Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Research Article - (2020)Volume 12, Issue 2
Introduction: the current burden of the spreading coronavirus (Covid-19) implied an action to review our basic strategies in hand hygiene practice. This calls for effective infection control measures in health care settings, in particular hand hygiene. Hence, hand hygiene practice will continue to be a concern and are essential to explore to bridge the theory practice gap.
Methodology: Cross sectional observational study was conducted from February to March 2020 at Jugal hospital, Harar, Ethiopia, which is found 525 km to East of Addis Ababa. Ethical clearance was obtained from Harar Health Science College institutional review board (IRB) (Ref.no.HHSC-27/2020). Consent was obtained from both administrative body and respondent. SPSS version 20 was used for data analysis.
Result: Majority 99 (59.64%) said that they use Soap bar followed by 57(34.34%) only water and 10(6.02%) alcohol base sanitizer, whereas there is no any one answered Chlorhexidine solution and Liquid hand wash use for hand washing. Only 7 (4.22%) washed their hands when switching from one patient to the second patient. Only twenty seven (16.27%) followed correct sequence in hand washing. Shared ward towels drying was the preferred method of hand drying after washing which was seen in 111 (66.87%) of the participants. Lack of water and soap were the major constraints against washing hands which was seen among 122 (73.49%)
Conclusion: Very poor practice with Hand washing practices among studied Health Care Workers is calling for urgent intervention. Implementing five movements of hand hygiene are the best method for preventing healthcare associated infections. Therefore, the health care provider should be followed this principle to fight healthcare associated infections.
Hand washing practice; Jugal hospital; Health care workers
Hand hygiene (HH) is a compliance of cleansing hands using soap and water or using antiseptic hand rub for removal of transient microorganism from hands and in the way of keeping the skin condition. [1]. Any action of hand cleaning is referred to as hand hygiene [1].
Hand hygiene is simple, easily implemented and an effective practice that can reduce the risk of infection [2]. Proper hand hygiene before and after each contact with any patient is an important measure to prevent Hickman catheter-related infection (HCRI) in cancer patients [3].
Hospital-acquired infections are a major threat to patients. It is estimated that annually about hundreds of millions of patients suffer from health care associated infections (HCAIs) worldwide [1]. Hospital acquired infection through the hands of health care workers is mostly due to poor hand hygiene of the health care providers [4].
Annually regarding many numerous patients have suffered from HCAIs worldwide [4]. Improper hand hygiene by HCPs is answerable for regarding 40% of health facility infections [5]. Health care related infection is estimated to affect 10% of patients in developed countries, and 25% in developing countries [6].
Understanding the WHO “SAVE LIVES: Clean Your Hands” program that reinforces the “My 5 Moments for Hand Hygiene” approach as key to protect the patients; HCWs and the healthcare environment against the spread of pathogens and thus reduce Healthcare-associated infections (HAIs). That approach encourages HCWs to clean their hands: before touching a patient, before clean/aseptic procedures, after body fluid exposure/risk, after touching a patient and after touching patient surroundings [7].
The importance of hand hygiene is not sufficiently recognized by health care workers and poor compliance has been documented repeatedly [4]. Notable factors for poor compliance include hand irritation, inaccessibility or shortage of handwashing equipment, dense working conditions and poor knowledge [4]. Others include work overload and insufficient time, negative attitude and wrong beliefs about HH and IC practices, improper supervision, and lack of training and absence of role model. [8].
Additionally, the current burden of the spreading coronavirus (Covid-19) implied an action to review our basic strategies in hand hygiene practice.
This calls for effective infection control measures in health care settings, in particular hand hygiene. Hence, hand hygiene practice will continue to be a concern and are essential to explore to bridge the theory practice gap. Thus, the aim of this study was to assess the hand hygiene practice among health care workers.
Study setting and participants
The institutional cross sectional quantitative observational study was conducted from February to March 2020 at Jugal hospital, Harar, Ethiopia, which is found 525 km to East of Addis Ababa. The hospital has a total of 342 health professionals. The study was conducted among sampled 166 staffs in Jugal hospital. Ethical clearance was obtained from Harar Health Science College institutional review board (IRB) (Ref.no.HHSC-27/2020). Before staring of a field work, Consent was obtained from both administrative body and respondent.
Data collection tool
Six nurses were trained on observing health care workers ’ (HCWs) hand washing practices during hand washing opportunities.
Data collection sheets were prepared for recording observations for each health worker being observed. Health care workers in Jugal hospital were observed during routine patient care for compliance with hand washing. The observing nurses unnoticeably recorded health workers hand washing practices in the data sheets. The observation periods were distributed randomly during the day as well as at night for 28 days.
The subjects were unaware that they were being observed. Each subject was observed once and the observation was recorded with the time of the event.
Data analysis procedure
For data processing and analysis, SPSS version 20 was used. Data was checked for completeness and consistency; Coded data was entered into computer programs after the required cleaning was done. Descriptive analyses were performed.
One hundred sixty six (166) health workers participated in the study. The mean age of the participants was 29 years of age, more than half 92(55.42%) were female, 112(67.47%) were nurses,67 (40.36%) of them were working in the hospital for less than 1 year and all of the participants answered that they practice hand washing (Table 1).
| Variable | Frequency | Percent | |
|---|---|---|---|
| Gender | Male | 74 | 44.58 |
| Female | 92 | 55.42 | |
| Age (years) | < 25 | 14 | 8.43 |
| 25-34 | 89 | 53.61 | |
| 35-44 | 36 | 21.69 | |
| 45 + | 27 | 16.27 | |
| Profession | Doctor | 19 | 11.45 |
| Nurse | 112 | 67.47 | |
| midwives | 18 | 10.84 | |
| Laboratory technician | 17 | 10.24 | |
| Years of Practice | <1 | 67 | 40.36 |
| 01-05 | 49 | 29.52 | |
| 06-10 | 33 | 19.88 | |
| 10 + | 17 | 10.24 | |
| Do you practice hand washing | Yes | 166 | 100 |
| No | 0 | 0 |
Table 1: Socio-demographic characteristics of the respondents.
Products used for Hand hygiene
The respondents used various products to clean or wash their hands at their work place. Majority 99(59.64%) said that they use soap bar followed by 57(34.34%) only water and 10(6.02%) alcohol base sanitizer, whereas there is no any one answered Chlorhexidine solution and Liquid hand wash use for hand washing.
Reasons why the respondents washed their hands at the workplace
Only 7 (4.22%) washed their hands when switching from one patient to the second patient, 133(80.12%) washed hands while going home after day’s work whereas all 166 (100%) wash their hand After touching blood, body fluids, secretions (Table 2).
| Frequency | Percent | |
|---|---|---|
| Immediately on arrival at work. | 10 | 6.02 |
| Before putting on gloves | 21 | 12.65 |
|  after removing gloves | 123 | 74.1 |
| After touching blood, body fluids, secretions | 166 | 100 |
| Before contact with patients | 21 | 12.65 |
| Between patients | 7 | 4.22 |
| After contact with patients without glove | 111 | 66.87 |
| Before a procedure | 11 | 6.63 |
| After a procedure | 123 | 74.1 |
| After a day’s work | 133 | 80.12 |
Table 2: Reasons why the respondents washed their hands at Jugal hospital, Harar, Ethiopia, 2020.
How the hands was washed
Only twenty seven (16.27%) followed correct sequence in hand washing. Starting from Remove jewelry, turn on the tap, wet hands thoroughly under running water, Soap hands adequately, Rub hands vigorously front and back, in between fingers, finger tips, the sides of the hand, the thumbs, up to and including the wrists then Rinse under clean running water until all soap removed.
Method of hand drying after washing
Shared ward towels drying was the preferred method of hand drying after washing which was seen in 111 (66.87%) of the participants (Figure 1).
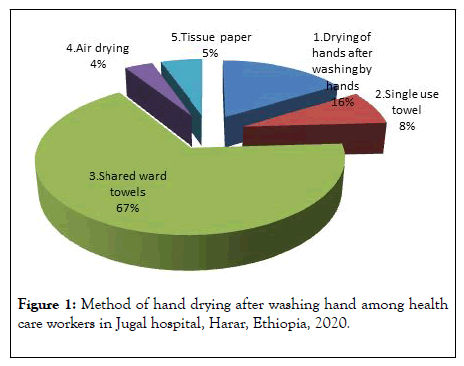
Figure 1: Method of hand drying after washing hand among health care workers in Jugal hospital, Harar, Ethiopia, 2020.
Barriers to compliance with hand hygiene practices
Lack of water and soap were the major constraints against washing hands which was seen among 122 (73.49%) HCWs whereas the least cause was Hand washing agents cause irritation and dryness among 11(6.63%) (Table 3).
| 1 | Lack of water | Frequency | Percent |
|---|---|---|---|
| 2 | Sinks are inconveniently located/lack of sinks | 74 | 44.58 |
| 3 | Lack of soap and water | 122 | 73.49 |
| 4 | Too busy/insufficient time | 87 | 52.41 |
| 5 | Understaffing/overcrowding | 27 | 16.27 |
| 6 | Unavailability of alcohol-based hand rubs | 37 | 22.29 |
| 7 | Lack of knowledge about guidelines/ protocols | 87 | 52.41 |
| 8 | Hand washing agents cause irritation and dryness | 11 | 6.63 |
| 9 | Patient needs take priority | 76 | 45.78 |
| 10 | Always wearing gloves | 44 | 26.51 |
| 11 | Low risk of acquiring infection from patients | 13 | 7.83 |
| 12 | I easily forget | 101 | 60.84 |
| 13 | No place to wash hands | 31 | 18.67 |
Table 3: Barriers to compliance with hand hygiene practices among health care workers in Jugal hospital, Harar, Ethiopia, 2020.
This is particularly true in the current course of Corona Virus(COVID-19) at international level Healthcare Workers have to be alert to strict infection control procedures such as hand hygiene practice.
The results of study show that the majority of respondents were nurses and female. Nurses contribute to the majority population of the health care workers in many health institutions. Nurses constitute the largest percentage of the health care workers (HCW) [9] and they are the “nucleus of the health care system” [10]. Because they spend more time with patients than any other HCWs, their compliance with hand washing guidelines seems to be more vital in preventing the disease transmission among patients. Nursing profession is mainly dominated by females throughout the world. Therefore it is not surprising that the majority of respondents were females.
In this study the majority of the participants were young population with a mean age of 29 years much younger population and the majority of them were between the ages of 20 and 34 years. It is similar with research was done in Sokoto State, Nigeria, another study conducted in Nigeria, study conducted in Ghana, [11-13]. The reason behind the majority of the study participants were young population in fact that 70% of the study participants have spent less than five(5) years in service among this 40% are newly recruited and spent less than one (1) year in the facility.
The most commonly used hand cleaning agent among the respondents was soap and water in many studies. In this study Majority 59.64% of the participants said that they use Soap bar for hand washing, the result showed that it is less than study done in Afar (72.53%) [14], Bahir Dar City (98%) [15], whereas in this study 6.02% of the participants used alcohol base sanitizer, which is in turn higher than study conducted at Bahir Dar City (2%) [16] And less than study done in Afar (27.47%) used alcohol based sanitizer. The discrepancy might be due to study methodology [14].
This study finding showed that hand washing practice immediately on arrival at work was 6.02%, it revealed that it is less than study done North-Western Nigeria hospital Only 14.5% comparable [14], whereas hand washing practice after the day’s work before leaving the hospital 80.12 it is higher than study done North-Western Nigeria hospital (72.8% ) [17].
In this study finding of hand washing practice after touching blood, body fluids, secretions 100%, other study showed that contact with patient’s body fluid was the most common reason (87.3%) for always washing hands. This is comparable with the findings of Kingston [17]. Other study showed that Hand washing rates dramatically improved after simple procedures. This shows that health workers were primarily concerned with protecting themselves from acquiring pathogenic organisms from their patients; rather than trying to prevent the occurrence and spread of nosocomial infections amongst patients admitted under their care.
Only twenty seven (16.27%) followed correct sequence in hand washing. Starting from Remove jewelry, turn on the tap, wet hands thoroughly under running water, Soap hands adequately, Rub hands vigorously front and back, in between fingers, finger tips, the sides of the hand, the thumbs, up to and including the wrists then Rinse under clean running water until all soap removed. It is less than study done in Nigeria (73.4%) [17]. Always followed the right sequence.
Shared ward towels drying was the preferred method of hand drying after washing which was seen in 66.87% of the participants it in line with more than half (72.0%) of the health workers were observed to dry their hands Common cotton towels [17]. This should be discouraged as it will result in further contamination of the hands of the health workers and encourage the spread of pathogenic organisms from one patient to the order.
Very poor practice with Hand washing practices among studied Health Care Workers is calling for urgent intervention. Implementing five movements of hand hygiene are the best method for preventing healthcare associated infections. Therefore, the health care provider should be followed this principle to fight healthcare associated infections.
Many constraints to hand washing existed in the hospital. The main constraints identified by the respondents were lack of water and/or lack of soap, as well as lack of alcohol hand rub. Provision of these hand sanitizers is important because basic hand hygiene is very important in preventing transmission of infection from one patient to another and from patient to health workers.
Frequent seminars should be organized by the Infection Prevention Committee to teach or remind them of the standard principles of hand hygiene. Written guidelines should be posted in well-known places to serve as a constant reminder. Washing agents should be made available more routinely. Disposable paper towels as well as ensuring constant water supply. The use of alcohol-based hand rubs would go a long way in improving hand hygiene because they are portable, hence easy to carry around; effective; and largely non-irritant. They can also be used in the absence of water supply. Health care workers should Endeavour to take their own hand towels to work to prevent the spread of infections via towels. At least two should be carried along so that the towel does not become unduly soaked.
The author would like to declare that no conflict of interests in this study.
The author would like to extend sincere thanks to Jugal hospital staffs and data collector (observer). The author would like to extend special thanks to Gizeshwork Mulugeta (Infection prevention committee head of the hospital) for her nice cooperation.
No funding to this research.
Citation: Jamie AH (2020) Hand Washing Practices among Health Care Workers in Jugal Hospital, Harar, Ethiopia, 2020: In the Era of Corona Virus: Observational Study. J AntivirAntiretrovir.12:197. DOI: 10.35248/1948-5964.20.12.197
Received: 18-Apr-2020 Accepted: 03-May-2020 Published: 08-May-2020 , DOI: 10.35248/1948-5964.20.12.197
Copyright: Jamie AH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : �???�???�???�???�???�?�¢??�???�?�¢??�???�???�???�?�¢??�???�?�¢??�???�??�?�© 2020 Jamie AH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.