Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2020)Volume 11, Issue 1
Pyoderma Gangrenosum (PG) is an inflammatory neutrophilic dermatosis of unknown etiology, primarily sterile with no underlying infectious process and commonly present as an association with a systemic disease. It is rarely seen in pediatric age group and here we describe an atypical presentation of painless cutaneous ulcerative eruption involving the upper thighs and buttock in an otherwise healthy 14-month-old girl. Diagnosis of idiopathic PG was made based on clinical and histopathological correlation, and after excluding other etiologies including immunodeficiency and infections. The patient improved and responded well within 4 weeks of treatment with systemic corticosteroids.
Pyoderma gangrenosum; Neutrophilic dermatoses; Pediatric; Cutaneous, Skin
Pyoderma Gangrenosum (PG) is an inflammatory neutrophilic dermatosis of unknown etiology. It was first described by a French dermatologist, Louis Brocq in 1916 and Fourteen years later Brunsting et al named it as PG in 1930 [1,2]. PG is uncommon with an incidence of 3-10 cases per million per year, affects any age group mostly adults between twenty and fifty years of age with a slight predilection for females. Pediatric presentation is rare and account for 4% of the cases. It is mainly idiopathic in (40%-50%), primarily sterile with no underlying infectious process and commonly present as an association with a systemic disease [1,3].
Classic clinical presentation is painful, rapidly evolving ulceration, with sharply marginated violaceous border and erythematous background over lower extremities, though any other body site can be involved. Besides the classic ulcerative presentation, four other clinical subtypes have been described; pustular, bullous, vegetative and peristomal [4,5].
Here we report a case of PG in an otherwise healthy, 14- monthold girl, with atypical presentation of painless ulceration involving the upper thighs and buttock.
A previously healthy, 14 months old girl was admitted to King Abdullah Specialized Children ’ s Hospital in Riyadh, Saudi Arabia, with a 5 days history of skin eruption in the diaper area. On examination, the patient was alert, playful and vitally stable, she had four symmetrically distributed, well defined ulcers with punched out border on the inner aspect of upper thighs and buttock area, surrounded by excoriated erythematous satellite papules (Figure 1). The initial clinical impression was of PG, further work up was conducted to rule out other etiologies and evaluate for systemic involvement. Laboratory workup was remarkable for a high white blood cell count (17.60 × 109/L [reference range, 4-12 × 109/L]) and elevated erythrocyte sedimentation rate (119 mm/hr [reference range, 0-20 mm/hr]). Other basic metabolic laboratory values were within normal values (liver function, renal function, and general electrolytes). Serological testing of Herpes simplex virus and Human immunodeficiency virus were negative and bacterial swab culture from the base of the lesion revealed scanty growth of Enterococcus faecalis.
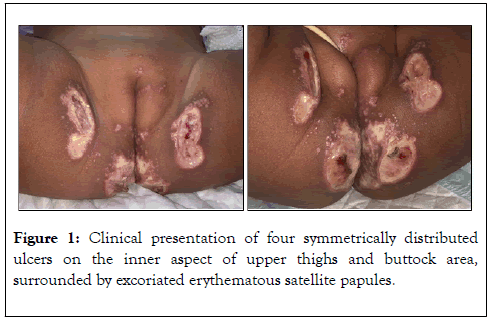
Figure 1. Clinical presentation of four symmetrically distributed ulcers on the inner aspect of upper thighs and buttock area, surrounded by excoriated erythematous satellite papules.
Two punch biopsies obtained from the ulcer border; one for tissue culture which revealed no growth of pathogenic organisms (bacterial, mycobacterial and fungal). The other punch sent for routine histopathology, the result of which showed an epidermal ulceration, with acanthosis, parakeratosis and hypergranulosis of the non-ulcerated side of the section, presence of mixed dermal inflammatory infiltrate, predominantly lymphoplasmacytic with few neutrophils and eosinophils. No features of infectious, vascular or granulomatous process noticed (Figure 2). Periodic acid-Schiff, Gomori Methenamine-Silver special stains and Epstein-Barr virus immunohistochemistry were all negative (Figure 2).
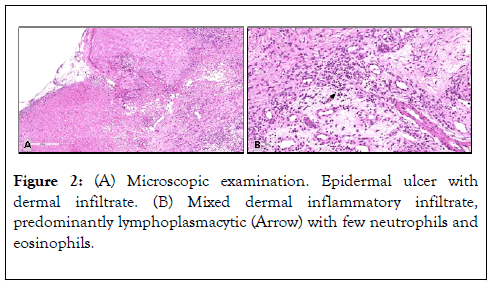
Figure 2. (A) Microscopic examination. Epidermal ulcer with dermal infiltrate. (B) Mixed dermal inflammatory infiltrate, predominantly lymphoplasmacytic (Arrow) with few neutrophils and eosinophils.
Imaging studies were performed, including renal ultrasonography and hip x-ray, the findings of which were normal. Immune function tests performed, she had low levels of immunoglobulins, IgG (3.11 g/L [reference range, 7.51-15.60 g/L]) and IgA (0.25 g/L [reference range, 0.82-4.53 g/L]), otherwise oxidative burst test and immunodeficiency panel were normal. Patient was treated with multiple intravenous antibiotics for 2 weeks and topical fusidic acid ointment, with poor response and minimal improvement. (Figure 3) Treatment with oral Predinsolone (2 mg/kg/day) was started and gradually tapered over 4 weeks, significant improvement noticed within 2 weeks (Figure 4), complete healing with scarring noticed over 2 months of follow up.
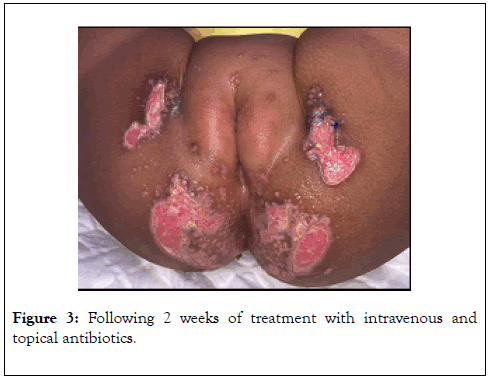
Figure 3. Following 2 weeks of treatment with intravenous and topical antibiotics.
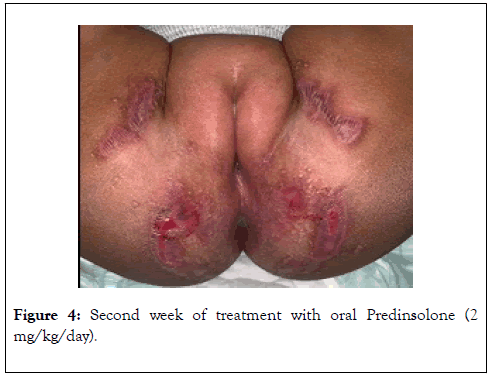
Figure 4. Second week of treatment with oral Predinsolone (2 mg/kg/day).
Pathogenesis of PG is not fully understood, involving interplay of dysfunctional neutrophils and inflammatory mediators in genetically predisposed patients [6]. The latest retrospective systematic review on 170 pediatric PG cases conducted by Kechician et al. revealed that the average age of diagnosis was 9.5 years, ulcerative subtype is the commonest clinical presentation (83.6%), 45% of the cases were idiopathic, with Inflammatory bowel disease being the commonest underlying association (20%) followed by hematopathological disorders (8.2%), vasculitis (6.5%), various immunodeficiency syndromes (5.9%), and other autoinflammatory syndromes (5.3%) including PAPA (pyogenic arthritis, PG, and acne), PAPASH (pyogenic arthritis, PG, acne, and hidradenitis suppurativa), and PASH (PG, acne, hidradenitis suppurative). Typical PG lesions are painful over lower extremities, in our patient the lesions were painless involving symmetrically the buttock and upper thighs. Perineum is the third most common location reported in pediatric cases, preceded by disseminated eruption (45%), and lower extremities (29.7%) [7].
PG is a diagnosis of exclusion and with low clinical suspicion due to it is rarity, identifying it can be challenging. Initially other cutaneous ulcerative etiologies need to be ruled out; thorough history, physical exam, excluding infectious causes along with tissue examination for routine histopathology, tissue cultures and special stains for infectious organisms are required. Specimens taken from the border of early active lesion will show an inflammatory neutrophilic infiltrate in a folliculocentric distribution with vasculitis, however histology can be inconsistent. PG is sterile in nature hence septic workup and tissue cultures are classically negative but can be secondarily colonized. Similarly, our patient showed no improvement despite being treated with IV antibiotics for 14 days (Figure 3). After confirming the diagnosis, investigations and work up should be done to rule out systemic etiology, since it can be an initial presentation of a systemic disease [3,8,9].
Treatment of PG should be tailored according to the patient’s condition, number of lesions, location and the association of systemic etiology. The aim is to control systemic condition, achieve wound healing and prevent recurrence. Local measures include appropriate wound care with dressings and barrier ointments to prevent local irritation. To date there is no goldstandard therapeutic regimen for adult or pediatric PG, monotherapy with systemic corticosteroids or in combination with steroid-sparing agents, especially Dapsone and Cyclosporine are reported to be used in 60% of the cases. Treatment can be tapered when re-epithelization occurs, observed by approximated edges and diminishing of the wound diameters till reach complete healing.
Citation: Alajroush W, Alqahtani N, Alfaleh A (2020) Idiopathic Pyoderma Gangrenosum in a Toddler: Case Report. J Clin Exp Dermatol Res. 11:516. Doi: 10.35248/2155-9554.20.11.516
Received: 24-Jan-2020 Accepted: 31-Jan-2020 Published: 07-Feb-2020 , DOI: 10.35248/2155-9554.20.11.516
Copyright: © 2020 Alajroush W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.