
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2021)Volume 11, Issue 3
One of the most popular cleaning and disinfecting agents used worldwide is household bleach, typically containing sodium hypochlorite. When sodium hypochlorite is combined with either an acid or ammonia, irritant gases such as chlorine and chloramine, respectively, are formed. Chlorine gas can be very toxic and result in a myriad of mucosal and pulmonary symptoms. Although most effects are self-limited, we report a case of acute respiratory distress syndrome (ARDS), and eventual death, related to a household cleaner exposure. This case report emphasizes the importance of public health awareness and utilization of in-home protection strategies when using bleach-containing products, as well as reviews management options in patients presenting with chlorine gas toxicity.
Chlorine; Inhalation injury; ARDS
Environmental cleaning is one of the recommended methods to reduce transmission of deadly germs among individuals. With recent emergence of coronavirus-19, household cleaning has been paramount. One of the most popular cleaning and disinfecting agents used worldwide is household bleach, with the active ingredient sodium hypochlorite. Likely due to its widespread use and presence in various formulations, chlorine is also one of the most common substances involved in chemical-related injuries, with an estimated 9000 calls occurring to U.S. Poison control centers annually for chlorine-related exposures [1]. Chlorine gas is a known pulmonary irritant that cause a myriad of symptoms dependent on the time of exposure and concentration of the gas [2]. Its toxicity is due to the creation of hydrochloric acid and hypochlorous acid, along with reactive oxygen species, when chlorine gas comes in contact with the moist membranes of the respiratory tract [3]. The extent of airway damage ranges from bronchospasm to respiratory failure [4]. Although most effects are self-limited, we report a case of Acute Respiratory Distress Syndrome (ARDS), and eventual death, related to a household chemical exposure.
A 50-year-old male with a pertinent history of chronic obstructive pulmonary disease, smoking, diabetes type II, chronic kidney disease, and hypertension presented with respiratory distress after accidentally inhaling household chemicals, including bleach, while cleaning his apartment. He was brought in by EMS on 2 liters of nasal cannula, with saturations in the 70% range. Upon arrival to the resuscitation bay, a strong smell of chlorine was noted. Physical exam was notable for nasal secretions, increased heart rate, tachypnea, bilateral rhonchi, mild accessory muscle use and GCS of 15. His clothes were immediately removed and he was placed on a nonrebreather (NRB) followed by non-invasive positive pressure ventilation via BiPAP with improvement of his oxygen saturation level to 96%.
Labs were drawn and poison control was consulted, recommending topical decontamination and chest x-ray. Patient’s saturations began to decline so an awake nasopharyngeal scope was performed using Midazolam 1mg and Ketamine 20mg aliquots to maintain respiratory drive while assess for airway edema and damage. Copious frothy secretions were noted so atropine was given. Due to hypoxia to 80% during the procedure, a 6-0 endotracheal tube (ETT) was passed via nasotracheal but failed due to patient coughing. Albuterol, ipratropium, and a dose of atropine were given and patient was resumed on BIPAP.
Despite BIPAP, patient’s oxygen saturation remained in upper 80% so rapid sequence intubation was initiated with intubation on first pass on first pass with video-assisted laryngoscopy, confirmed with the ETT visualized going through the vocal cords, capnography, breath sounds, and chest x-ray, although R main bronchus intubation was not noted on portable viewing in critical care room (Figure 1).
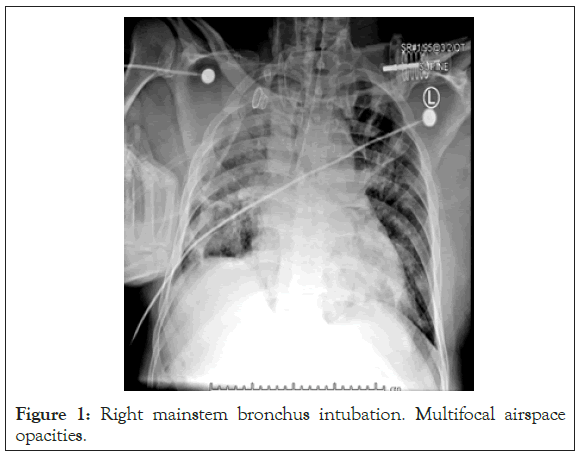
Figure 1: Right mainstem bronchus intubation. Multifocal airspace opacities.
Three minutes after ventilatory support patient’s oxygenation decreased to 80%. Pink frothy sputum was noted in ET tube. Despite disconnection from vent, bagging and copious suctioning, saturation did not improve. Repeat chest x-ray was performed (Figure 2), concerning for ARDS, pulmonary edema and R main bronchus intubation which was corrected without improvement. Repeat chest x-ray showed worsening ARDS despite our medical efforts (Figure 3). As a result of bedside literature review recommendations, solumedrol was given; and toxicology, medical intensive care unit and cardiothoracic surgery (CT) were consulted for consideration of Extracorporeal Membrane Oxygenation (ECMO).
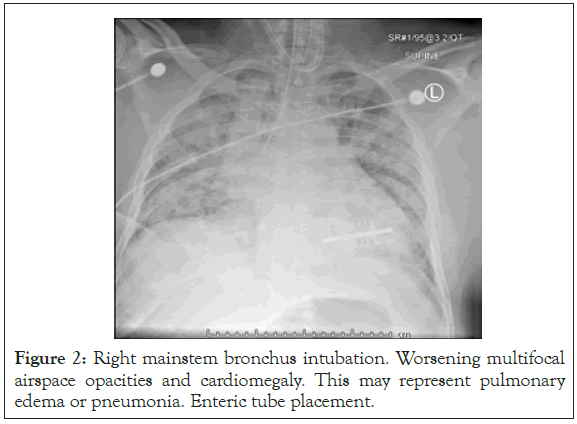
Figure 2: Right mainstem bronchus intubation. Worsening multifocal airspace opacities and cardiomegaly. This may represent pulmonary edema or pneumonia. Enteric tube placement.
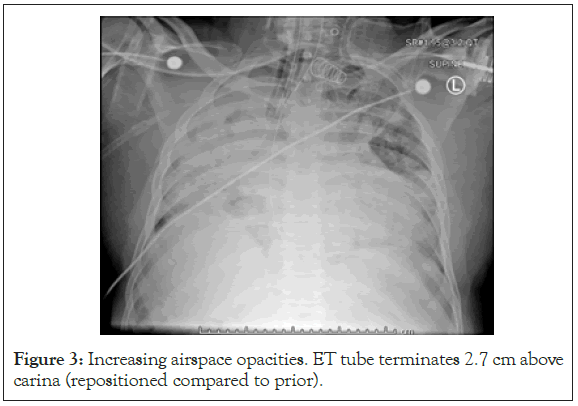
Figure 3: Increasing airspace opacities. ET tube terminates 2.7 cm above carina (repositioned compared to prior).
Toxicology and CT surgery team arrived at bedside to evaluate patient. After their evaluation, the patient became bradycardic, hypoxic (oxygen saturation level <55%), hypotensive and lost pulses. Advanced cardiac life support (ACLS) was initiated. Return of spontaneous circulation (ROSC) was achieved after 5 minutes of ACLS accompanied by IV epinephrine, calcium, and bicarbonate. Labs were notable for acidosis and acute on chronic CKD. CT surgery deemed patient a nonqualifying candidate for ECMO. Oxygen saturation ranged from 50%-60% with heart rate in 40s, resulting in initiation of transcutaneous pacing, epinephrine drip and nebulized bicarbonate for anecdotal treatment of chlorine gas inhalation. Despite efforts, patient lost pulses and was deemed expired after 30 minutes of ACLS accompanied by multiple boluses of calcium, epinephrine and bicarbonate.
Chlorine is one of the most common substances involved in chemical-related injuries, with exposure to chlorine gas occurring in association with swimming pool disinfection or the accidental combination of bleach and acid cleaning solutions in homes [1,5]. The combination of bleach with acid forms chlorine gas reacts with mucosal water to form hydrochloric and hypochlorous acid, along with reactive oxygen species [6]. Given its intermittent water solubility, symptoms are initially mild but can worsen over several hours. Another common reaction is the mixture of bleach and ammonia (or ammonia-containing substances), which forms the more water-soluble chloramine that liberates hypochlorous acid and hydrochloric acid. Given their increased water solubility, the symptoms are more immediate in onset and, due to the mucosal irritation; patients more readily remove themselves from the exposure. Based on this information, we believe that our patient was likely exposed to a combination of bleach and acid cleaning solutions.
The degree of injury is affected by many factors such as concentration of inhaled toxin, duration of exposure, ventilation of exposure location, and chlorine inhalation at toxic levels. In general, greater exposure dose, which is the product of the concentration of exposure and duration of exposure, is associated with greater potential harm. In addition to environmental and chemical properties, host factors such as extremes of age, tobacco abuse, and underlying lung disease contribute to worse outcomes [4]. Our patient had host factors (tobacco abuse, underlying lung disease) and environmental factors (small, poorly ventilated area) that both likely contributed to the severity of the patient’s symptoms.
Although most symptoms of chlorine intoxication are self-limited, exposure to high concentrations can prove dangerous [4]. The formation of hydrochloric and hypochlorous acids along with chlorine’s strong oxidizing potential results in the extraction of hydrogen from water, liberating oxygen free radicals that cause direct cellular injury [5]. As the pro-inflammatory cascade continues, interstitial edema develops, compromising the airways further. Signs and symptoms therefore reflect injury to mucus membranes and respiratory tract, resulting in lacrimation, rhinorrhea, conjunctival irritation, cough, and dyspnea. Common physical exam findings include tachycardia, tachypnea, wheezing, crackles (noncardiogenic pulmonary edema) and crepitation (associated with pneumomediastinum) [7]. Severe pulmonary toxicity resulting in life-threatening toxic pneumonitis, acute respiratory distress syndrome (ARDS), and respiratory failure is very rare [8].
Initial management includes airway management, stabilization and decontamination. After stabilization, the priority in acute exposures is decontamination, removing the person from the hazardous environment and decreasing contamination of healthcare workers [9]. In symptomatic patients, a baseline chest x-ray should be obtained and respiratory function should be monitored for at least 4-6 hours, including ABG and pulse oximetry [10]. As there is no specific antidote for chlorine intoxication, treatment of acute exposure targets relief of symptoms caused by bronchospasm and mucous membrane damage. Current therapies are based on reported experience, with therapeutic modalities including humidified oxygen, bronchodilation, aerosolized sodium bicarbonate, inhaled and intravenous corticosteroids, cough suppressants, intravenous furosemide, aminophylline, positive pressure ventilation, and mechanical ventilation if indicated [3,11]. If intubation is necessary, tidal volumes of 6 ml/kg are preferred, aiming to protect the lungs [4]. Beta-adrenergic receptor agonists and humified oxygen are the most commonly used agents in the emergency department, and are therefore accepted as first-line treatment [5]. Nebulized bicarbonate has been suggested as an anecdotal treatment in several case reports due to bicarbonate theoretically neutralizing the hydrochloric acid formed in the respiratory tract [12-14]. Recommended dose concentrations of nebulized bicarbonate are between 3.75%–4.25% [2]. The role of inhaled or systemic steroids is controversial given the risk of superimposed infection; however animal studies and a few case reports suggest improved mortality rates with increased use in acute chlorine exposure [8]. There is a twin case report in which the two patients had presumably similar exposures to chlorine. One received steroids and the other did not, and steroids showed some improvement in markers of pulmonary damage [6]. Additionally, some studies also mention antioxidants, such as ascorbic acid, and deferoxamine as adjunct therapies [15,16]. Lastly, extracorporeal blood purification is a last resort for intoxication management, with hemofiltration removing solutes by convection, attenuating excessive expression of systemic inflammatory mediators and restoring immune homeostasis [3]. Among direct causes of ARDS, chlorine gas inhalation injury is uncommon and can lead to serious respiratory failure. Majority of literature on the use of ECMO for refractory ARDS is directed towards viral illness such as Influenza and most notably COVID-19. However, there have been cases reports generated that demonstrate if the team is able to stabilize the patient in emergency room, ECMO may be the next best step in these patient's course. The ventilation-perfusion mismatch is what makes these patients inevitably difficult to manage once successful intubation occurs. More specifically, chlorine gas inhalation seems to cause a component of atelectasis that is in the dorsal distribution of the lung. These factors generate the refractory hypoxemia due to ventilation-perfusion mismatch. Prone positioning with ECMO may be of advantage given the pathophysiology of this process in which a ventilation-perfusion mismatch occurs. The combination of ECMO and prone positioning has been associated with an improvement in oxygenation and in chest X-ray findings while simultaneously being able to be performed safely [17]. Prone positioning during ECMO can be an effective approach to hasten the weaning of ECMO when atelectasis and ventilation-perfusion mis-match occur in a patient with severe ARDS induced by chlorine gas inhalation [18]. However, the aforementioned therapy was only looked at in case studies. Based on our literature review, no study to date has validated any of these treatments in randomized, controlled trials in humans, likely due to ethical limitation precluding such trials.
Chlorine gas is a known pulmonary irritant that causes a wide range of pathologic conditions, depending on the concentration and length of exposure as well as host factors. Acute Respiratory Distress Syndrome is a rare but fatal complication of chlorine inhalation. Our case reports ARDS, respiratory failure and death resulting from exposure to chlorine vapor/gas in a confined space, likely due to combining sodium hypochlorite with an acidic substance. Reasonably soon after presentation, he developed florid ARDS and serious difficulty oxygenating which led to a hypoxic arrest. From toxicology standpoint, chlorine was historically used as a war agent in WW1. When it comes into contact with mucous membranes, it reacts with water present there to form HCl and hypochlorous acid, and eventually reactive oxygen species. All pulmonary irritant chemicals are associated with ARDS and increased alveolar-capillary membrane permeability. Based on imaging, he had progressively worsening ARDS which fits with the exposure. Regarding treatment, the only options are removal from the source and supportive care, which in this case may be aggressive airway maneuvers/vent settings, bronchodilators and steroids. The only treatment not performed was ECMO. Further studies need to be done to delineate treatment options, dosing recommendations, and long-term effects, if any, for severe chlorine toxicity. Additionally, public health awareness and utilization of in- home protection strategies when using bleach-containing products is important to prevent future cases of accidental household chlorine inhalation injuries.
Citation: Turner A (2021) Household Bleach Leading to ARDS. J Clin Toxicol. 11:475.
Received: 10-Feb-2021 Accepted: 24-Feb-2021 Published: 02-Mar-2021 , DOI: 10.35248/2161-0495.21.11.475
Copyright: © 2021 Turner A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.