
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2024)Volume 14, Issue 3
Objective: To observe the influence factors of assisted reproductive treatment outcomes and the impact of the combined application of DE T-1 (Shawkea T-1) and Sho-ko-sen (Songkangquan) of refractory infertility patients.
Methods: A retrospective study was conducted. 31 patients defined as refractory infertility who had embryo transfer at least one time with the pregnancy test positive at Hanabusa Women’s Clinic of Japan from January 2016 to October 2019 were enrolled in this study. All the enrolled patients took DE T-1 oral solution and Sho-ko-sen capsule according to the nutritional support center's recommendations at Hanabusa Hospital. The general information of the patients was recorded, and In Vitro Fertilization (IVF) treatment process was recorded and the usage of the DE T-1 and Sho-ko-sen was analyzed.
Results: The patients enrolled were aged from 30 to 48 years, with a median (P25, P75) age of 36.0 (34.0, 39.0) years. AMH ranged from 0.4 ng/ml to 17.9 ng/ml, with a median (P25, P75) of 1.74 (0.80, 3.90) ng/ml. The duration of infertility ranged from 3 to 12 years, with a median (P25, P75) of 6.0 (5.0, 9.0) years. All 31 patients gave live births, including 29 cases (93.5%) with single births and 2 cases (6.5%) with twins. A total of 72 egg retrieval cycles were performed in the 31 patients, including 5 cases (6.5%) of long protocol, 7 cases (9.7%) of short protocol, 12 cases (16.7%) of antagonist protocol, and 48 cases (66.7%) of micro-stimulation protocol. Among the 31 patients included, 7 cases (22.6%) underwent one egg retrieval cycle, 16 cases (51.6%) underwent two cycles. A total of 38 embryo transplantation cycles were performed in the 31 patients, including 24 cases (77.4%) with one transplantation, and 7 cases (22.6%) with two transplantations. Among the 38 transplantation cycles, 36 (94.7%) used the Stimulation of Endometrium-Embryo Transfer (SEET) method and 2 (6.3%) used the two-stage method. Among the enrolled patients, 10 cases (32.3%) took 3 bags of DE T-1 and 6 capsules of Sho-ko-sen; 18 cases (58.1%) took 4 bags of DE T-1 and 6 capsules of Sho-ko-sen; and 3 cases (9.7%) took 5 bags of DE T-1 and 9 capsules of Sho-ko-sen. The duration of DE T-1 and Sho-ko-sen usage ranged from 4 to 45 months, with a median (P25, P75) duration of 10 (7, 14) months.
Conclusion: Under the premise of standardized IVF treatment, taking DE T-1 and Sho-ko-sen according to standardized courses and doses might help patients with refractory infertility achieve satisfactory treatment results, and mild stimulation would be the most suitable method for oocyte retrieval.
Refractory infertility; IVF; Live birth rate; AMH; DE T-1; Sho-ko-sen
China has entered the ranks of countries with a high rate of infertility due to various factors, including the fact that the average age of first marriage for women is over 30 years old and work pressure is increasing. The incidence of infertility in China is around 18%, with nearly 48 million couples experiencing reproductive health issues nationwide [1]. Some patients with refractory infertility have failed to conceive despite years of preparation and multiple attempts of assisted reproductive treatment. This not only poses a series of social problems but also brings tremendous psychological pressure to these patients [2].
The principal raw material of DE-T1 (Shawkea T-1) is dandelion, and its primary component is a type of amino-polysaccharide extracted from dandelions (Taraxacum mongolicum Hand.-Mazz). Dandelion polysaccharides (or polysaccharide extracts) were identified to possess multiple functions, including antioxidant, hepatoprotective, anti-free radical, growth-factor secretory, hypoglycemic, and antitumor activities [3-5]. Previous study ascertained that DE-T1 could regulate the pituitary-ovarian reproductive axis and female hormone secretion, and promoted growth and inhibited apoptosis of ovarian granulosa cells [6,7]. The usage of DE-T1 was identified to have an influence on improving the blastocyst formation rate and live birth rates in women undergoing IVF-ET treatment, and women of different ages and AMH levels could benefit from DE-T1 usage [8,9].
The main ingredient of Sho-ko-sen (Songkangquan) is pine polyphenols extracted from pine knots, which are the nodules on the branches of pine trees (including Pinus tabulaeformis Carr., Pinus massoniana Lamb., Pinus densiflora Sieb.et Zucc., and Pinus yunnanensis Franch). Pine knots are a rich source of lignans, flavonoids, and stilbenes. These bioactive compounds are widely known for their roles to combat human disorders but also to protect plants against pathogens [10,11].
This study aims to observe the impact of the combined application of DE T-1 and Sho-ko-sen on the assisted reproductive treatment outcomes of refractory infertile populations using a retrospective study design. The general information of the patients will be recorded, and the treatment process will be summarized to provide references for future prospective randomized controlled trials.
This study was approved by the Institutional Review Board (IRB) of Hanabusa Women’s Clinic (approval number: 2021-09).
Inclusion criteria
The definition of refractory infertility: 1) Infertility duration ≥ 3 years; 2) Age ≥ 40 years; 3) AMH ≤ 1.1 or>6.8; 4) A history of IVF treatment failure. Any patient who meets three of the four items above was defined as refractory infertility.
Patients who meet all the following requirements was included: 1) Meet the above definition for refractory infertility; 2) Regularly take DE T-1 oral solution and Sho-ko-sen capsules at the required dosage and course, and have corresponding purchase records; 3) Patients volunteer to participate in the investigation and sign the informed consent form; 4) The patient has undergone at least embryo transfer once during the observation period, and the pregnancy test was positive, in the meantime follow-up is required until delivery.
Exclusion criteria
• Surrogate mothers.
• Patients who took other plant extracts during the observation period.
Treatment method
All the patients underwent standardized Japanese Reproductive Assisted Reproductive Technology (JISART) intervention. On this basis, DE T-1 and Sho-ko-sen were taken according to the nutritional support center's recommendations at Hanabusa Hospital.
Observation indicators and methods
General information: The age, AMH value, infertility time and reasons for infertility of the enrolled patients, as well as their husbands’ semen situation were recorded.
Delivery outcome: All included patients were followed up to record their pregnancy and delivery outcomes.
IVF treatment information: The IVF treatment situation of included patients was statistically analyzed, including the number of egg retrieval cycles, egg retrieval plans, embryo culture and PGT-A (Preimplantation Genetic Screening) situation, transplantation situation, etc.
Usage analysis: The DE T-1 and Sho-ko-sen dosage and course of treatment of included patients were counted and analyzed.
Statistical methods
Data were analyzed using SPSS 23.0. The measurement data that conformed to the normal distribution and had homogeneous variance were expressed as mean ± standard deviation [(x̄ ± s)]. The measurement data that did not conform to the normal distribution or had heterogeneous variance were expressed as median [P25, P75]. Count data were expressed as number of cases and percentage (%).
Sources and general conditions of cases
According to the inclusion criteria, 31 patients treated at Hanabusa Hospital from January 2016 to October 2019 were collected.
Reasons for infertility: Poor ovarian function (including premature ovarian failure, advanced age ovarian failure, poor egg quality) in 27 cases (87.1%), severe polycystic ovary syndrome in 4 cases (12.9%).
Husband's semen situation: Activity rate<20% in 5 cases (16.1%), concentration<20 million/ml in 2 cases (6.2%), azoospermia in 1 case (3.2%).
The general condition is shown in Table 1.
| Item | Range | M(Q25,Q75) |
|---|---|---|
| Age(year) | 30~48 | 36.0(34.0,39.0) |
| AMH(ng/ml) | 0.4~17.9 | 1.74(0.80,3.90) |
| Infertility time(year) | 3~12 | 6.0(5.0,9.0) |
Table 1: General condition of 31 refractory infertility patients included.
Delivery outcome
After follow-up, all 31 patients gave birth alive with a live birth rate of 100%. Among them, 29 cases (93.5%) were single birth and 2 cases (6.5%) were twins. No abortion or fetal demise occurred in the patients included in the observation. All patients gave birth alive after positive pregnancy determination.
IVF treatment information
Egg retrieval protocol: A total of 72 egg retrieval cycles were performed in 31 patients, including long protocol in 5 cases (6.5%), short protocol in 7 cases (9.7%), antagonist protocol in 12 cases (16.7%), and micro-stimulation in 48 cases (66.7%) (Figure 1).
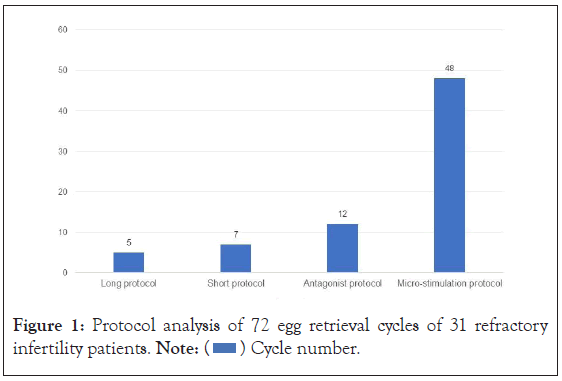
Figure 1: Protocol analysis of 72 egg retrieval cycles of 31 refractory infertility patients. Note:  Cycle number.
Cycle number.
Egg retrieval cycle: Among the 31 included patients, 7 cases (22.6%) underwent 1 egg retrieval cycle, 16 cases (51.6%) underwent 2 cycles, 2 cases (6.5%) underwent 3 cycles, and 3 cases (9.7%) underwent 4 cycles. Additionally, 1 case (3.2%) underwent 5 cycles, 1 case (3.2%) underwent 6 cycles, and 1 case (3.2%) underwent 8 cycles (Figure 2).
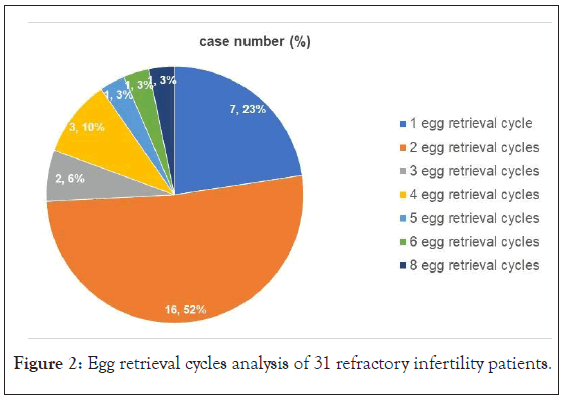
Figure 2: Egg retrieval cycles analysis of 31 refractory infertility patients.
Fertilization: Among the 68 cycles that retrieved qualified eggs, 2 micro-stimulation cycles of a patient (aged 35 years with AMH value of 0.5 ng/ ml) each retrieved 1 or 2 eggs, but none of them formed a fertilized egg. The other 66 cycles (97.1%) formed fertilized eggs.
Blastocyst culture: Among the 66 cycles that formed fertilized eggs, 62 cycles (93.9%) had all fertilized eggs cultured into blastocysts, while the other 4 cycles preserved early embryos. Among the 62 cycles that were cultured into blastocysts, 10 cycles (16.1%) did not successfully cultivate blastocysts; 52 cycles (83.9%) successfully cultivated blastocysts.
Preimplantation Genetic Testing for Aneuploidy (PGT-A): Among the 52 cycles that obtained blastocysts, 43 cycles (82.69%) underwent PGT-A. A total of 118 blastocysts underwent PGT-A, including 56 (47.5%) euploid, 19 (16.1%) mosaic, and 43 (36.4%). The details of IVF treatment are shown in Figure 3.
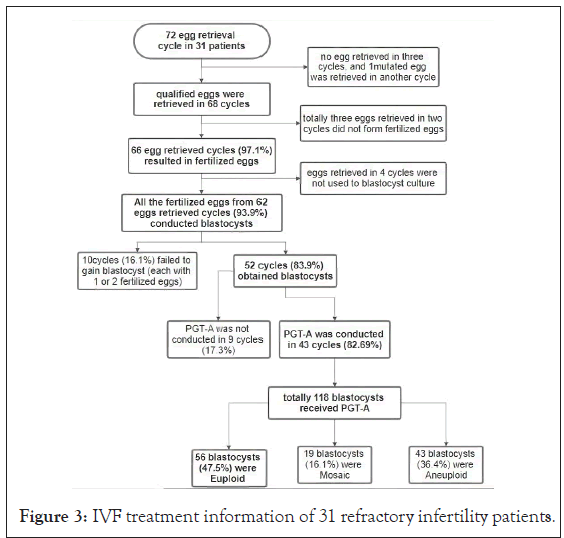
Figure 3: IVF treatment information of 31 refractory infertility patients.
Transplantation situation
A total of 31 patients underwent transplantation in 38 cycles, of which 24 cases (77.4%) received transplantation once and 7 cases (22.6%) received transplantation twice. Among the 38 transplantation cycles, 36 cycles (94.7%) used the Stimulation of Endometrium-Embryo Transfer (SEET) method, and 2 cycles (6.3%) used the two-stage method (Figures 4 and 5).
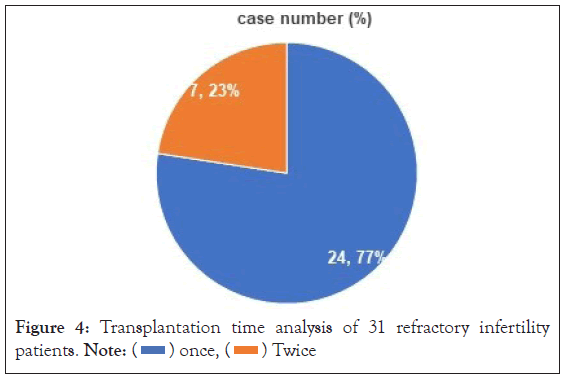
Figure 4: Transplantation time analysis of 31 refractory infertility patients. Note:  once,
once,  Twice
Twice
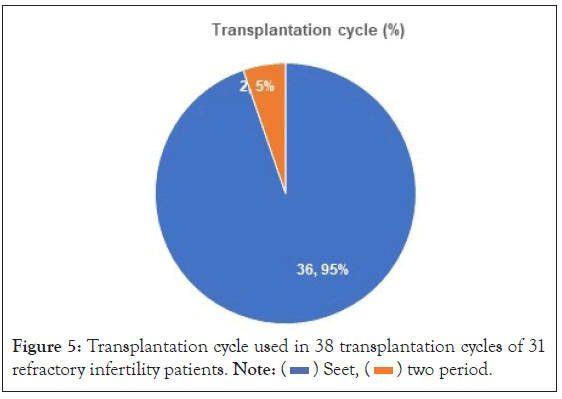
Figure 5: Transplantation cycle used in 38 transplantation cycles of 31 refractory infertility patients. Note:  Seet,
Seet,  two period.
two period.
DE T-1 and Sho-ko-sen usage
The duration of treatment until pregnancy diagnosis varied from 4 to 45 months, with a median duration of 10 months (7 to 14 months). The daily dosage of DE T-1 and Sho-ko-sen used by these patients were as follows: 10 cases (32.3%) used 3 bags of DE T-1 and 6 capsules of Sho-ko-sen, 18 cases (58.1%) used 4 bags of DE T-1 and 6 capsules of Sho-ko-sen, and 3 cases (9.7%) used 5 bags of DE T-1 and 9 capsules of Sho-ko-sen (Figure 6).
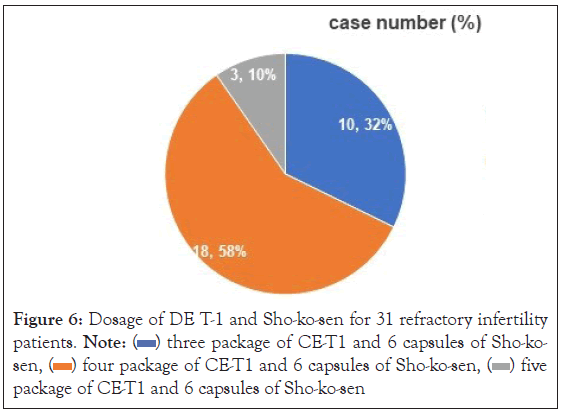
Figure 6: Dosage of DE T-1 and Sho-ko-sen for 31 refractory infertility patients. Note:  three package of CE-T1 and 6 capsules of Sho-kosen,
three package of CE-T1 and 6 capsules of Sho-kosen,  four package of CE-T1 and 6 capsules of Sho-ko-sen,
four package of CE-T1 and 6 capsules of Sho-ko-sen,  five package of CE-T1 and 6 capsules of Sho-ko-sen.
five package of CE-T1 and 6 capsules of Sho-ko-sen.
Characteristics and treatment outcomes of patients included in the study
The 31 patients included in this study had the following characteristics: Advanced age (up to 48 years), long duration of infertility (up to 12 years), poor ovarian function (AMH values ranging from 0.4 to 17.9), and high treatment difficulty (most had failed IVF treatment). However, all 31 patients achieved pregnancies after treatment, indicating that with appropriate treatment and persistence, satisfactory treatment outcomes can still be achieved for patients with refractory infertility.
Analysis of IVF treatment
Of the 31 patients included in this study, only 7 cases (22.6%) underwent oocyte retrieval once, while more than half (16 cases, 51.6%) underwent oocyte retrieval twice. The three patients who underwent the most retrieval cycles each underwent 8, 6, and 5 cycles, respectively (one patient per cycle). This shows that although refractory infertility patients who achieve pregnancy with one retrieval are few in number, more than 70% of patients can achieve satisfactory fertility results after two retrievals.
More than half (66.7%) of the 31 patients included in this study used mild stimulation for oocyte retrieval, indicating that mild stimulation may be more suitable for most refractory infertility patients.
Regarding blastocyst culture, 83.9% of the 62 cycles using initial embryos achieved blastocysts, indicating a high blastocyst culture success rate. When considering the number of oocyte retrieval cycles instead, excluding the four cycles where initial embryos were not completely cultured into blastocysts, blastocysts were successfully cultured in 52 of the remaining 68 cycles (76.5%), indicating that about one quarter of the retrieval cycles failed to culture blastocysts.
PGT-A results showed that 43 blastocysts (36.4%) were aneuploid, 56 blastocysts (47.5%) were euploid, and 19 blastocysts (16.1%) were mosaic.
Only 7 patients (22.6%) achieved successful pregnancy after the second transplantation, while the remaining 24 patients (77.4%) achieved successful pregnancy after the first transplantation. All patients included in this study delivered healthy live births without any abortions. In addition, both patients who received two-stage transplantation delivered twins.
The combination of PGT-A results and live birth rates indicates that although obtaining blastocysts through PGT-A may result in some loss of embryos, once qualified blastocysts are obtained, transplantation success and live birth rates are relatively optimistic.
Analysis of DE T-1 and Sho-ko-sen usage in patients included in the study
Among the patients included in the study, 10 cases (32.3%) used 3 packages of DE T-1 and 6 capsules of Sho-ko-sen, 18 cases (58.1%) used 4 packages of DE T-1 and 6 capsules of Sho-ko-sen, and 3 cases (9.7%) used 5 packages of DE T-1 and 9 capsules of Sho-ko-sen. It is considered that the patients had poorer baseline conditions and took higher doses after considering that more than 50% of patients took 4 packages of DE T-1 and 6 capsules of Sho-ko-sen. In this study, only the duration of treatment until pregnancy diagnosis was analyzed, which ranged from 4 to 45 months, with half of the patients taking it for at least 10 months. Additionally, most patients continued to take DE T-1 and Sho-ko-sen under guidance after obtaining positive pregnancy test results, and the related results were not included in the analysis of this study.
Analysis of the mechanism of DE T-1 and Sho-ko-sen
Mechanism of DE T-1: Dandelion is a traditional Chinese medicine that has a long history of use in Japan and China. Polysaccharides from dandelion have been studied extensively in recent years, and multiple studies have found that they have multiple functions such as antioxidant, anti-free radical, liver protection, hypoglycemic, growth factor secretion promotion, and anti-tumor activities. The main ingredient of DE T-1 is dandelion polysaccharide, which is a kind of amino sugar compound. Previous study [8,9], have shown that taking DE T-1 can improve the success rate of IVF-ET treatment and increase the live birth rate, and women of different ages and AMH values can benefit from it.
The mechanism may be that DE T-1 can significantly improve patients' blastocyst acquisition, allowing patients to have more blastocysts available for embryo transfer. FSH receptor is the only receptor present in granulosa cells. Studies [3,12], have shown that dandelion extract can increase the activity of receptors on granulosa cells surface and receptors for FSH, LH and other reproductive hormones, which may be related to promoting growth hormone secretion to increase the number of granulosa cells, delaying granulosa cell apoptosis, and promoting follicle development and ovulation. Its mechanism involves multiple organs, multiple pathways, and multiple targets. As relevant studies have been relatively extensive, no further analysis was conducted on patients' oocytes, embryos, and blastocyst culture in this study.
In addition, previous studies have shown that there are multiple receptors on the ovaries and uterine endometrium, which can be upregulated by DE T-1 to balance female reproductive hormone secretion [3]. Dandelion polysaccharides also have the ability to promote growth hormone secretion and related receptor activities [4,5], playing a role in oocyte growth, embryo implantation, and fetal development. Therefore, DE T-1 can promote high-quality fertilized egg production and blastocyst implantation, thereby increasing the live birth rate.
Mechanism of Sho-ko-sen: The main ingredient of Sho-ko-sen is pine polyphenols extracted from pine knots, which have antioxidant, anti-inflammatory, dilation of blood vessels at the end of the extremities, antiplatelet aggregation, promotion of peripheral circulation, strong connective tissue, improvement of the in vitro in vivo activity of vitamin C and its biological effects [10,13-15]. It was demonstrated that acute arithmetic stress-induced increases in sympathetic and parasympathetic nervous activity were detected by the autonomic nervous balance assay in the placebo group. However, such increases in sympathetic nervous activity were not observed in those who ingested Sho-ko-sen [16]. Our previous clinical observations have found that Sho-ko-sen can effectively improve the endometrial inflammation and endometrial blood flow in patients undergoing assisted reproduction treatment, enhance endometrial receptivity, regulate sleep disorders and anxiety, and improve the treatment results.
In summary, for patients with refractory infertility, under the premise of standardized IVF treatment, DE T-1 and Sho-ko-sen usage according to the standardized course and dosage may help to achieve satisfactory treatment results. Reproduction is a complex physiological process, and further studies are needed to explore the mechanism of DE-T1 and Sho-ko-sen on multiple targets of different organs such as the hypothalamus, pituitary gland, ovaries, and uterine endometrium. This study can provide a reference for future prospective clinical research.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Shao H, Ren J, Dong X, Wang L, Jiao S, Yanagihara N, et al (2024) Impact of the Combined Application of DE T-1 and Sho-ko-sen on the Outcomes of Assisted Reproductive Treatment in Refractory Infertile Populations: A Retrospective Study. J Clin Trials. 14:557.
Received: 20-Feb-2024, Manuscript No. JCTR-24-29693; Editor assigned: 22-Feb-2024, Pre QC No. JCTR-24-29693(PQ); Reviewed: 07-Mar-2024, QC No. JCTR-24-29693; Revised: 14-Mar-2024, Manuscript No. JCTR-24-29693(R); Published: 21-Mar-2024 , DOI: 10.35248/2167-0870.24.14.557
Copyright: © 2024 Shao H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.