Journal of Thyroid Disorders & Therapy
Open Access
ISSN: 2167-7948
+44 1300 500008
ISSN: 2167-7948
+44 1300 500008
Research Article - (2022)Volume 11, Issue 1
The workup of Incidental Thyroid Nodules (ITNs) is costly for both patient and the associated health care system, and there have been no studies to date demonstrating the value of building a best practice model for ITN evaluation. The purpose of the study is to evaluate the impact of adding the following statement to a Computed Tomography (CT) report when an ITN has been discovered: “No further follow up is indicated for the ITN”. A tertiary multicentre clinical decision analysis study was performed where the primary outcome measured was the adherence to the best practice of including the statement when indicated. Data was collected from eight radiology practices for a preintervention six-month period from February to July 2015 including 1936 CT scans, and a post-intervention period from July to December 2015 including 2121 CT scans. Nodules were reported according to best practice 30.81% during the pre-intervention period, and 84.35% during the post-intervention period. Using a clinical decision analysis tree and previous Medicare data, there was a predicted cost savings of approximately $23,057,208. At the same time, an estimated 7,592 negative fine needle aspirations were avoided and 750 additional thyroid cancers were estimated to be detected. Significant cost control and universal health benefit can be achieved if referring physicians adhere to the best practice of not following-up ITNs that meet criteria.
Thyroid nodule; Incidental Thyroid Nodule (ITN); Best practice model
An incidental thyroid nodule (ITN) is defined as a nodule identified on an imaging exam that was not present on earlier exams or is suspected based on a clinical exam. ITNs are a relatively common finding on advanced medical imaging exams and it has been reported that ITNs are seen in 16-18% of CT and Magnetic Resonance Imaging (MRI) scans in which the neck is imaged [1]. In order to create a best practice approach to the work-up of ITNs, radiologists need to give referring physicians better guidance of what the work-up should include, if anything at all. The overutilization of follow-up thyroid images and potential thyroid ablation techniques has resulted in adding to the rise of healthcare spending and reducing the Quality Adjusted Life Years (QALY) in patients with ITNs. Radiologists can be fearful of missing critical results and often recommend more imaging for continued follow-up, however,such practice might lead to further potentially unnecessary, risky, and costly procedures, perpetuating the overuse dynamic.
Value in health care is defined as the quality of care delivered per dollar spent [2]. Given the current economic environment and the need to develop innovative health care best practices that increase the value of care, the purpose of our study was to evaluate the impact of adding the following statement to a CT report that has discovered an ITN: “No further follow up is indicated for the ITN”. It was then evaluated whether this statement had a significant effect on the reduction of follow-up thyroid ultrasounds, thyroid fine needle biopsies, thyroid surgeries, and health care dollars saved after implementing this best practice standard of managing ITNs. Creating value through an economic model should lead to a significant reduction in overall health care dollars spent, an improvement in overall health care system performance ranking, and an improvement in overall patient health status.
This study involved eight tertiary referral hospitals. Computed tomography imaging was reviewed in a pre-intervention six-month period from February to July 2015. CT imaging was then reviewed for a post-intervention six-month period from July to December 2015. Patients were excluded from the study if there was a history of a known thyroid nodule, history of thyroidectomy, or known thyroid dysfunction. Scoring of adherence to best practice was performed by a group of nine highly trained board certified radiologists who were blinded to the data collection. A randomized list of cases was provided to each radiologist and a “Smart Sheet” entry form was utilized for data entry by each reviewer that included if a nodule was present, size of the nodule, and whether or not best practice standards were followed. Descriptive statistics on presence of nodule, nodule size, and recommendation for Ultra Sound (US) follow-up were calculated for the pre- and post-intervention periods.
Analysis was performed using SAS version 94.4. Pre- and postintervention data was utilized in a clinical decision analysis tree. The percentages utilized in the decision tree were obtained from the study dataset and from the literature reviewed. Standard costs for follow-up US, Fine Needle Aspiration (FNA)/biopsy, and thyroidectomy were estimated from a cohort of patients who had a CPT code of chest CT (71250, 71260, 71270, 21275) in the Medicare 5% limited data set for 2016. Unit costs for use in the model were calculated as mean payments for ultrasound (CPT 76536), fine needle aspiration (CPT 76942), biopsy (CPT 60100, 10022), and surgery (CPT 60512, 60500, 60502, 60505, 60212, 60225, 60240, 60252, 60254, 60260, 60270, 60271).
The results from the decision tree analysis were used to identify expected differences in long term outcomes for the study.
Pre and post-intervention dataset
1936 CT scans of the chest, neck, and cervical spine were performed during the pre-intervention period from February 2015 to July 2015 and 2121 CT scans were performed during the postintervention period from July 2015 to December 2015. Figures 1 and 2 summarize the breakdown of CT scans performed during the pre- and post-intervention periods at each of the facilities and their representative percentage of the total amount of scans performed (Figures 1 and 2).
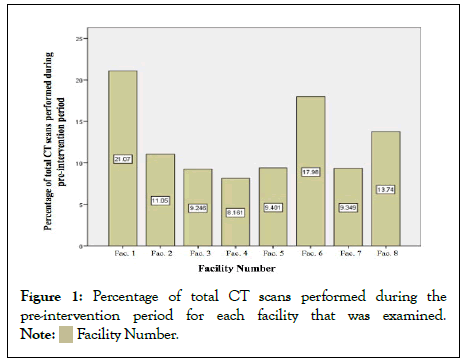
Figure 1: Percentage of total CT scans performed during the pre-intervention period for each facility that was examined.

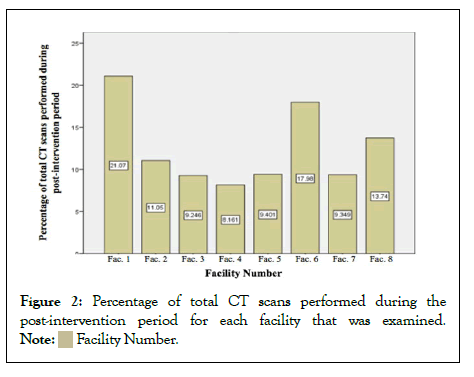
Figure 2: Percentage of total CT scans performed during the post-intervention period for each facility that was examined.
A total of 4057 CT scans were examined. Of these, 766 (18.88%) scans had an observed nodule and 295 (38.51%) of these nodules were noted in the CT report. Each facility contributed a mean of 254 CT scans in the pre- and post-intervention periods with a range of 358 to 816 exams towards the study.
Primary outcome-best practice standard adherence
During the pre-intervention period, a total of 65 (30.81%) of 211 nodules were reported according to best practice standard. This best practice reporting range varied from a high of 53.94% to a low of 7.14% (p=.0005) between facilities. The adherence to the best practice standard during the post-intervention period was 194 out of 230 (84.35%) observed nodules for a best practice adherence of 84.35%. The range in adherence to best practice between facilities ranged from 56.25% to 91.18%. This difference was not statistically significant (p=0.0751). General adherence and implementation of the best practice standard between pre- and post-intervention increased from 27.0% in the pre-intervention period to 73.0% in the post-intervention period, which was statistically significant (p<.0001).
Follow-up ultrasound according to best practice standards
18% of patients in our overall study population had a thyroid nodule. During the pre-intervention period, 30.81% of the 211 nodules identified were reported and during the post-intervention period 84.35% of 230 nodules were reported. 41% of patients with thyroid nodules received ultrasound examinations in the preintervention group, whereas 45% received ultrasound examinations in the post-intervention group.
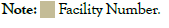
Within the pre-intervention group, only 50% of those patients received ultrasound following up examinations according to best practice standard, compared to 92% of the patients in the postintervention group. Of the patients in the pre-intervention group who did not receive a follow up ultrasound, 61% was in accordance with best practice standard, whereas 92% was in accordance with best practice standard in the post-intervention group. Figure 3 demonstrates the adherence to best practice guidelines for receiving a follow-up ultrasound. The first part of Table 1 summarizes our study-derived data utilized in the derivation of the decision analysis tree.
Additional thyroid cancers detected and negative FNAS avoided
Using the decision analysis tree estimates previously described and data from previously published studies, estimates were extrapolated of the number of additional thyroid cancer cases detected and the number of negative FNAs avoided (Figure 3). Within the preintervention group, 17% of patients received a follow-up ultrasound in contradiction to best practice standard. With an estimated 76% of the population having a TI-RADS 3 or above thyroid nodule and an estimated 30% of all fine needle aspirations having a diagnostic outcome, the decision analysis tree was able to be completed for the follow-up ultrasounds that were received in contraindication to best practice standards [3]. For the patients who did not receive a follow-up ultrasound in contraindication to best practice standards, the amount of missed thyroid cancers was extrapolated using the missed thyroid cancer incidence in the general population [4]. The remaining portions of Table 1 summarize the origin of the data utilized in the decision analysis tree (Figure 3).
Figure 3: Decision analysis tree reporting percentages of patient population. Utilizing study derived population thyroid nodule incidence and percentages of ultrasound follow up studies according to best practice, the number of additional thyroid cancers detected and the number of negative FNAs that were able to be avoided were calculated.
| Variable name | Base value | Data source |
|---|---|---|
| Study population overall nodule rate | 0.1888 (range 0.1707-0.2087) | CT study data |
| Pre-intervention percent Received US | 0.41 | CT study data |
| Post-intervention percent Received US | 0.45 | CT study data |
| Pre-intervention percent who received US according to best practice standard | 0.5 | CT study data |
| Post-intervention percent who received US according to best practice standard | 0.92 | CT study data |
| Pre-intervention percent who received US not in accordance with best practice standard | 0.17 | CT study data |
| Post-intervention percent who received US not in accordance with best practice standard | 0.44 | CT study data |
| Overall population incidence of TI-RADS3+ category in patients with thyroid nodules | 0.756 | Pantano study 2018 [3] |
| Overall population incidence of positive FNA biopsy in patients with thyroid nodules | 0.3 | Pantano study 2018 [3] |
| Missed thyroid cancer incidence | 0.0055 | Ospina study 2016 [4] |
Table 1: Summary of data used for the decision analysis estimates.
Cost savings analysis
Using the decision analysis tree estimates and data from the 5% Medicare sample data set, an estimated cost savings was able to be calculated. With a total of 185,976 CT scans reported in the Medicare data and 20% of the population expected to have thyroid nodules, approximately 38,813 nodules would be detected. According to Medicare data, 5,162 of those patients had a follow-up ultrasound (regardless of best practice standards) resulting in 5,642 FNAs and 693 surgeries. The individual costs for ultrasounds, FNAs, and surgical costs were also able to be determined (Table 2).
| Medicare 2016 data | Our CT Study Data | ||
|---|---|---|---|
| Number of CT scans | 185976 | ||
| Expected Nodules | 38813 | ||
| Number of US performed | 5162 | ||
| % of patients who received an US | 13.30% | 9.39% | |
| Number of FNAs performed | 5642 | ||
| % of patients who received a FNA | 3.08% | 2.63% | |
| Number of surgeries | 693 | SD | Median |
| Surgery/FNA | 12.30% | 22.60% | |
| Outpatient surgery cost (N=467) | $3,921 | 1024 | 3830 |
| Inpatient surgery cost (N=226) | $13,970 | 12568 | 11641 |
| Mean of surgery cost | $6,741 | ||
| FNA cost | $36 | $11 | |
| US cost | $54 | $36 |
Table 2: Base estimation cost for treatment and surgery of 2016 data.
Using the above generated costs and population incidence of thyroid nodules, ultrasound follow-up examinations, FNAs, and surgery, the following Monte Carlo simulation output was generated with a +/- 10% standard deviation for each variable, of which the median is $22,563,522 (Figure 4).
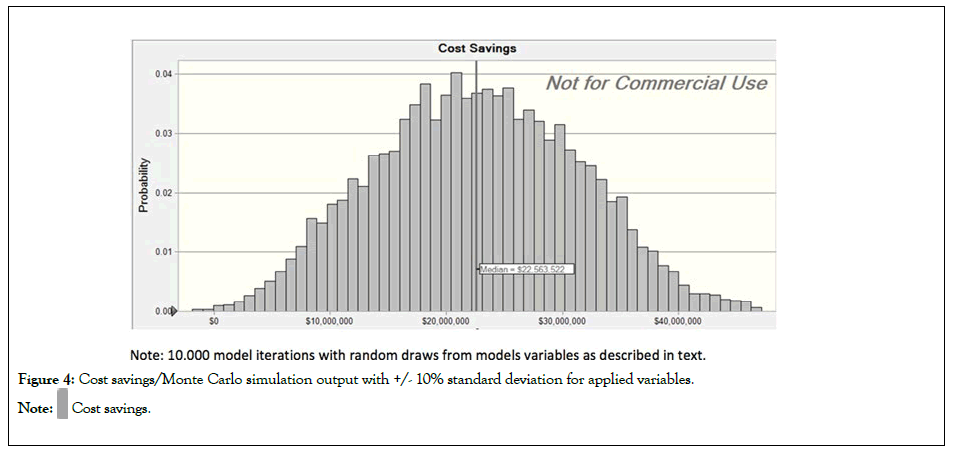
Figure 4: Cost savings/Monte Carlo simulation output with +/- 10% standard deviation for applied variables.
With a total of 3,615,800 chest CT scans performed on Medicare patients in 2016 and an estimated population thyroid nodule incidence of 20.87%, the following data was extrapolated by applying our study rates of follow-up ultrasounds received for both pre- and post-intervention data (Table 3).
| Pre-intervention | Post-intervention | |
|---|---|---|
| Chest CT scans | 36,15,800 | 36,15,800 |
| Population incidence of thyroid nodules | 0.2087 | 0.2087 |
| Patients with nodules | 7,54,617 | 7,54,617 |
| % of patients who received an US | 41 | 45 |
| US received according to best practice (%) | 50 | 92 |
| No US according to best practice (%) | 61 | 91 |
| US received in contradiction to best practice (%) | 17 | 44 |
| Population incidence of TI-RADS 3+ (%) | 75.6 | 75.6 |
| FNA (+) biopsies (%) | 30 | 30 |
| Incidence of missed thyroid cancer (%) | 0.55 | 0.55 |
| 2016 Estimated medicare costs | ||
| US cost | $54 | $54 |
| FNA cost | $36 | $36 |
| Surgery cost | $6,741 | $6,741 |
| Total cost | $42,302,658 | $19,245,450 |
| Missed cancer | 955 | 205 |
| Negative FNAs | 13917 | 6326 |
| Cost savings | $23,057,208 | |
| Missed cancer avoided | 750 | |
| Negative FNAs avoided | 7,592 | |
Table 3: Pre- and post-intervention base estimates cost savings, calculated from study rate of follow-up ultrasounds received according to and in contradiction to best practice standards extrapolated to Medicare 2016 data.
The base value savings was estimated to be $23,057,208 while 750 additional thyroid cancers were detected and 7,592 negative FNA avoided.
Incidentalomas such as ITNs are a relatively frequent finding of medical imaging exams. Our study results are consistent with previous studies, with an ITN frequency of about 18.88% [1]. During the pre-intervention period, 30.81% of the 211 nodules identified were reported and during the post-intervention period 84.35% of 230 nodules were reported. This is a significant response to adhering to a best practice standard. If ITN best practice reporting standards were applied to a cohort of Medicare patients, this best practice would generate a cost savings $23,057,208 and would result in approximately 750 additional thyroid cancers detected, as well as 7,592 negative FNAs being avoided.
Thyroid nodule evaluation and management has always been very cumbersome for radiologists and referring clinicians. With the recent ACR adoption of the TI-RADS risk stratification system for classifying thyroid lesions, thyroid reporting has become more streamlined. While the workup of a thyroid nodule with ultrasound and a FNA/biopsy seems rather benign, there are several issues regarding the further workup that may prove to be harmful and disadvantageous for the patient. When findings suggest a benign cytological diagnosis, there is a good prognosis in terms of patient-important outcomes, which should ultimately encourage all clinicians to ensure appropriate follow-up or for radiologists to include the phrase “no further follow-up needed for this ITN” in the report. This will hopefully avoid overwhelming the healthcare system with useless overutilization of unneeded thyroid imaging and FNA/biopsies. If a thyroid nodule is malignant, the need for follow-up with FNA/biopsy and possibly a thyroidectomy is indicated. However, an issue arises when a patient is categorized as non-diagnostic or indeterminate. These patients may require a second FNA/biopsy, adding to the cost of the thyroid nodule workup. In the categories of suspicious for malignancy, or suspicious for follicular neoplasm, diagnostic thyroid lobectomy is recommended. Of patients who undergo FNA biopsy for thyroid nodules, 22% to 41% proceed to a diagnostic surgical thyroid lobectomy [5]. Of further interest, in a retrospective review of this patient cohort (those patients proceeding to surgery following FNA biopsy), 76% percent of those patients had surgically proven benign results [6]. While there was no cancer, the patient underwent an unnecessary surgery that incurred potential risks in addition to added health costs incurred by the patient and healthcare system.
Over-diagnosis of thyroid cancer is another potential problem if best practice standards are not implemented in the follow-up of ITNs. Over-diagnosis is the detection of disease that will not result in death or cause symptoms related to a particular disease process. There is a mismatch in rates between the incidence of thyroid cancer and the mortality [7]. The incidence of thyroid cancer in 2009 was 14.3 per 100,000 persons, which represented a quadrupling in incidence in 36 years; however, there was no change in the mortality rate, which in 2009 was 29 times lower than the incidence [8]. The mismatch between incidence and mortality suggests that additional cancers were treated without survival benefit.
For the cases of thyroid cancer that proceed to treatment of either thyroidectomy or radioactive iodine therapy, there are multiple possible significant complications. In addition to the general risks of surgery, potential risks include recurrent laryngeal nerve injury, Hypoparathyroidism, hypocalcaemia, and vocal cord paresis [9]. Patients requiring total thyroidectomy also require lifelong thyroid hormone replacement with regular monitoring of thyroid hormone blood levels. Radioactive iodine treatment also has potential serious adverse side effects with associated risks of future secondary cancers.
The costs of thyroid cancer to the US health care system are substantial. Most of the costs are incurred during the initial diagnosis and follow up phases of treatment. With such a burden on the US health care system, there is a need for more cost analysis studies to better understand the real impact on society. Using a model developed in 2014 and current incidence trends, thyroid cancer costs are estimated to exceed $3.5 billion dollars. While our study did not specifically look at the costs of thyroid cancer treatment, there is considerable overlap with previous cost analysis studies, in particular a study performed in 2013 estimating the overall societal cost for the treatment of differentiated thyroid cancer. Using this model, the predicted costs by year 2030 based on current incident trends is projected to exceed $3.5 billion [10]. Our study projects a significant cost-savings that would offset the billion-dollar cost of managing and treating ITNs.
In order to control costs, recommendations for the work-up of ITNs need to be embraced. A 2015 ACR white paper on ITNs provides a set of evidence-based guidelines for radiologists to follow. This white paper aimed to improve appropriateness of the management of ITNs and also to reduce variability in radiology recommendations regarding the further work-up of ITNs [11]. Our study verifies the need for a best practice standard regarding recommendations for further work-up of ITNs detected at CT. From the ACR 2015 white paper, dedicated thyroid ultrasonography is only recommended for nodules at least 1.5 cm in patients 35 years or older and for nodules at least 1.0 cm in patients younger than 35 years. As demonstrated in our study, when best practice models are adhered to, the use of the radiology report is a powerful platform in order to convince clinicians that no further work-up is required. The goal of any best practice model should be to diagnose clinically significant diseases, while reducing unnecessary workup and providing guidance for clinical practice.
Summary sentence
If ITN best practice reporting standards were applied to a cohort of Medicare patients, this best practice would generate a cost savings $23,057,208 and would result in approximately 750 additional thyroid cancers detected, as well as 7,592 negative FNAs being avoided.
Take home points
• By creating a new best practice standard to include the statement “no further follow up is indicated for the ITN” for incidental thyroid nodules, significant cost control and universal health benefit can be achieved.
• After examining the CT scans and results of 4057 adults, the post-intervention adherence to best practice standard was 84.35%, which was a significant increase from 30.81% preintervention adherence.
• By adhering to the proposed best practice standard, there is a projected significant cost-savings in Medicare population of about $23 million and a significant health benefit of reduction in number of negative FNAs.
Author has nothing to disclose.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Wulfeck D, Bronner J, Crawford TJ, Kocher M, Simpson K (2022) Impact of Report Recommendation on Follow-up Ultrasound Studies in the Work-Up of Incidental Thyroid Nodules. Thyroid Disorders Ther. 11:265.
Received: 17-Jan-2022, Manuscript No. JTDT-22-15491; Editor assigned: 21-Jan-2022, Pre QC No. JTDT-22-15491(PQ); Reviewed: 11-Feb-2022, QC No. JTDT-22-15491; Revised: 18-Feb-2022, Manuscript No. JTDT-22-15491(R); Published: 25-Feb-2022 , DOI: 10.35248/2167-7948.22.11.265
Copyright: © 2022 Wulfeck D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.