Translational Medicine
Open Access
ISSN: 2161-1025
ISSN: 2161-1025
Review Article - (2023)Volume 13, Issue 1
The Herd immunity is very hot topic during this COVID-19 pandemic era for discussion among scientific community and researchers as well as peoples around the globe. Usually in common term it refers to a herd or group of people or a proportion of population immune to COVID-19 infection among individuals in a population. In other way researcher describe it as the threshold proportion of immune individuals (due to natural immunity or conferred through vaccination) in a population required to decline COVID-19 incidence of infection. Some researchers describe it as a pattern of immunity required to protect a population from invasion of a new infection. In simple words we can say that the chance of infection among susceptible individuals in a population is decreased by the presence and availability of more and more immune individuals which is referred as indirect protection or a herd effect for protection. In this study brief historical, epidemiologic, theoretical, and realistic public health perspectives on this model relevant to COVID-19 were discussed.
COVID-19; Herd immunity; Vaccination
Historically in a paper published by W.W. Topley et al. titled “The spread of bacterial infection: The problem of herd immunity” in 1923 the term herd immunity was first used [1]. In the current ongoing COVID-19 pandemic era the term “herd immunity” is widely used and discussed word in media and among researchers. The use of this term is particularly increased after introduction of COVID-19 vaccines and discussions about COVID-19 eradication, as well as economic evaluation about costs and benefits of COVID-19 vaccination programs.
Herd immunity' is sometimes referred as 'population immunity'. The WHO advocates achieving 'herd immunity' through vaccination, as this would avoid unnecessary mortality and morbidity while some researchers advocate it through acquisition of natural immunity. In this context theorem of Smith in 1970 [2] and Dietz in 1975 [3] of threshold states that if immunity (i.e., successful and effective vaccination) were delivered randomly and if members of a population is also mixing up randomly, such that on an average each single individual contacted R0 individuals in a manner enough to transmit the COVID-19 infection [4,5], then incidence of the COVID-19 infection would decrease if the proportion of immune exceeded (R0-1)/R0, or 1–1/R0. This is explained with Figures 1 and 2 and Table 1 below:
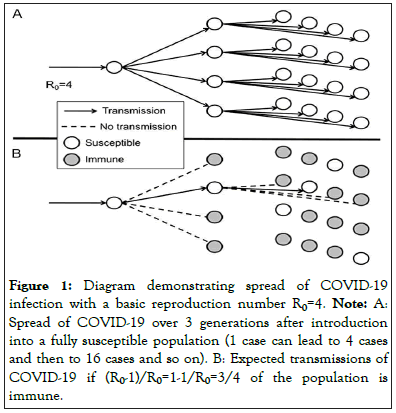
Figure 1: Diagram demonstrating spread of COVID-19 infection with a basic reproduction number R0=4. Note: A: Spread of COVID-19 over 3 generations after introduction into a fully susceptible population (1 case can lead to 4 cases and then to 16 cases and so on). B: Expected transmissions of COVID-19 if (R0-1)/R0=1-1/R0=3/4 of the population is immune.
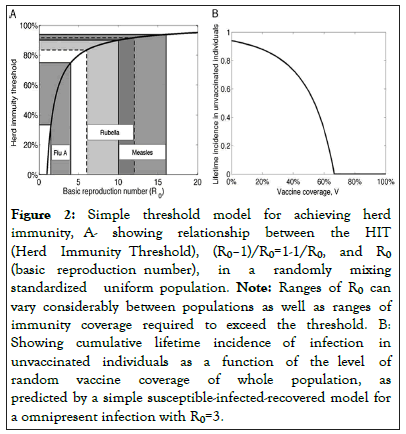
Figure 2: Simple threshold model for achieving herd immunity, A- showing relationship between the HIT (Herd Immunity Threshold), (R0–1)/R0=1-1/R0, and R0 (basic reproduction number), in a randomly mixing standardized uniform population. Note: Ranges of R0 can vary considerably between populations as well as ranges of immunity coverage required to exceed the threshold. B: Showing cumulative lifetime incidence of infection in unvaccinated individuals as a function of the level of random vaccine coverage of whole population, as predicted by a simple susceptible-infected-recovered model for a omnipresent infection with R0=3.
| Term | Symbolic Expression | Definition |
|---|---|---|
| Basic reproduction number |
R0 | Total Number of secondary cases generated by a single infectious COVID-19 individual when the rest of the population is susceptible (i.e., at the start of a novel COVID-19 outbreak) |
| Critical Vaccination level |
Vc | Proportion of the population that must be vaccinated to attain herd immunity threshold, pretentious that vaccination takes place at random |
| Vaccine effectiveness critical of transmission breakup |
E | Reduction in transmission of infection to and from vaccinated compared with unvaccinated control persons in the same population (similar to conventional vaccine efficacy but measuring protection against transmission rather than protection against disease |
Table 1: Symbolic expression for given the variables.
Under such circumstance (achieved through vaccination or natural immunity), all except 1 of the contacts for each case is immune, hence in this circumstances one case will leads to only 1 successful transmission of the infection; this will lead to constant incidence over time; if a greater proportion of the population is immune to COVID-19, then the incidence will decrease. On this calculation and basis, (R0-1)/R0 is known as the herd immunity threshold.
This assumes a 100% effective vaccine (E=1). Note that the probable growing incidence is 0 if coverage is maintained above Vc=1-1/R0=67% (Table 1).
Homogeneous mixing and simple thresholds have existed. In some papers it was found how to derive R0 for various infections, often implying that the 1-1/R0 threshold can be utilized as a set target for immunization coverage and that this achievement can lead to eradication of target (here COVID-19) infections [7].
Epidemiologic viewpoint
There are several examples of herd immunity demonstrating the significance of indirect protection through herd immunity for short-term and long-term effect of vaccination programs, for justifying vaccines economically, and for evaluating the immunity induced by various vaccines.
For example periodic epidemics of several global childhood infections like MMR (Measles, Mumps, Rubella,), DPT (Diphtheria, Pertussis, Tetanus) chickenpox, and polio, etc. happens sometime due to the accumulation of a critical number of susceptible individuals in populations and these outbreaks could be delayed or averted by vaccination through maintaining the numbers of susceptible individuals below this critical number (i.e. by keeping the proportion immune population above a calculated threshold) [8,9].
Another example of indirect protection was seen after the introduction of pneumococcal conjugate vaccines and haemophilus infections. Reductions in disease incidence among cohorts too old to be vaccinated was responsible for one to twothirds of the total disease decline attributable to these vaccines in some populations because of the ability of pneumococcal conjugate vaccines to defend not only against disease but also against nasal carriage, and hence infectiousness.
Selection and vaccination of population which are likely to play a key role in transmission (such as highly mobile workers, health care workers) can help in reducing transmission in general However in a published paper by Fox, et al 1971 [6]. it is suggested that simple thresholds was not enough for public health, due to the fact of population heterogeneity, belief of populations and this will reduce incidence among general population at risk of acquiring infection. Colleges, schools can play an important link in community transmission of COVID-19 viruses, and thus there have been decisions of reducing transmission either by closing schools or by vaccinating school children and college adults. One example is selective vaccination of children against influenza in Japan during the 1990s and was found to reduce morbidity and mortality among the elderly population [10].
The successful global eradication in the case of smallpox and rinderpest based on vaccine and at least regionally successful in the case of wild polio virus though the thresholds for herd immunity have proved the importance of achieving herd immunity. These programs have used a combination of routine vaccination added with campaigns in high-risk regions and populations in order to stop the final chains of transmission. This demonstrates how the direct effect of immunity in population (i.e., successful vaccination or through natural infection) can help in reducing infection or infectiousness in other individuals at risk of infection who are susceptible in the population. In this way a vaccine’s affects transmission causing the indirect protection. However if vaccine can prevent disease only but not alter either the risk of infection or infectiousness, then this indirect effect and herd immunity is impossible.
The extent of the indirect outcome of vaccine-derived immunity is decided by the transmissibility of the infectious causativeagent, the nature-strength of the immunity developed as a consequence of vaccination, the amount of mixing and infection transmission in community-populations, and the vaccination target distribution as well as immune status of the population. Here comes the main barrier of knowledge that is the naturestatus of immunity and the situation of population heterogeneity which usually makes prediction difficult to predict the HIT. For understanding of these effects we have to look after 3 factors: It includes
• The study reports and research experience of vaccines in different populations.
• The development of more developed techniques capable of finding heterogeneous mixing within populations.
• Sophisticated reliable analysis to measure indirect protection in the context of vaccine efficacy-effectiveness and observational-descriptive-analytic studies, by comparing the risk-difference/relative-risk of infection among individuals as a function of their vaccination status and of their household or village contacts.
Theoretical progress
Theoretically it is assumed that in the context of herd immunity that vaccines induce solid immunity against infection (which is not perfectly true as evidenced by breakthrough infections and morbidity-mortality data) and that populations mix at random, regular with the simple herd immunity threshold for random vaccination of Vc=(1-1/R0), using the symbol Vc for the significant least proportion to be vaccinated (considering 100% vaccine effectiveness). Several research has addressed this problem of imperfect immunity, heterogeneous populations, nonrandom vaccination, and ‘‘freeloaders’’ [11,12].
Imperfect immunity
From evidence of breakthrough infections and facts it’s clear that COVID-19 vaccination does not impart 100 percent solid immunity against infection to all vaccinated individuals, naturally the threshold limit of vaccination required to protect a increased population [13]. If vaccination protects only a fraction of population vaccinated then E among those vaccinated (E ranking for effectiveness against infection transmission, in the field trial), then the calculation for critical vaccination coverage level will be Vc=(1-1/R0)/E. We can see from this that if E is<(1-1/R0) it would be impossible to eliminate an infection even by vaccinating the whole population. At the same time, fading away of COVID-19 vaccine-induced immunity requires repeated levels of coverage or more booster vaccination [14]. For illustrations of this principle with example we know the shifts to multiple doses (up to 20) and to monovalent vaccines in India to eliminate polio, where the standard trivalent-oral polio vaccines and regimens produced low levels of protection [15].
Heterogeneous populations-nonrandom mixing
Working on heterogeneous populations needs deep knowledge or assumptions about how different groups interact with each other. The dynamics of infection transmission within and between each group depend upon the rate of acquisition of infection from all other groups and individuals within the group. In simple random models of study, all mixing behavior is captured by a single parameter, but in heterogeneous populations this must be replaced by different parameters to describe how each group interacts with other group. Here the barrier is evaluation of this contact matrix which may be quite impracticable, or impossible, and so approximations are usually done. The questionnaire studies although quite tough and expensive to carry out can collect better data about range of interactions between different age groups, allowing evidencebased study with parameterization of age-structured models with complex mixing . Spatially explicit models can be parameterized using transport data to know about dynamics of interaction. The mathematical models to describe this heterogeneous mixing are quite complex and difficult to understand and interpret by most researchers, the critical threshold remains: Vc=(1-1/R0)/E, except that R0 is no longer to be considered a simple function of the average number of contacts of individuals. Instead it’s true that R0 is a measure of the average number of secondary cases generated by a primary infectious person but at the same time it’s a fact that this average will depends upon how the various groups/individuals interacts and can be calculated from a composite-matrix describing how the infection spreads within and between groups. Usually the interactions are often observed to be more rapid within than between groups, in such case the most highly interacting groups will have more transmission, resulting in a higher value of R0, and a larger vaccination threshold (vast population and population density are very important factors) will be obtained by assuming that all individuals display average behavior.
Nonrandom vaccination implications
Usually the vaccination coverage differs between different (age) groups in a population, and these different groups differ in their risk behavior which simply results no longer follow up. To illustrate this fact, let us consider a population consisting of 2 groups, 1 high risk behaviour and 1 low risk behaviour, and let us suppose that one high-risk case infects 5 high-risk individuals and one low-risk case infects 1 low-risk individual. Here, R0=5, so Vc=80%. The high-risk group outbreaks could theoretically be prevented by vaccinating 80% of the high-risk group alone, thus, 80% of the entire population. Hence, if highly transmitting groups are preferentially vaccinated, lower values of coverage than calculated/predicted using random vaccination models will be sufficient to protect the entire population. Nonrandom vaccination may be for more cost-effective interventions but at the same time it raises problems in practice. If those at greatest risk are the least likely to be vaccinated then extra resources are required to ensure sufficient coverage. Added to this nonrandom vaccination can be ineffective even in a behaviorally homogeneous population because it may results in clusters of unvaccinated individuals; such groups/clusters are quite vulnerable to outbreaks. Clusters may emerge because of spatial vaccination as well as because of social segregation. Social clustering of parents who will not to vaccinate their children can result in clusters of children in which vaccination levels are quite below the herd immunity threshold. The same effect can be found in religious communities that avoid vaccination; even if they form only a small fraction of the population, usually they often mix selectively with other members of the same community hence they are at an elevated risk of infection.
''Freeloaders'' taking advantage of others' generosity without paying anything in return. COVID-19 vaccination has costs (also provided free by several governments) to the individual—adverse effects, time, and money, inconvenience etc. which affects an individual decisions about whether to be vaccinated or not vaccinated. As per health belief model constructs individual decision are based on a complex balancing of perceived susceptibility/severity/benefits/barriers/costs of vaccination and disease. Theoretically a high level of vaccination in the community may mean that the chance of contracting an infection is close to 0 which is not perfectly true as stated above due to different factors. The strategy is that everyone should be directly protected by COVID-19 vaccination, allowing the exceptional freeloaders to be protected from the indirect protection. People are usually performing complex cost-benefit analyses, based on imperfect own assumptions (example a failure to appreciate the relationship between age and clinical severity of infections), when deciding whether or not to have themselves or their children vaccinated. It is not surprising that a sustained low incidence of infection, caused in large part by successful vaccination programs, makes the maintenance of high vaccination levels difficult, especially in the face of questioning or negative media attention.
Public health practice scenario
The theoretical description provides a useful background, but field/health managers of COVID-19 vaccination programs usually face several non-theoretical problems in attempting to vaccinate populations [16]. Public health managers usually concentrate over target thresholds for vaccination, as thresholds are based on theoretical assumptions that greatly simplify the complexity of actual populations. In most circumstances, the prescribed public health practice is to aim for 100% COVID-19 vaccination coverage, with all the doses (usually two) recommended. Well aware of the fact that 100% is never achievable due to several reasons mentioned above, hoping to reach the ‘‘real’’ herd immunity threshold in the population concerned is difficult due to fact that it’s difficult to calculate real HIT due to factors mentioned above. Monitoring of huge population coverage is itself a problem. Managers are usually not confident of the immunity coverage actually attained, because of avoidance of vaccine by some population subsets, ineffective or poorly administered vaccine, vaccination missing the recommended schedule, delays and inaccurate (sometimes even fabricated/falsified) data, as well as population migrations, private sector vaccine providers, if they do not provide data to national statistics. Another difficulty is raised by campaigns, against COVID-19 vaccinations; missing data of numbers of doses administered, multiple (unnecessary) vaccinations, whereas others are repeatedly left out. Sound knowledge of population statistics is a requirement for sound policy for vaccination coverage. Maintenance of high coverage is particularly difficult because the COVID-19 diseases decline in frequency in different seasons and as populations become more aware they are more likely to question evidence-facts-recommendations. This leads to growth of anti-vaccine sentiment in many societies which is a complicated issue, whether based on religious-libertarian philosophies, or frank misinformation/rumors (of which there is an increasing amount, readily/widely available on the internet media). The recent global pandemic of COVID-19 is the latest in a long list of examples of the constraints of maintaining high vaccine coverage and to convey the appropriate message for the public. Added to this herd immunity is not the same as biologic (immunologic) immunity; individuals saved only by indirect herd effects are fully susceptible to infection if they ever be exposed. This has advantages, in protecting individuals with absolute contraindications to vaccination or those who for any other reasons miss vaccination, but it also has its disadvantages. Outbreaks among universities etc., are among examples of the consequences of clusters of susceptible individuals who have not been protected by vaccination, and escaped infection because of a herd immunity effect earlier in timeline. Infection later in life may cause more serious disease due to development of comorbidities like diabetes, hypertension etc., which has most severe consequences. This clearly outlines that there is a need for immunization programs to maintain high vaccine coverage, together with supportive surveillance and outbreak response capabilities, as numbers of vulnerable individuals accumulate in older age groups. Herd immunity usually implies a lasting programmatic responsibility to the public health managers.
Usually COVID-19 eradication and control strategies aim at protecting the maximum number of individuals at risk, typically with a combination of high vaccination coverage and additional targeted vaccination of high risk populations. These strategies require timely knowledge of population/places where transmission is occurring, and thus surveillance is critical. COVID-19 vaccination mass campaigns for eradication and containment are costly and require detailed planning to reduce cost. These are massive routine regular logistic undertakings, often implying severe disruption to routine health services like RCH programmes. These activities have engendered considerable antipathy in some populations and should be rectified timely. COVID-19 vaccination can be made more costeffective if we have better tools to determine immunity levels and to understand transmission dynamics. It is important to understand the fact that models are just tautologies of their assumptions, and sound field epidemiological research study is essential to provide appropriate data on which to base these assumptions. Finally, there are ethical and legal constraints of herd protection. In so far as encouraging vaccination as a method, to provide indirect protection to unvaccinated individuals, have risk implications-albeit a very small risks-being imposed on few individuals for the benefit of other individuals.
HIT approach has implications and limitations as discussed above-different in different cultural, ethical, or legal contexts-for government liability in circumstances of adverse events to vaccines. Viewed from this perspective I find that indirect protection based on ‘‘herd immunity,’’ raises many critical and important issues as well as problems about implementation, individual and public values. Indeed, we can say that herd immunity, in the final analysis, is about protecting society by the society.
This paper has not been previously published by any peerreviewed journal. The document is Microsoft word with English (United States) language & 3251(excluding declaration and reference) words total.
Ethics approval and consent to participate
Not applicable. This study has not involved any human or animals in real or for experiments.
Consent for publication
Not applicable
Availability of data and materials
The data and materials for study are mentioned in article and available as reference.
Conflicts of interest
There are no conflicts/competing of interest.
Funding
Self-sponsored, No aid taken from individual or agency etc.
Author contributions
The whole work is solely done by the author, Dr Piyush Kumar, M.B.B.S., Sri Krishna Medical College, EMOC- General Medical Officer- Bihar Health Services; Government of Bihar, India and Advocate Anupama.
Acknowledgement
I am thankful to Advocate Anupama my wife and my daughters Aathmika, Atheeva for cooperation.
Author information
The author is currently working as Senior Medical Officer for the government of Bihar, India.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kumar P, Anupama (2023) Herd Immunity and COVID-19 Vaccines- A Brief Discussion. Trans Med. 13:281.
Received: 27-Feb-2023, Manuscript No. TMCR-23-21225; Editor assigned: 01-Mar-2023, Pre QC No. TMCR-23-21225 (PQ); Reviewed: 15-Mar-2023, QC No. TMCR-23-21225; Revised: 22-Mar-2023, Manuscript No. TMCR-23-21225 (R); Published: 30-Mar-2023 , DOI: 10.35248/2161-1025.23.13.281
Copyright: © 2023 Kumar P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.