Journal of Antivirals & Antiretrovirals
Open Access
ISSN: 1948-5964
ISSN: 1948-5964
Research Article - (2010) Volume 2, Issue 1
A study on the prevalence of common intestinal parasitic diseases with a high carriage rate within the global population in Senegal was conducted among HIV-infected persons. A systematic parasitological stool test from 150 patients HIV infected showed a low carriage rate10.6% (16/150). The following parasites were isolated: Entamoeba coli 4% (6/150), Ascaris lumbricoides 2.6% (4/150) and Trichuris trichiura 1.3% (2/150). The 31-50 age group was the most affected one. The carriage rate stood at 93.3% among patients with a CD4 T-cell rate <500/ mm3, without any significant difference compared to intestinal parasite negative patients.
<Keywords: Intestinal parasites; HIV
In tropical areas, one of the most prominent features of HIV infection is its frequent association with opportunistic or not often parasitical infectious diseases. It should be noted that these co-infection can have an influence in the intensity of HIV infection in particular in viral load and CD4 T-cell rate. However, few studies have been conducted so far in on the common (non opportunistic) intestinal parasitic diseases-HIV in West Africa. We deemed it interesting to explore the relationship between HIV infection whose prevalence stands at 0.7% (CNLS, 2007) and the most widespread intestinal parasitic diseases in Senegal (Ascariasis, Giardiasis, Trichocephalosis, Amebiasis etc…) (Ndir et al., 2002), especially their potential effect in the infection intensity objectified by the CD4 T-cell rate.
The objectives of our study were to assess the prevalence of these parasitic diseases in HIV infected persons and to measure their potential effect on the CD4 T-cell rate. A prospective study was undertaken in HIV-1 or HIV-2 infected patients who were admitted or treated in an ambulatory way in the National Hospital Center of Fann which is the Senegalese reference centre for HIV management. An informed consent was obtained for each patient prior to his/her inclusion in the study.
Stool samples emitted in the morning by patients were collected and kept in a sterilized container then sent immediately to the parasitology laboratory of the Faculty of Medicine of the UCAD. A macroscopic examination was conducted followed by a fresh microscopic examination, after staining (Lugol and Zielh Neelsen modified) then after concentration (Ritchie, Baerman and Lee techniques). The clinical and biological data for all patients (HIV serotype, CD4 T-cells) were collected.
Sample size was calculated using Epi info software (version 6.04 d). Based on a prevalence of intestinal parasite infection at 56.5% (Ndir et al., 2002), assuming a precision of 10%, with a significance level (alpha two side) equal to 0.05, required sample size for this study is estimated at 100 patients. To avoid unreliable samples (20%) the required sample size was estimated at 120 patients.
Data were computered and analyzed using Epi info software (version 6. 04 d). Quantitative variables were described in terms of number of patients, average and standard deviation. Qualitative variables were described in terms of number of patients and percentage of data provided. Confidence intervals 95% (CI 95%) and relative risk (RR) were computed.
Comparisons between groups were made using the Pearson Chi square or Fischer exact test for qualitative data, and student t test or Mann Withney test for quantitative variables. A p value below 0.05 were considered as significant.
From December 2006 to March 2007, 150 HIV infected patients (HIV1 or HIV 2) were recruited. The average age was 39.7 years CI 95% [20-72 years]. 22% (33/150) were 20-30 years old, 64% (96/150) between 31 and 50 years old and 14 % (21/ 150) were above 50 years. The sex ratio (M/F) was 1.7.
Stools parasitological examination showed a carriage of at least an intestinal parasite in 10.6% (16/150). Among the parasites which were found, Entamoeba coli accounted for 4% (6/ 150) of cases followed by Ascaris lumbricoides for 2.6% (4/150) and Trichuris trichiura 1.3% (2/150). The other eggs or intestinal parasite cysts found were Giardia lamblia, Endolimax nana, Ancylostoma duodenale. Only one patient presented with a biparasitism with an Entamoeba coli and Trichuris trichiura association. Cryptosporidium parvum, Isospora belli and Microsporidium were not found.
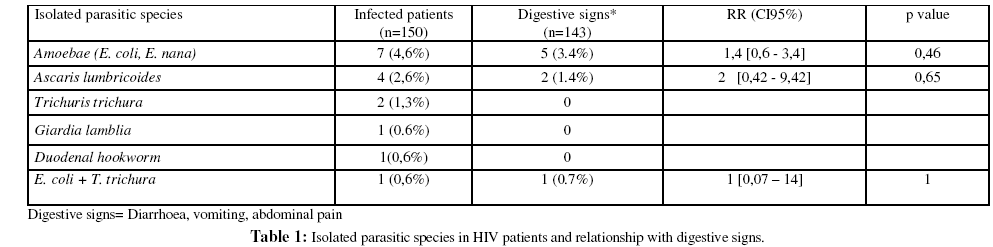
The 31–50 years age group was the most affected with 50% (8/16) of cases. A digestive symptomatology was found in 56.6% (85/150). Among these patients, 10.6% (9/85) were intestinal parasite carriers (Table 1). Digestive symptoms were noted in 56.7% among patient who didn’t have intestinal parasite (76/ 134) versus 56.2% in the group with intestinal parasite (9/16) (p=0.971). Among the positive patients (Table 1), this symptomatology was more frequent in the case of Entamoeba carriage (3.1%) with a relative risk 1.4 [0.6 – 3.4] even if the infecting capacity of the species found is not significant.
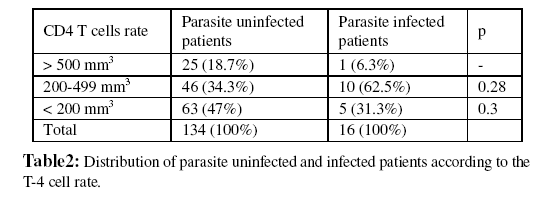
An analysis based on CD4 T-cells rate (Table 2) showed that 93.7% (15/16) of intestinal parasite positive patients had a CD4 T-cells rate below 500 of which 33% (5/15) with CD4 T-cells below 200 without any significant difference (p=0.2).
Despite a high rate of intestinal parasite carriage in Senegal (Ascaris lumbricoides: 34.17%, Giardia lamblia : 22.50%,Trichirus trichiura: 22.08% and Entamoeba coli :14.58%) (Ndir et al., 2002), the prevalence observed in our study seems to be low. Only 10% of HIV-infected patients were intestinal parasite carriers. A higher carriage rate was registered in Mali and in Ethiopia (Konate et al., 2005; Hailemariam et al., 2004).
The most frequent parasites were amoebae (Entamoeba coli, Endolimax nana) followed by Ascaris lumbricoides with a digestive sign associated in 3.4% and 1.4%, respectively, of parasitic carriage cases.
As demonstrated by other studies (Rossit et al., 2009; Mohandas et al., 2002), Ascaris lumbricoides, Giardia lamblia and Entamoeba histolytica infections are frequently found but in our study Giardia lamblia infection level during the HIV infection is low in Africa. Infection with Strongyloïdes stercoralis wich is very common and severe in HIV infection (Bava and Troncoso, 2009) and Entamoeba histolytica were not found. The presence of a digestive symptomatology (diarrhoea, vomiting, gastralgiae) is not correlated with the presence of intestinal parasites and seems to have a different origin (bacterial, viral or mycosis infection) as demonstrated by others studies (Rossit et al., 2009).
Regarding CD4 T-cells, 93.7% of the intestinal parasite positive patients had a CD4 T-cells rate below 500 (of which 31.3% with a rate below 200). Even though a negative impact of intestinal parasites on CD4 T-cells was not demonstrated in our study and in some others studies (Rossit et al., 2009), an immunity deregulation is possible, making these patients more vulnerable with a decrease of CD4 T-cell (Harms and Feldmeier, 2002; Mohandas et al., 2002). This negative impact seems to be more frequent in infections with coccidia (Mariam et al., 2008; Assefa et al., 2009). However, a deworming must present a positive impact in CD4 T-cell count (Walson et al., 2009).
This study has shown a low level of intestinal parasite carriage among HIV infected patients. However, further studies are needed to establish the national epidemiological profile of intestinal infection during HIV carriage in order to guide policy markers and medical staff.
All patients who accepting to participate to this study ; the medical staff of Clinique des maladies infectieuses Ibrahima Diop Mar ; of the Centre Régional de Recherche et de Formation à la Prise en charge clinique du VIH /Sida et maladies associées (CRFP) and of the Centre de Traitement Ambulatoire (CTA).