the previous visit to classify glycemic control into good (reading ≤ 130 mg/dl) and poor (reading >130 mg/dl) [69] and medical chart of patients was used to obtain data regarding FBS level, comorbidity, and complication of diabetes patients.
Besides, we developed questionnaires for socio-demographic factors after reviewing conceptual as well as empirical literature documented previously.
Data processing and analysis
Epi-info version 7 was used as a data entry tool and SPSS-20 had been employed to analyze the data after it was exported from Epi-info. Descriptive methods such as frequency, median, standard deviation mean and crosstabs were employed in summarizing depression and independent variables. A logistic regression model was fitted to identify related factors for depression. A p-value <0.25 in the bivariate analysis was used as fitting criteria into multivariable logistic regression. An Odds ratio with 95% CI had been employed to show association strength and a p-value of <0.05 in multivariable logistic regression were statistically declared as significant. We employed Hosmer and Lemeshow test to check model fitness and Collinearity was also checked with Standard error of independent variables and not a problem in the present study.
Ethical considerations
The authors request the ethical institutional board of university of Gondar and AMSH that reviews the ethical consideration of research procedures to take oral consent since the research procedures imposes minimal risk to participants. The mentioned institution above therefore approves the ethical soundness of the research with a letter. Furthermore, a supportive letter from Felegehiwot hospital administration had been obtained before commencement of study procedures. Consent was taken verbally from each study participant after explanation and supplying sufficient information regarding the aim of the research to the individual participant and society in general, procedures to be implemented. Participants were also informed about their rights not to participate or to withdraw at any time from the study. Participation was voluntary and information was collected anonymously by assuring confidentiality throughout the data collection period and also after the study. Patients with severe depression were linked for a psychiatric service in the hospital.
Socio-demographic characteristics of participants
The response rate was 421 (96.3%). The mean age ( ± SD) of participants was 38.0 (±13.9) years. Two hundred twenty-seven (53.9%), three hundred fifty-three (83.6%), two hundred fifty-six (60.8%), one hundred ninety-two (45.6%) and one hundred ninety-six (46.6%) were males, orthodox, married, non-educated and farmers respectively. Considering the level of social support 242 (57.5%), 128 (30.4%) and 51 (12.1%) were with poor, moderate and strong support respectively (Table 1).
| Variables | Frequency | Percentage |
|---|---|---|
| Age group | ||
| 18-24 | 74 | 17.6 |
| 25-34 | 116 | 27.6 |
| 35-44 | 97 | 23 |
| 45-54 | 77 | 18.3 |
| = 55 | 57 | 13.5 |
| Sex | ||
| Male | 227 | 53.9 |
| Female | 194 | 46.1 |
| Marital status | ||
| Married | 256 | 60.8 |
| Single | 93 | 22.5 |
| Widowed/divorced | 72 | 16.7 |
| Religion | ||
| Orthodox | 352 | 83.6 |
| Muslim | 51 | 12.1 |
| Protestant | 18 | 4.3 |
| Occupation | ||
| Government employee | 71 | 16.9 |
| Private employee | 58 | 13.8 |
| Unemployed | 28 | 6.7 |
| Farmer | 196 | 46.6 |
| Student | 26 | 6.2 |
| Others | 42 | 10 |
| Educational status | ||
| No formal education | 192 | 45.6 |
| Grade 1-8 | 93 | 22.1 |
| Grade 9-12 | 58 | 13.8 |
| Diploma and above | 78 | 18.5 |
| Monthly income | ||
| < $27 | 159 | 37.8 |
| $27-$43.56 | 96 | 22.8 |
| >$43.56 | 166 | 39.4 |
| With whom patient is living | ||
| With family | 375 | 89 |
| Alone | 46 | 11 |
| Social support | ||
| Poor | 242 | 57.5 |
| Moderate | 128 | 30.4 |
| Strong | 51 | 12.1 |
Table 1: Socio-demographic description of study participants at Felegehiwot referral hospital (n=421), Bahirdar, Ethiopia, 2017.
Clinical and substance use characteristics of the respondents
The mean BMI ± SD of DM participants was 21.89 ± 13.65 kg/m2. Three hundred thirty-three (79%) of study participants are in the normal BMI range (18.5 kg/m2- 24.5 kg/m2). Three hundred sixty-three (86%) and 56 (14%) of participants were type-II and type-I DM cases respectively. One hundred eightyfour (43.7%) were on insulin therapy. Two hundred fifty-seven (61%) had been living with diabetes for <5 years. Fifty-six (13.3%) of subjects had comorbid medical illnesses in addition to DM. One hundred thirty-six (32.3%) of the respondents had a history of substance use within the past three months before data collection time. Among these; the majority, 123 (90.5%) reported that they were using alcohol and 11 (8%) of them were smoking a cigarette (Table 2).
| Variables | Frequency | Percentage |
|---|---|---|
| Type of DM | ||
| Type 1 | 58 | 13.8 |
| Type 2 | 363 | 86.2 |
| Duration since DM dx | ||
| <5 years | 257 | 61 |
| >=5 years | 164 | 39 |
| Current DM treatment | ||
| Insulin | 184 | 43.7 |
| Insulin and oral agents | 57 | 13.6 |
| Oral hypoglycemic agents | 180 | 42.8 |
| Comorbid medical illness | ||
| Hypertension (HTN) | 44 | 10.5 |
| HIV | 6 | 1.5 |
| Asthma | 3 | 0.65 |
| Renal diseases | 3 | 0.65 |
| No medical illness | 365 | 86.7 |
| Complication due to DM | ||
| Yes | 18 | 4.3 |
| No | 401 | 95.2 |
| Glycemic control | ||
| Poor | 205 | 48.7 |
| Good | 216 | 51.3 |
| Medication adherence | ||
| Low | 85 | 20.2 |
| Medium | 167 | 39.7 |
| High | 169 | 40.1 |
| Moderate physical activity | ||
| Yes | 129 | 30.6 |
| No | 292 | 69.4 |
| Co morbid depression | ||
| Yes | 163 | 38.7 |
| No | 258 | 61.3 |
| Body mass index (kg/m2) | ||
| < 18.5 | 40 | 9.5 |
| 18.5-24.9 | 333 | 79.1 |
| = 25.00 | 48 | 11.4 |
| Family history of suicidal attempt | ||
| Yes | 15 | 3.6 |
| No | 406 | 96.4 |
| Current substance use | ||
| Yes | 136 | 32.3 |
| No | 285 | 67.7 |
| Current cigarette smoking | ||
| Yes | 11 | 2.6 |
| No | 410 | 97.4 |
Table 2: Clinical and substance related characteristics of diabetic patients attending Felegehiwot referral Hospital, Diabetic Clinic (n=421), Bahirdar, Northwest Ethiopia, July 2017.
The magnitude of depression and its severity among study participants
The frequency of depression in DM subjects was 38.7% (95% CI: 34.20, 43.50). Regarding severity 100 (23.75%), 39 (9.25) and 24 (5.7%) of depressed participants were with moderate, moderately severe and severe depression respectively (Figure 1). Depression was higher among type 1 DM subjects (50%) than type 2 DM subjects (36.9%), despite this was not significant statistically (X2 =3.60, P=0.061) which suggests that depression is independent of the DM type. Depression is also slightly lower among males (37.5%) than females (40%). Moreover, the magnitude of depression is higher among participants with comorbid medical illness (54.5%) than those without comorbid medical conditions (36.3%) and this difference is significant statistically (X2 =6.68, P=0.01).
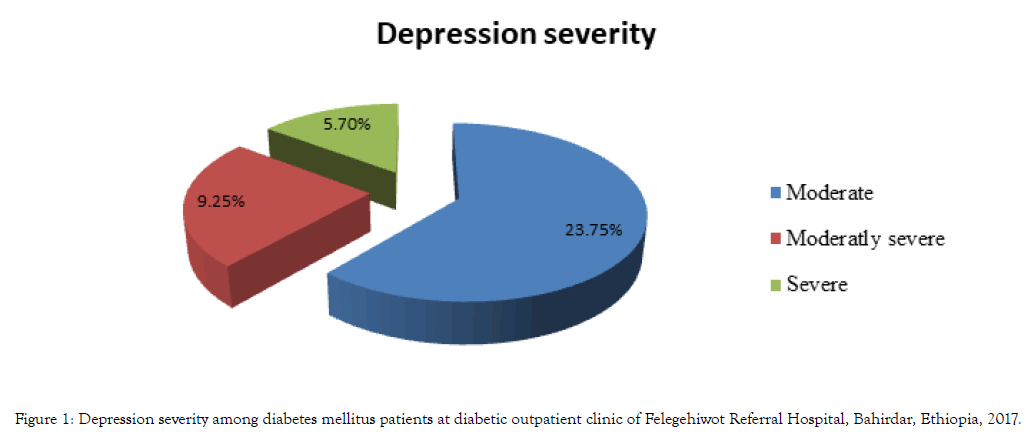
Figure 1: Depression severity among diabetes mellitus patients at diabetic outpatient clinic of Felegehiwot Referral Hospital, Bahirdar, Ethiopia, 2017.
Factors associated with depression in diabetes mellitus patients at Felegehiwot referral hospital.
Medication non-adherence, poor social support, age group (45-54 years) and the presence of medical comorbidity were the identified factors for depression. Participants with age from 45 to 54years were two-point six times (AOR=2.64, 95%CI: 1.38, 8.95) at a higher odds of developing depression than those with the age of 55years and above. Besides, respondents who were with poor adherence to their medication had a thirty-five per cent (AOR=1.35, 95% CI: 1.18, 5.85) bigger vulnerability to depression than those with high medication adherence.
Besides, a poor level of social support was also another factor reasonably having a statistically significant association with depression; respondents with poor social support were twentyone percent (AOR=1.21, 95%CI: 1.06, 4.34) at a higher probability of developing depression than respondents of good social support.
Moreover, Coexisted medical problem in addition to DM was also responsible for the occurrence of depression. Participants who were diagnosed by a medical practitioner to have an additional medical illness on the top of DM had almost two and half times higher odds of becoming depressed than DM participants who were not diagnosed with an additional medical illness (AOR=2.52, 95% CI: 1.28, 6.39) (Table 3).
| Depression | ||||
|---|---|---|---|---|
| Explanatory variables | Yes | No | COR (95% CI) | AOR (95% CI) |
| Current DM treatment | ||||
| Insulin | 81 | 103 | 1.36 (0.89,2.07) | 1.32 (0.89,2.07) |
| Insulin and oral agents | 16 | 41 | 0.67 (0.35,1.29) | 0.61 (0.31,1.20) |
| Oral agents only | 66 | 114 | 1 | 1 |
| Comorbid-medical illness | ||||
| Yes | 30 | 25 | 2.83 (1.58, 7.45) | 2.52 (1.28,6.39)a |
| No | 133 | 233 | 1 | 1 |
| Medication adherence | ||||
| Poor | 31 | 54 | 1.52 (1.29, 4.37) | 1.35 (1.18, 5.85)a |
| Intermediate | 74 | 93 | 1.09 (0.64,1.89) | 0.90 (0.71,2.55) |
| High | 58 | 111 | 1 | 1 |
| Type of DM | ||||
| Type 1 DM | 29 | 29 | 0.59 (0.27,1.32) | 1.55 (0.81,2.91) |
| Type 2 DM | 134 | 229 | 1 | 1 |
| Current substance use | ||||
| Yes | 104 | 181 | 0.75 (0.49,1.14) | 0.79 (0.51,1.25) |
| No | 59 | 77 | 1 | 1 |
| Social support | ||||
| Poor | 101 | 141 | 1.4 (1.15, 3.48) | 1.21 (1.06, 4.34)a |
| Moderate | 40 | 74 | 1.06 (0.57,2.01) | 0.85 (0.43,1.68) |
| Strong | 22 | 43 | 1 | 1 |
| Age of respondents | ||||
| 18-24 | 32 | 42 | 2.58 (1.19,5.57) | 1.83 (0.77,4.32) |
| 25-34 | 45 | 71 | 2.15 (1.04, 4.42) | 1.83 (0.85,3.95) |
| 35-44 | 37 | 60 | 2.09 (0.99,4.38) | 2.11 (0.96,4.95) |
| 45-54 | 36 | 41 | 2.99 (1.39,6.38) | 2.64 (1.38, 8.95)a |
| 55 and above | 13 | 44 | 1 | 1 |
Table 3: Bivariate and multivariable Logistic Regression analysis result showing the associations between the factors and depression among diabetic patients at Felegehiwot Referral hospital, Bahir Dar, Ethiopia, 2017 (n=421).
This study assessed the magnitude and related factors for depression among both Type 1 and 2 DM patients in North West Ethiopia. We believe that the results obtained from this study would be beneficial evidence in early detection of depression which will be essential in the early initiation of intervention for depression as well as the related factors for occurrence of depression in diabetes mellitus patients.
The result of the study displayed that nearly four in ten DM subjects were depressed. Slightly higher depression was observed in type 1 DM subjects; 28 of 58 (50%) than type 2 DM; 134 of 363 (36.9%). Poor adherence to medication, poor social support, and age (45-54years) and comorbid medical illness were the factors responsible.
The present finding is in line with studies in Malaysia (40.3%) [21], Pakistan (43.3%) [22], India (25.3 - 35.4%) [23,24] and Ethiopia (43.6%) [70]. Oppositely, it was lower as comparatively seen with prior studies in united states of America (USA); 59.8% [16], Asia; 50 – 60% [17,18], Nepal; 54.1% [19], Bangladesh; 45.2% [20], India; 45.2% [71] and two Ethiopia studies; 61% [27], 44.7% [28]. Such a variance would be attributed to the discrepancy in sample and assessment methods. Only 112 type 2-DM subjects in USA [16], 110 and 140 participants in Asia [17,18], 157 patients in Nepal [19], 230 type 2 DM patients in India [72], 264 and 313 DM cases in Ethiopia [27,28]. Assessment tools were hospital anxiety and depression scale in Asian studies [17,18], Hamilton depression scale in Ethiopia [27] which might be responsible for this.
On the opposing side, the current finding was greater than prior studies in USA; 18%-30.2% [14,15,73], Poland, 17% [73], 30.5% in Bangladesh [74], Nigeria, 27.8% [25], 15.4% in Gondar [26] and 17% at Mekelle [45]. This might happened due to the larger sample size used; 1803 patients in the USA study [15], 477 patients in Poland study [75]. Different tools used such as children's depression inventory in Poland, Composite International Diagnostic Interview USA, depression manual of the mini-international neuropsychiatric interview in Nigeria and BDI-II in Ethiopia might also contribute. Moreover, variance in risk factors for depression between current and prior studies could be accountable for the difference in the magnitude of depression.
Poor social support had also been related to depression. Respondents with poor social support were twenty-one percent at a higher probability of developing depression than respondents with good social support Such a relationship between social support with depression was evidenced by several prior studies [12,13,28,36-38,76,77]. The reason could be poor social interaction across the patient’s social networks lowering the quality of life of patients and thus increasing the risk of depression [78].
Age was also a factor with a statistically valid relationship with depression in the present study. The respondents whose age was from 45 to 54years were two-point six times at a higher risk of developing depression as compared to those with age of 55years and above. This was reinforced by studies in Malaysia [21], Pakistan [22], Bangladesh [20], India [71] and Ethiopia [27].
The way respondents adhere to their diabetic management was also identified as having a significant contribution to the development of depression in DM cases. Diabetic cases that were poorly adhered to medication had a 35% higher risk of developing depression than cases with high medication adherence. This conclusion is dependable with previous studies from Minnesota, USA [43], Washington, USA [44] and Ethiopia [45]. This can be warranted with poor medication compliance bringing about poor glycemic control and studies support that poor glycemic control is highly associated with depression [42,54] as the quality of life of people with poor glycemic control deteriorates [78] and further prospective studies need to be considered to approve such hypothesis.
Moreover, coexisted medical problem besides DM was also responsible for the high occurrence of depression. Participants who were diagnosed by a medical practitioner to have an additional medical illness on the top of DM had almost two and half times higher odds of becoming depressed than DM participants who were not diagnosed with additional medical illness. This was in line with a finding from former [17,19,27,74,79,80] studies This could be explained by the increased health care cost, frequent complications and restrictions in mobility as well as impairment in functioning in the presence of additional medical comorbidity [81].
Although cigarette smoking and depression did not show a relationship in the present survey, smoking cigarettes increases the risk of developing comorbid depression in diabetes mellitus patients as supported by empirical evidence in different countries [36,37,42,49,50].
This could be due to the small number of participants with cigarette smoking in the current study. Besides, cultural factors in which smoking cigarettes not culturally acceptable in our culture but may be considered culturally as normal in most of the countries at which previous studies mentioned above were piloted.
The prime limitations of the study emanate from the crosssectional nature that makes causality inference difficult. Next, we assessed depression with PHQ-9 and some of the elements of this tool like appetite problem, a problem with sleep and fatigability can be greatly affected since they are common complains of DM patients. So overestimation of depression could have happened. Besides, social desirability bias as data was collected by interviewer-administered questionnaires should be taken into consideration.
Overall, nearly four in ten DM participants (38.7%) were depressed with 23.75%, 9.25% and 5.7% having moderate, moderately severe and severe depression respectively. Depression was relatively higher in type 1 DM cases (50%) than type 2 DM cases (36.9%). Age, poor social support, poor medication adherence, and comorbid medical illness were related factors. Therefore, the system of care for diabetes patients should allow routine depression screening that can help to take immediate intervention and prevents further problems. Moreover, the factors described above that were responsible for the outcome variable should be targeted in the managing procedure for a diabetic patient.
The authors request the ethical IRB of UOG that reviews the ethical concern of study processes to take oral consent since it imposes a negligible risk to participants. The mentioned institution above therefore approves the ethical soundness of the study with a letter. Consent was taken verbally from each study participant. Involvement was voluntary and data has been collected namelessly by guaranteeing confidentiality during the data assortment period and also after the study. Patients with severe depression (PHQ-9 score≥10) were linked for further evaluation in the hospital.
Not applicable
The datasets used throughout this research process are available from the corresponding authors on reasonable request.
None.
The research fund was supported by Amanuel Mental Hospital. However, the funding organization played no role over study designation, analysis of data and manuscript preparation.
MN was the principal investigator designing the research and doing the whole research analysis. MN, MT, and YG involved in manuscript preparation. All of the authors approved the final version of the manuscript.
We deeply acknowledge Gondar University College of medicine and health science & Felegehiwot referral hospital for all forms of help provided. Besides, we would like to acknowledge the participants, data collectors, and supervisors for active involvement in the study process.
Citation: Necho M, Tsehay M, Getachew Y (2020) Half of Type 1 and Nearly Four in Ten of Type 2 Diabetes Patients Were Living With Depression in North West Ethiopia, Amhara Region. J Dep Anxiety. 9:359. doi: 10.35248/2167-1044.20.9.359
Received: 28-Apr-2020 Accepted: 18-May-2020 Published: 25-May-2020 , DOI: 10.35248/2167-1044.20.9.359
Copyright: �?�© 2020 Necho M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : The research fund was supported by Amanuel Mental Hospital. However, the funding organization played no role over study designation, analysis of data and manuscript preparation.