Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research - (2023)Volume 12, Issue 12
Introduction and Hypothesis: POP (pelvic organ prolapse) and anti-UI (urinary incontinence) surgery are performed to restore the function of the female pelvic floor. The study aims to determine the effectiveness of the electromagnetic muscle stimulation (HIFEM) procedure as a form of postoperative pelvic floor physiotherapy on women who have undergone POP and anti-UI surgery.
Methods: Fifty females received a total of six HIFEM procedures scheduled twice a week over three weeks with follow-up visits after the last treatment and at 3 and 6 months. BFLUTS-SF questionnaire was used to evaluate UI and quality of life (QOL) before and after treatments.
Results: The mean pre-treatment combined score was 17.4±1.5 points. The score decreased significantly (p<0.001) at 3 and 6 months to 11.9±1.5 (-5.5 points) and 12.6±1.7 (-4.8 points), respectively. The women with three or more childbirths had significantly better improvement in average BFLUTS-SF score (-7.0 points) compared to women with a maximum of two deliveries (-4.4 points) at 3 months, when the results peaked. Overall, the results were not associated with the severity of the prolapse, and the most prominent changes were seen in the Incontinence, Filling, and QoL domains.
Conclusions: The data indicate that the HIFEM procedure significantly reduces the severity of lower urinary tract symptoms including UI while improving the QoL in subjects with persistent post-surgery incontinence.
Anti-urinary incontinence surgery, Pelvic floor muscles, Pelvic floor dysfunction, Pelvic organ prolapse surgery
Pelvic organ prolapse (POP) is defined as a downward descent of female pelvic organs, including the bladder, uterus, or posthysterectomy vaginal cuff, and the small or large bowel, resulting in a protrusion of the vagina, uterus, or both [1-5]. Its development is multifactorial, mainly characterized by the loss of some of the supportive mechanisms of the pelvic floor (e.g. pelvic floor muscle dysfunction), most often due to vaginal childbirth, advancing age, physical exertion e.g. lifting of heavy things or cough (from chronic obstructive pulmonary disease), or increasing body-mass index [6,7]. It is estimated that approximately 50% of all parous women suffer from varying stages of POP with the lower genital, urinary, and gastrointestinal tract symptoms that can affect a woman’s daily activities and quality of life [8-12].
Accompanying POP, the pelvic floor muscle (PFM) dysfunction, also results in urinary incontinence (UI), especially stress urinary incontinence (SUI), which is a very common condition occurring before or with the POP [13,14]. POP and anti-UI surgery remain the mainstay of treatment for these both disorders [15]. In order to prevent the persistence of UI symptoms after POP surgery and to improve the overall health and function of the pelvic floor, there is a need to strengthen the weakened PFM [16, 17].
The function of weakened PFM can be effectively enhanced by non-invasive electromagnetic muscle stimulation (HIFEM) procedures. As a well-established technology, HIFEM induces brain-independent supramaximal contractions of PFM using an electromagnetic field, selectively targeting only the striated muscles of interest [18, 19]. The previous studies were primarily focused on the non-invasive treatment of UI and sexual dysfunction or comparison between Kegel’s exercise and the HIFEM procedure [20–22]. The aim of this study is to determine the effectiveness and safety of the HIFEM procedure as a form of postoperative pelvic floor physiotherapy, and as a treatment of persistent UI in women post POP and anti-UI surgery.
Study Requirements and Ethical Considerations
The enrolment process in this study considered adult female subjects suffering from UI (either SUI, UUI, or MUI). Inclusion criteria for participation were as follows: female aged 35-80 years, a medical history of POP or anti-UI surgery or both, willing and able to abstain from partaking in any treatment of UI followed by a two-week wash-out period from any UI treatment before the start of the study. The severity of POP was assessed according to the grades: 0= No prolapse, I = the most distal portion of the prolapse is >1 cm above the level of the hymen, II = the most distal portion of the prolapse is ≤1 cm proximal or distal to the hymen, III = the most distal portion of the prolapse is >1 cm below the hymen but protrudes no further than 2 cm less than the total vaginal length, IV = complete eversion of the total length of the vagina, the distal portion protrudes at least the total vaginal length -2 cm beyond the hymen.
The subjects meeting any of the following criteria were excluded from participation in the study: suffering from other types of urinary incontinence other than SUI, UUI, MUI, currently lactating, cardiac pacemakers, implanted defibrillators and/or neurostimulators, electronic implants, metal implants, including copper IUD, drug pumps, hemorrhagic conditions, anticoagulation therapy, fever, pregnancy, following recent surgical procedures when muscle contraction may disrupt the healing process, application over areas of the skin which lack normal sensation, and any disorders that would interfere with study endpoints or subject safety.
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to. All patients signed study participation consent and informed treatment consent. The authors and staff have prior research experience and have completed and been certified in the GCP (Good Clinical Practice) program.
Treatment Protocol
This is a prospective single-center open-label one-arm study. Subjects were recruited from the existing pool of the Investigator’s patients and received the treatments at the principal investigator’s site. There was no randomization. All subjects received six 28-minute treatments delivered twice a week with EMSELLA (BTL Industries Inc., Boston, MA) device using the HIFEM procedure. A fully clothed patient sat straight in the center of the chair applicator, just above the stimulation coil which generates a magnetic field of 2.5 Tesla and provides electromagnetic stimulation of pelvic floor muscles. Treatment stimulation intensity was gradually increased on a scale of 0-100% according to the patient’s comfort. Patients were asked to report any sign of pain or discomfort during therapies and after each treatment session, they were examined for possible adverse events or side effects in the treated area. In order to observe long-term results in POP and anti-UI surgery patients, subjects were required to complete three follow-up visits (after the last treatment and at 3- and 6-month follow-up).
Main Outcomes Evaluation and Statistical Methods
To assess the patients’ condition throughout the study, the Bristol Female Lower Urinary Tract Symptoms – Short Form Questionnaire (BFLUTS-SF) was administered at baseline and at all follow-up visits. The BFLUTS-SF included questions relating to incontinence, other lower urinary tract symptoms, sexual matters, and quality of life, constituting domains: Filling, Voiding, Incontinence, Sex, and Quality of Life [23, 24]. The data analysis was performed using Microsoft Excel and Real Statistics Resource Pack add-in [25]. The descriptive statistic was calculated (mean, standard error of the mean) and all data were analyzed for normality. Based on the paired and independent variables measured at multiple time points, parametric tests (paired T-test, One-way Repeated measures ANOVA) were used. The significance level was set to α=0.05 (5%). For safety measurements, the adverse events and side effects were monitored during all treatment sessions and follow-up visits.
Fifty women (36-79 years, BMI=28.5 ± 0.9 kg/m2) meeting the inclusion and exclusion criteria were enrolled in this study as shown in Figure 1.
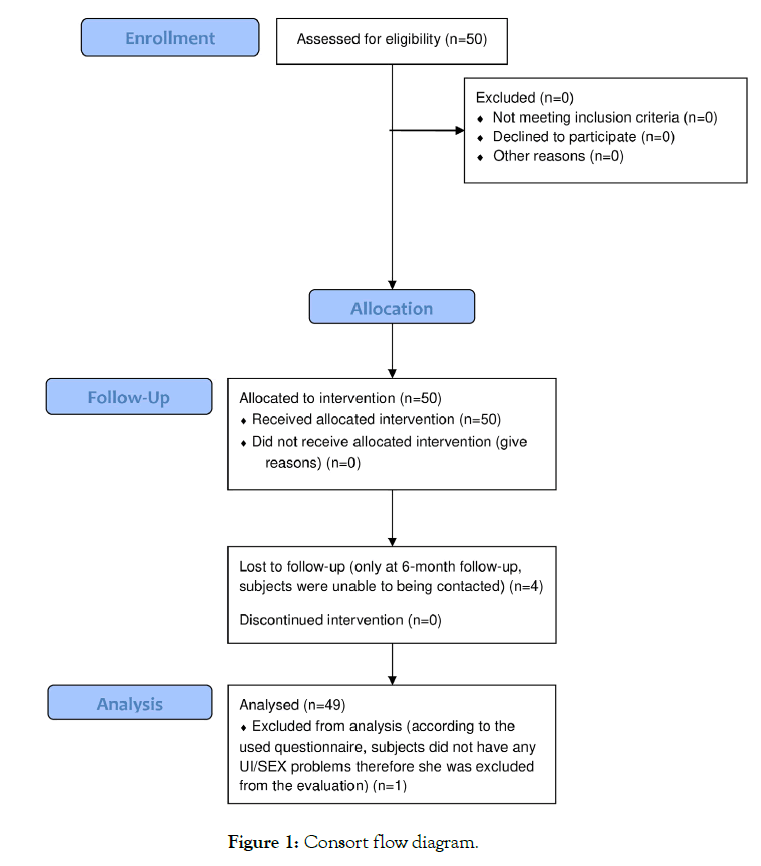
Figure 1. Consort flow diagram.
One patient did not adhere to the inclusion criteria throughout the study thus her data were not included in the evaluation. Based on the demographic data, the patients (N=49) were further divided into subgroups according to the number of deliveries (up to 2 or 3 and more) and the overall stage of prolapse and cystocele condition (major stage III or greater cystocele and prolapse, and minor stage II or less cystocele and prolapse) as documented in Table 1.
| Group | Number of deliveries | POP and cystocele stage | ||
|---|---|---|---|---|
| Up to 2 | 3 and more | Minor (II) | Major (III) | |
| N (group) | 28 | 21 | 23 | 26 |
| Age | 59.6 ± 2.3 | 61.3 ± 2.8 | 55.5 ± 2.7 | 64.7 ± 2.0 |
| POP surgery | 28 | 20 | 22 | 26 |
| Anti-UI surgery | 28 | 21 | 23 | 26 |
| Vaginal delivery | 1.4 ± 0.2 | 3.4 ± 0.3 | 2.2 ± 0.3 | 2.3 ± 0.3 |
| C-section | 0.3 ± 0.1 | 0.2 ± 0.1 | 0.3 ± 0.2 | 0.2 ± 0.1 |
Table 1: Patients’ demographic information (count and mean ± SEM; SEM=standard error of the mean), divided according to the number of deliveries (up to 2 or 3 and more) and the overall stage of prolapse and cystocele condition.
For all patients, the average combined BFLUTS-SF score significantly (P<0.001) decreased from the baseline value of 17.4 ± 1.5 points to 12.1 ± 1.5 points after the treatments and 11.9 ± 1.5 points at the 3-month follow-up visit. The improvement was significantly (P<0.001) maintained to the 6 months at 12.6 ± 1.7 points while showing a slight relapse shown in Figure 2.
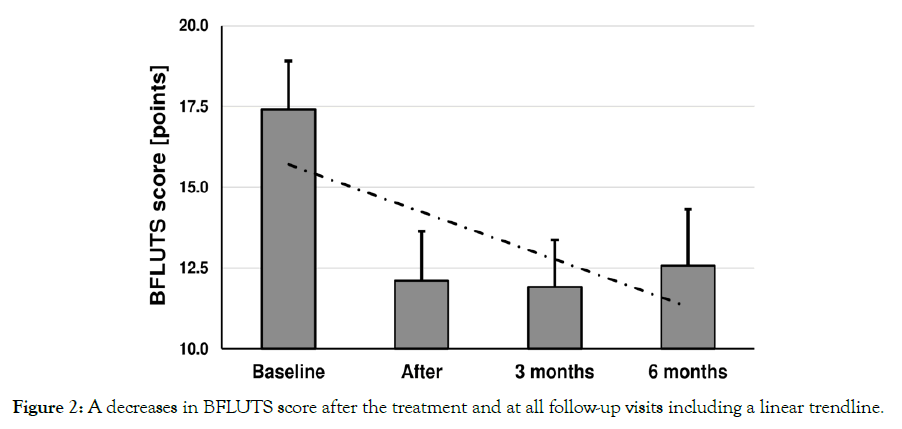
Figure 2. A decreases in BFLUTS score after the treatment and at all follow-up visits including a linear trendline.
In absolute numbers, the greatest decrease was observed in the Incontinence domain (-2.0 points, p<0.001) and Filling domain (-1.4 points, p<0.001) at six months and QoL domain at three months (-1.5 points, p<0.05). Interestingly, at 6 months there was a noticeable increase in the QOL domain score suggesting that individual decline of results may be bothersome to subjects and propagates to their everyday life substantially since on average, the improvement seen in the other individual domains remained essentially unchanged Table 2. When comparing the groups according to the parity, it was found that especially at 3 and 6 months there was noticeably greater improvement in combined overall BFLUTS score in subjects with 3 and more deliveries than in the group with up to 2 deliveries. Women with 3 and more deliveries showed a reduction of -7.0 points (p<0.001) and -5.7 points compared to -4.4 points and -4.2 points in the second group (p<0.05) at 3 and 6 months. This difference was primarily attributed to greater enhancement in Incontinence, Filling, and QOL domains.
| Baseline | After | Difference | 3 months | Difference | 6 months | Difference | |
|---|---|---|---|---|---|---|---|
| Filling | 5.1 ± 0.5 | 3.7 ± 0.4 | -1.4 | 4.1 ± 0.4 | -1 | 3.7 ± 0.4 | -1.4 |
| Voiding | 1.9 ± 0.3 | 1.6 ± 0.3 | -0.3 | 1.2 ± 0.2 | -0.7 | 1.1 ± 0.3 | -0.8 |
| Incontinence | 4.9 ± 0.7 | 3.0 ± 0.6 | -1.9 | 3.0 ± 0.6 | -1.9 | 2.8 ± 0.7 | -2 |
| Sex | 0.9 ± 0.2 | 0.5 ± 0.2 | -0.3 | 0.4 ± 0.2 | -0.4 | 0.1 ± 0.1 | -0.8 |
| QOL | 4.7 ± 0.6 | 3.4 ± 0.6 | -1.3 | 3.2 ± 0.5 | -1.5 | 4.0 ± 0.6 | -0.8 |
| SUM | 17.4 ± 1.5 | 12.1 ± 1.5 | -5.3 | 11.9 ± 1.5 | -5.5 | 12.6 ± 1.7 | -4.8 |
Table 2: Average scores (mean ± standard error of the mean) in the BFLUTS-SF domains and their point differences against the baseline.
In addition, there was also a significant improvement in the Major-POP and Minor-POP subgroups regardless of the severity of prolapse (p<0.05). The combined score showed that patients from the Minor POP group achieved a higher baseline score (19.0 ± 2.2 points) than the Major POP group (16.0 ± 2.1 points). However, the relative improvement for both groups was essentially the same, averaging around approximately 30% (-4.7 points for Major group; -5.7 points for Minor group). Analysis of the questionnaire domains revealed that Major POP group achieved substantially greater improvement in Filling, Voiding, and Incontinence domains and the Minor POP group has better outcomes in Sex and QOL domains. Interestingly, there was almost no relapse seen in the Major POP group. No adverse events or no side effects were not observed.
Based on the BFLUTS-SF results, the impact of lower urinary tract symptoms was significantly alleviated after the HIFEM procedure in female patients post-POP and anti-UI surgery. There were no adverse events or side effects. The most prominent improvement was in the QOL domain at 3 months and at the Filling and Incontinence domain at 6 months. On the other hand, the relapse in QOL domain seen at 6 months suggests that individual decline of results may be bothersome to subjects, propagating substantially to their everyday life and influencing their wellbeing, although on average the improvement seen in the other individual domains remained essentially unchanged.
Further, it was found that there was greater improvement in the combined BFLUTS score in subjects with 3 and more deliveries. Studies by DeLancey et al. [26] and Leijonhufvud et al. [27] found that women who underwent vaginal childbirth had more damaged PFM and increased risk of genitourinary tract disorders, in comparison to the women who did not give childbirth or underwent cesarean section. Hypothetically, it may be more challenging to achieve superior results in subjects who experienced multiple deliveries. Nonetheless, the group with 3 and more deliveries shows greater improvement rates in this study, supposedly due to their more severe baseline condition of PFM dysfunction thus providing a higher potential for favorable outcomes after HIFEM treatment. In addition, there was a significant (p<0.05) improvement in both Major and Minor POP subjects showing that the HIFEM procedure can help to improve pelvic floor function regardless of the severity of prolapse. It corresponds with findings evidenced by Silantyeva et al. [18, 19] that the HIFEM procedure is able to restore PFM integrity by inducing supramaximal contraction and increasing its activity and endurance.
Based on the research of Hlavinka et al. [28] and Samuels et al. [29] the HIFEM treatment also effectively improves sexual function as seen in this study as well. Although the Sex domain did not show such high changes as Filling or Incontinence domains in absolute numbers, it still achieved a remarkable decrease in a score when gradually reduced from average 0.9 points to 0.1 points at 6 months, being the most progressive change relatively, in contrast to rest of the domains.
One of the greatest limitations of this study was that it relies only on the use of one pre-selected questionnaire, narrowing the focus of the results to a specific evaluation of the study group. In future studies, the design should include multiple means of evaluation or questionnaires to further investigate the impact of HIFEM treatment in subjects post-POP and post-UI surgery, especially with regards to their QOL. Another limitation in such studies can also arise from an insufficient follow-up on POP and anti-UI surgery, which should be considered during patient recruitment. Borstadt et al. [30] and Lensen et al. [7] concluded that anti-UI surgery should be provided minimally 3 months apart from the POP surgery due to the possibility of the disappearance of UI symptoms after POP surgery itself. In addition, subjects in this study (by design) underwent both types of corrective procedures prior to the HIFEM treatment, which restrain us from inferring the magnitude of its effect in subjects after POP or anti-UI surgery alone. Hereafter, it would be interesting to investigate the effects of the HIFEM procedure in subjects who underwent only one corrective surgery of the pelvic floor, elaborating on the results of this underlying study.
The HIFEM procedure is safe and significantly reduces the UI and severity of lower urinary tract symptoms associated with POP and anti-UI surgery in multiparous women. The observed changes accompanied by a noticeable increase in QOL were seen in the whole study group regardless of the severity of POP. The magnitude of achieved improvement is likely to be greater for multiparous women with markedly deconditioned pelvic floor musculature. Also the use of the BFLUTS-SF questionnaire, as a valid and publicly known questionnaire is beneficial. The results can be easily compared to other studies showing the position of the HIFEM procedure amongst current treatments. The main outcome of this study is to offer an effective and non-invasive viable option for women seeking the treatment of persisting UI after POP or/ and anti-UI surgery.
None.
None.
The data were properly anonymized and informed consent was obtained from all patients at the time of original data collection, and therefore no IRB approval is needed.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: Singhal D, Gopal M (2023) HIFEM procedure for Treatment of Persistent Urinary Incontinence Post-Pelvic Organ Prolapse and Anti-Incontinence Surgery. 12(12):701.
Received: 28-Nov-2023, Manuscript No. 28229; Editor assigned: 30-Nov-2023, Pre QC No. 28229; Reviewed: 15-Dec-2023, QC No. 28229; Revised: 21-Dec-2023, Manuscript No. 28229; Published: 27-Dec-2023 , DOI: 10.35248/2167-0420.23.12.701
Copyright: © 2023 Singhal D & Gopal M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited