Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Research Article - (2024)Volume 15, Issue 7
This article explores the management of hypertriglyceridemia in infants undergoing congenital cardiac surgery, a topic with limited data. It introduces a structured protocol addressing pathophysiology and management strategies, emphasizing complications and management during congenital cardiac surgeries. We hope this article will serve as a reference for managing similar cases and for further research.
Hypertriglyceridemia; Cardiac surgery; Congenital heart disease; Plasmapheresis
LPL: Lipoprotein Lipase; GP1HBP1: Glycosyl Phosphatidylinositol Anchored High-Density Lipoprotein Binding Protein1; APOC-11: Apo Lipoprotein C-11; APO-AV: Apo Lipoprotein A-V: LMF 1: Lipase Maturation Factor-1; TGs: Triglycerides; APR: Acute Phase Reactants; HCT: Hematocrit; CPB: Cardiopulmonary Bypass; NFK: β-Nuclear Factor Kappa; ICAM-1: Intracellular Adhesion Molecule 1; MUF: Modified Ultrafiltration; AP: Acute Pancreatitis; MCT: Medium Chain Triglycerides; ANGPTL3: Angiopoietin-Related Protein 3; PAH: Pulmonary Arterial Hypertension; PVR: Pulmonary Vascular Resistance
• Avoid dehydration during fasting.
• Keep an additional CPB pump as stand-by.
• Maintain act>480 sec.
• Choose a higher-sized arterial and venous cannula to have as low as line pressure as possible.
• Monitor pre and post-membrane pressure on CPB.
• Monitor oxygenator and CPB reservoir for clots.
• NIRS monitoring for early identification of tissue hypoperfusion.
• Maintain normothermia or mild hypothermia.
• Maintain adequate hematocrit to prevent excessive viscosity decrease which can lead to a vasoplegic state and elevated hematocrit can increase viscosity.
• Maintain adequate urine output while avoiding excessive diuresis.
• Modified ultrafiltration with zero balance to maintain adequate dilution.
• Monitor for hemolysis and serum electrolytes, and increase in awareness to detect early hemolysis complication.
• Early identification of complications and imaging as serum levels of enzymes may be erroneous.
• If peritoneal dialysis is planned-use isodextrin.
• Consider early plasmapheresis for crisis.
In 1967, Fredrickson classified elevated lipoproteins into five types each requiring distinct management approaches [1]. However, there is limited data regarding hypertriglyceridemia in infants, especially within the scope of cardiac surgeries. Severe hypertriglyceridemia in infants is commonly attributed to lipoprotein lipase deficiency, often inherited in an autosomal recessive pattern. It is typically diagnosed incidentally during routine preoperative screening, where milky serum may be observed, or it may present acutely with signs of acute pancreatitis. This article introduces a novel, structured protocol addressing the pathophysiology and management strategies for elevated hypertriglyceridemia in infants undergoing cardiac surgery.
Hypertriglyceridemia can occur as either primary or secondary, with severe cases (2%) emerging in children often attributed to monogenic factors such as LPL deficiency, GP1HBP1 deficiency, APOC-11 deficiency, APO A-V deficiency and LMF1 deficiency. Conversely, in adults, it typically stems from polygenic causes. Recent years have seen an explosion of genetic insights through genome-wide association studies, uncovering over 300 distinct genetic loci associated with elevated triglycerides. Secondary causes encompass drug-induced, hypothyroidism, metabolic disorders, Chronic Kidney Disease (CKD) and Chronic Liver Disease (CLD) [2]. Children with Acyanotic congenital heart disease are often prescribed diuretics, which can increase triglyceride levels (Table 1) [3].
| Classification | Triglyceride levels (mg/dL) |
|---|---|
| Normal | <150 |
| Mild | 150-199 |
| Moderate | 200-299 |
| Severe | 1000-1999 |
| Very Severe | ≥ 2000 |
Table 1: Classification of hypertriglyceridemia.
Pathophysiology of hypertriglyceridemia
According to Hagenpoiseuilles law, elevated viscosity disrupts blood flow dynamics, leading to a reduction in blood flow rate. To counteract either an increase in blood pressure or vasodilatation should occur. Manifestation of symptoms often occurs when blood viscosity increases to three times the normal value, with a particularly pronounced impact on vessels measuring less than 30 μ in diameter.
Elevated levels of triglycerides initiate a cascade of physiological responses, increasing inflammatory markers and acute phase reactants, as well as an increase in free radicals and reactive oxygen species. These responses contribute to endothelial cell injury and dysfunction, impairing vasodilation and leading to microcirculatory dysfunction.
Both elevated triglyceride levels and increased blood viscosity exert negative effects on the rheological properties of red blood cells and exacerbate the inflammatory processes during cardiopulmonary bypass procedures in congenital cardiac surgery. Additionally, factors such as hypothermia, hemolysis, and cardiopulmonary bypass-induced inflammation can further complicate.
Severely elevated triglycerides can have deleterious effects on organs, and congenital cardiac surgeries involving cardiopulmonary bypass add further complexities (Figure 1).
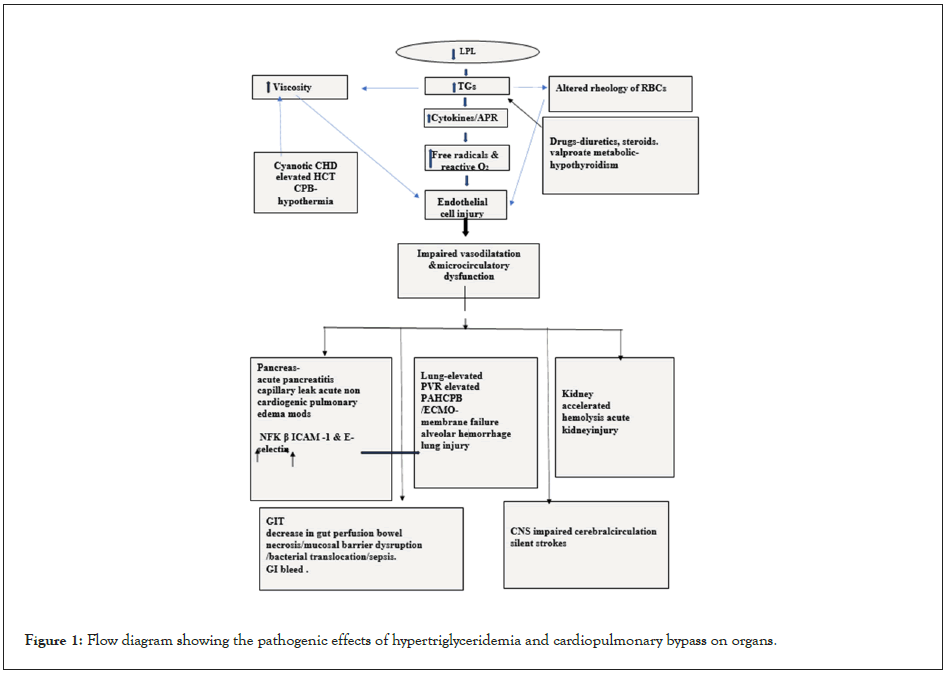
Figure 1: Flow diagram showing the pathogenic effects of hypertriglyceridemia and cardiopulmonary bypass on organs.
Pancreas
Elevated serum triglycerides and increased viscosity can induce microcirculatory dysfunction, and elevated intracellular calcium levels leading to pancreatic cell injury, ischemia, cellular acidosis, and activation of trypsinogen by Cathepsin B. Additionally, elevated fatty acids can contribute to acute pancreatitis. CPB- related complement activation, shear stress, and abnormal flow patterns can further complicate matters. The incidence of pancreatitis in congenital cardiac surgery is approximately 5%, with risk factors including prolonged perfusion and ischemia times, complex cardiac surgeries, and right-sided reconstructive procedures [4] .The incidence of acute pancreatitis rises to approximately 5% when triglyceride levels exceed 1000 mg/dl, and it escalates to 20% when levels surpass 2000 mg/dl [5] Diagnosis is often challenging, and unexplained hemodynamic instability, high-output cardiac failure, hypoxia, pulmonary edema of non- cardiac etiology, hypocalcemia should raise suspicion of pancreatitis. Spuriously low lipase and amylase levels in hypertriglyceridemia can be misleading, necessitating early imaging.
Lung
Severely elevated triglycerides can adhere to capillary walls, causing blockages and alveolar hemorrhages. This increases blood viscosity, impairing blood flow and tissue perfusion. Elevated triglycerides can worsen conditions like Pulmonary Arterial Hypertension (PAH) related to congenital cardiac lesions, as well as Acute Lung Injury (ALI) caused by Cardiopulmonary Bypass (CPB) or pancreatitis, which induces NF-kB, ICAM-1, and E-selectin, further contributing to lung injury. This exacerbates hypoxia and complicates the clinical condition [6,7].
Central nervous system
Increased viscosity can decrease regional cerebral blood flow and reduce wall shear stress in focal areas, potentially leading to silent strokes. Perioperative Near-Infrared Spectroscopy (NIRS) monitoring is recommended [8].
Gastrointestinal tract
Increased viscosity and chylomicron migration lead to compromised blood flow, which can result in bowel necrosis and gastrointestinal bleeding. A decrease in gut perfusion related to Cardiopulmonary Bypass (CPB), along with the use of high inotropic support and a breach in the gut mucosal barrier, can lead to bacterial translocation, causing sepsis [9].
Kidney
Microcirculatory changes, elevated inflammatory cytokines, and increased Intra-Abdominal Pressure (IAH) decrease glomerular filtration and increase hemolysis [10]. These factors, along with pancreatitis, can lead to an increased risk of perioperative acute kidney injury. It is essential to avoid nephrotoxic medications and maintain perfusion pressures on CPB appropriate to the age.
Management of hypertriglyceridemia
There is sparse literature about the effects of hypertriglyceridemia on congenital cardiac surgery, and only one case series by Yadav, et al., [11], has been documented in this age group. There is not much evidence to determine at what serum level of hypertriglyceridemia a case should be postponed, or at what level of serum triglycerides CPB membrane lung failure can occur. In the event of an emergency, postponement may be unavoidable. Understanding the effects of hypertriglyceridemia and its complex interactions during CPB will aid in developing better management strategies. Genetic analysis may not be useful in managing emergency surgery and should not delay the procedure. There is currently no evidence regarding perioperative infusion of octreotide and N-acetyl cysteine for the prevention of organ injury in severe hypertriglyceridemia during congenital cardiac surgeries, despite both having anti-inflammatory properties (Figure 2).
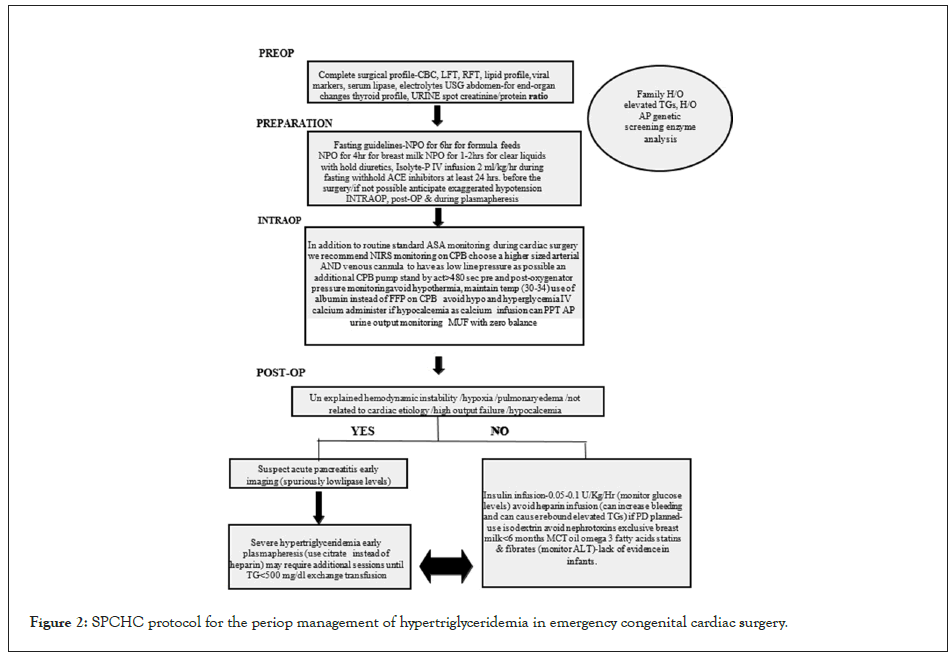
Figure 2: SPCHC protocol for the periop management of hypertriglyceridemia in emergency congenital cardiac surgery.
Interpret arterial waveforms with caution, as increased blood viscosity can disperse lower frequency components of the pulse waveform. This dispersion reduces the amplitude of the pulse wave, potentially causing damping effects [12].
Post-operatively, it is difficult to diagnose complications of hypertriglyceridemia, as the patient is often sedated or paralyzed on mechanical ventilation and the interpretation becomes challenging and can mask signs. Additionally, inflammation related to Cardiopulmonary Bypass (CPB) may mimic symptoms, and spuriously low levels of enzymes, CPB-related hemolysis, falsely elevated markers of hemolysis and hypocalcemia can give a false impression of routine post-congenital cardiac surgery course, it is difficult to interpret and should be interpreted cautiously, as these spurious changes can lead to mismanagement. We recommend continuing Near-Infrared Spectroscopy (NIRS) monitoring post-operatively for early detection of decrease in tissue perfusion. There should be a low threshold and meticulous monitoring to detect early signs of complications. Any signs of unexplained hypoxia, non-cardiogenic pulmonary edema, or hypocalcemia should raise suspicion and early imaging is recommended.
Postoperative low serum lipase, amylase and sodium levels, along with elevated markers of hemolysis, should be interpreted cautiously, as these spurious changes can lead to mismanagement.
Prefer albumin instead of Fresh Frozen Plasma (FFP) during Cardiopulmonary Bypass (CPB) or plasmapheresis. If peritoneal dialysis is planned, use isodextrin. In the event of a crisis, early initiation of plasmapheresis is beneficial, and exchange transfusion should also be considered if plasmapheresis in neonates/infants is not feasible. Administering insulin at 0.05- 0.1 units/kg/hr and dextrose to prevent hypoglycaemia can significantly activate lipoprotein lipase, which accelerates the degradation of triglycerides. Heparin, an activator of lipoprotein lipase, is not routinely recommended due to its increased risk of bleeding in post-op congenital cardiac surgeries.
Exclusive breastfeeding is recommended until infants reach six months of age, as fat is crucial for brain development during the first 12 months [13]. Completely avoiding fat may hinder their growth. Omega-3 fatty acids may be helpful, but evidence regarding MCT oil is conflicting, as some studies have shown that it elevates triglyceride levels. Fibrates and statins are not recommended in the infant group, and if initiated ALT/AST levels should be monitored.
Recent drugs
Research for newer drugs is ongoing with few successes in phase I trials. Gene therapy is of special interest where multiple approaches are tried. A summary has been provided in the Table 2.
| Mode of intervention | Types | Targets | Advantages | Disadvantages | Notable trials and results |
|---|---|---|---|---|---|
| Replacing diseased gene with a healthy copy | (a) Adeno associated virus mediated therapy | LDLR | Better efficiency lower side effects | Lower transfection efficiency long-term treatment might cause fat accumulation | Not significant |
| (b) Exosome mediated therapy | LDLR, PCSK9, ANGPTL3, APOC3 | Stable with good biocompatibility | Low yield and poor ability to transfer large RNAs | Phase 3 data with INCLISIR AN, targeting PCSK9 has shown 50% reduction in LDLC | |
| Inactivating a disease-causing gene | (a) Small interfering RNA (SiRNA) | Lipoprotein (a), PCSK9 | Higher specificity lower frequency of administration | In vivo easy degradation | OPALSIR AN, targeting Lp (a) showed an average reduction of 85% |
| (b) Antisense Oligonucleotides (ASO) | ANGPTL3, APOC3, Lp (a) | Higher specificity lower frequency of administration | In vivo easy degradation | Vupanorsen targeting ANGPTL3 showed dose-related reduction of total cholesterol reduction with a treatment duration of 4 weeks | |
| Introducing a new or modified gene for therapy | (a) CRISPR-Cas 9 | PCSK9, ANGPTL3 | Efficient and simple | Unpredict able off-target mutations | Ongoing animal trials |
| (b) Base editing | PCSK9 | No chromosomal translocation or off-target editing | Low operation efficiency | Mice trials underway | |
| (c) Meganuclease | PCSK9 | High specificity | Risk of off-target vector genome is unclear | Trials on rhesus monkey are ongoing |
Table 2: Short summary of recent drugs.
A Phase 1 trial demonstrated that evinacumab, a monoclonal antibody acting as an ANGPTL3 inhibitor, reduces triglyceride levels. However, it has not yet received FDA approval specifically for reducing triglycerides. FDA recommends its use for homozygous familial hypercholesterolemia, with a recommended dosage of 15 mg/kg IV once a week for four weeks [14].
Vupanorsen, an N-acetyl galactosamine-conjugated antisense drug targeting ANGPTL3 mRNA, demonstrates a reduction in triglycerides. However, it was discontinued during a phase 2b study.
Liver transplant
A liver transplant may be a possible option and Patients with homozygous familial hypercholesterolemia who do not respond to medical therapy may be candidates for liver transplant [15-17].
In conclusion, the management of hypertriglyceridemia and congenital hyperlipidemia poses significant challenges in clinical practice. While current treatment options such as lifestyle modifications, pharmacotherapy, and surgical interventions offer some relief, there remains a critical need for further research into novel therapeutic approaches. There should be a low threshold and meticulous monitoring to detect early signs of complications. Any signs of unexplained hypoxia, non-cardiogenic pulmonary edema, or hypocalcemia should raise suspicion, and early imaging is recommended.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Yadav MA, Trivedi D, Kasturi S, Reddy SN, Subramaniam G (2024) Hypertriglyceridemia in Infants during Congenital Cardiac Surgery: Pathophysiological Insights and Management Strategies. J Clin Exp Cardiolog. 15:896.
Received: 10-Jun-2024, Manuscript No. JCEC-24-31939; Editor assigned: 12-Jun-2024, Pre QC No. JCEC-24-31939 (PQ); Reviewed: 26-Jun-2024, QC No. JCEC-24-31939; Revised: 03-Jul-2024, Manuscript No. JCEC-24-31939 (R); Published: 10-Jul-2024 , DOI: 10.35248/2155-9880.24.15.896
Copyright: © 2024 Yadav MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.