Reproductive System & Sexual Disorders: Current Research
Open Access
ISSN: 2161-038X
ISSN: 2161-038X
Research Article - (2024)Volume 13, Issue 1
Background: Male Urinary Incontinence (UI) and Erectile Dysfunction (ED) significantly impact men's well-being, with UI prevalence experiencing a marked increase in recent years. While traditionally studied in women, UI's prevalence among men, particularly those over 60, has notably risen. UI types, such as urgency, mixed, and stress incontinence, often coincide with ED affecting the quality of life and overall sexual health.
Objective: This study aims to assess the safety and efficacy of the HIFEM procedure in improving male urinary function and erectile dysfunction. HIFEM, a novel non-invasive approach, targets pelvic floor muscles, focusing on intensifying and enhancing muscular contractions beyond traditional exercise modalities.
Methods: This pilot study involved 28 men, aged between 27 and 72 years, who were experiencing Urinary Symptoms (UI) and Erectile Dysfunction (ED). They participated in a structured treatment program that included ten weekly HIFEM therapy sessions. The severity of UI was measured using the International Prostate Symptom Score (IPSS), and the severity of ED was evaluated using the International Index of Erectile Function (IIEF). Additionally, penile ultrasound scans were performed both before and after the last treatment to assess changes in penile tissue. Of these participants, 20 men, aged 27 to 72 years and a median age of 57, had complete data from both the questionnaires and the ultrasound scans, and their results were analyzed.
Results: The study's findings indicated that 70% of patients experienced improvements based on the International Prostate Symptom Score (IPSS). After treatment, there were statistically significant (P<0.05) enhancements in urinary incontinence symptoms, notably a 46.2% reduction in the frequency of nighttime urination and a 38.2% improvement in urinary control. According to the International Index of Erectile Function (IIEF) questionnaire, patients reported a 37.0% improvement in maintaining an erection until the completion of intercourse, a 24.2% increase in satisfaction with sexual intercourse attempts, a 10.7% increase in ejaculating frequency, and an 18.9% increase in the frequency of experiencing orgasms or climaxes. Furthermore, penile ultrasound scans showed an increase (N=11) in the number and density of tissue segments after treatment (69.0%), suggesting an enhancement in erectile function.
Conclusion: While initial results are promising, further research is imperative to fully understand and optimize treatment protocols, ensuring maximized benefits and contributing to the holistic well-being of patients. The continued investigation into HIFEM's applications and outcomes will be crucial in solidifying its role in treating these common male health issues.
Erectile dysfunction; Male urinary incontinence; Pelvic floor muscle strengthening
Urinary Symptoms (UI) and Erectile Dysfunction (ED) are two prevalent health concerns in men, impacting not only their physical health but also their psychological and emotional wellbeing [1,2]. Traditionally, the epidemiology of Urinary Incontinence (UI) has primarily centered on women due to higher prevalence, but it's important to acknowledge that UI significantly impacts the quality of life for men as well, often requiring medical intervention [3-6]. From 2001 to 2020, the estimated prevalence of male UI doubled [7]. In 2017-2020, more than one-third of men aged 60 or older reported experiencing some kind of UI [7]. Urgency UI was the most common, affecting 31.3% of these individuals, followed by mixed incontinence at 10-30% and stress incontinence at less than 10% [7]. UI often carries a psychological and sexual burden and can be linked to Erectile Dysfunction (ED), particularly problems with penile erection [8,9].
Erectile dysfunction is diagnosed in more than 20% of men under 40, over 50% of men over 40, and more than 66% of men over 70 [10]. However, the exact prevalence of ED is still uncertain. Many affected individuals avoid seeking help due to feelings of guilt, shame, and fear associated with urological examinations, resulting in unreported cases [11-13]. Even when the root cause is physical, psychological consequences like marital issues, cultural norms, self-esteem loss, anxiety, and depression can persist. Both UI and ED significantly impact the emotional well-being and health-related quality of life for patients and their partners [14,15].
The first-line UI treatment is conservative management, which involves lifestyle changes, which is not easy to initiate or maintain (floor muscle training, bladder retraining, losing weight, etc.) [16-18]. For improving ED, pharmacotherapy with drugs based on blood supply improvement is common [19-22]. However, the efficacy depends on the root cause of ED and over time may decline due to progressive damage to small blood vessels [23]. Surgical intervention in both cases is not a suitable solution for every patient and introduces a great risk, especially for the elderly. Therefore, other methods including Pelvic Floor Muscle (PFM) exercises, or better blood circulation crucial for healing, are recommended [10,24,25].
In recent years, non-invasive technologies like shockwave therapy, Vacuum Erectile Devices (VED), or Electrical Stimulation (ES) have gained preference. Shockwave therapy is effective in tissue repair and vascular regeneration and is widely used in ED treatment. However, long-term studies confirming the safety of shockwave therapy are lacking, and therapy is directly applied to the treatment area without clothes contributing to the patient’s discomfort and shame associated with nudity. VED, despite the general satisfaction, can cause a lot of discomfort insufficient lubrication may lead to bruising, numbness and/or pain of the penis, cold sensation, and inability to ejaculate [26-28]. It can also cause some psychological discomfort to the patient, such as frustration and feelings of lack of autonomy [26-29]. The disadvantages of ES for ED treatment include a lack of a systematic and standardized treatment plan, a lack of sufficient clinical case verification, and the difficulty of applying individualized treatment for different causes [30]. PFM exercises may help to improve or alleviate UI and ED [31-33]. Nonetheless, the efficacy of PFM training always relies on the patient's commitment and physical abilities to perform correct PFM contractions.
This study introduces High-Intensity Electromagnetic Muscle Stimulation (HIFEM), a non-invasive technology designed to strengthen and enhance PFM function. HIFEM uses an alternating magnetic field to induce contractions in the skeletal muscles that are more intense and frequent than those achieved through voluntary contractions or biofeedback during PFM training. During the therapy, the patient is fully clothed, and that contributes to higher comfort, overcoming shyness, and better patient compliance. The objective of this pilot study is to assess the safety and effectiveness of HIFEM technology for treating male UI with ED using this innovative device and challenge the stigma surrounding intimate male health issues.
Recruitment of subjects
The target study population (up to 40 subjects) reflected the range of males with demonstrable UI symptoms accompanied by ED. Inclusion criteria were: Males between 21 and 80 years of age, willing to complete all study questionnaires and ultrasound, have intercourse at least once per week, and willing to complete ten (10) weekly-delivered treatments with a device utilizing HIFEM technology. Exclusion criteria included the known presence of untreated cardiovascular, respiratory, or infectious disease. Individuals were deemed unfit for study by the principal investigator due to possible inconsistencies in the patient profile provided by the developer company, e.g. metal-containing implants in the treatment area.
This study was approved by the Advarra Institutional Review Board, and its conduct adhered to the ethical principles of the 1975 Declaration of Helsinki. Informed consent was obtained from all patients. No study procedure was implemented before obtaining written informed consent from the subject. In addition, the subjects provided their consent for the use and disclosure of personal health information under the U.S. Health Insurance Portability and Accountability Act (HIPAA) regulations by signing a HIPAA authorization form.
Treatment protocol
The subjects received ten (10) 28-minute treatment procedures, delivered once a week, with a device utilizing HIFEM technology (Emsella, BTL Industries Inc, Boston, MA). Patients underwent treatment while fully clothed, in a sitting position on the device’s chair applicator. The magnet field power was adjusted according to the subject’s feedback collected during the therapy. During the whole therapy time, the operator communicated with the subject to get appropriate feedback on the therapy session.
Data collection, evaluation, and statistical methods
Evaluation of urinary symptom severity was done through the International Prostate Symptom Score (IPSS) survey. This selfreported psychometric questionnaire contains seven questions relating to different waterwork symptoms such as incomplete emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia. Each question is assigned points from 0 to 5 indicating increasing severity of the particular symptom. The total score can therefore range from 0 to 35 (asymptomatic to very symptomatic). Although there are no standard recommendations for grading patients with mild, moderate, or severe symptoms, patients can be tentatively classified according to IPSS as follows: 1-7=mildly symptomatic; 8-19=moderately symptomatic; 20-25=severely symptomatic.
ED severity evaluation was done through the International Index of Erectile Function (IIEF) survey. This questionnaire includes fifteen questions (with a score of 0-5 varying in individual domains) over the last four weeks and examines the four main domains of male sexual function: Erectile function, orgasmic function, sexual desire, and intercourse satisfaction [34].
In addition, penile ultrasound scans were taken at baseline and after the treatment. The ultrasound was transferred electronically to Morphometrix Imaging Technologies Inc., which is cloudbased software as a service company with revolutionary and disruptive medical function software Tissue Segmentation Technology which is applied to ultrasound images. The Tissue Segment Counts (TSC) are counted, tabulated, and presented as visual images, as graphical displays, and in data format available for further analytics. The algorithm also computes the Cross- Sectional Area (CSA) of the tissue selected in each frame of a cine loop and computes a Tissue Segment Density (TSD).
Two visits, baseline, and post-treatment, were performed in addition to the treatment visits in this study. The comfortability and safety of the treatment were monitored during all treatment visits and patient satisfaction was assessed. A paired t-test was used to statistically analyze the significance of intragroup differences between pretreatment and posttreatment (α=0.05).
This observational study followed adult men with diagnosed urinary symptoms accompanied by erectile dysfunction undergoing HIFEM treatment for strengthening pelvic floor muscles. Twenty-eight (28) males were recruited for this study and received the treatment. Twenty (20) patients (27-72 years, median of 57) had complete data in both questionnaires and ultrasound scans and were admitted for study evaluation.
IPSS questionnaire
At baseline, moderate symptoms of urinary incontinence were documented by a total average value of 9.9 ± 1.6 points from the IPSS questionnaire, with intermittency, nocturia, frequency, and weak stream symptoms as the most problematic. After the treatment, patients' symptoms significantly (P<0.05) improved to mildly symptomatic (6.7 ± 1.1 points, N=20). In all examined question categories (Incomplete emptying, Frequency, Intermittency, Urgency, Weak stream, Straining, and Nocturia), an IPSS score decrease was detected, as shown in Figure 1. Patients reported the most prominent changes in not getting up so often to urinate during the night (46.2%), less intermittent while urinating (38.2%), and less overall urinating frequency (30.0%).
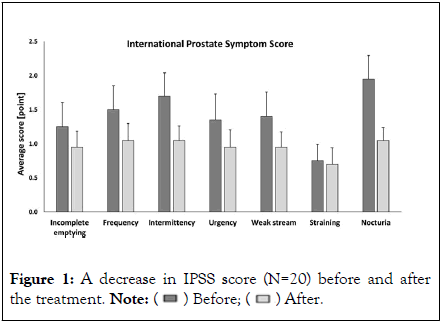
Figure 1: A decrease in IPSS score (N=20) before and after
the treatment. 
In addition, the improvement was supported by achieving the Minimal Clinically Important Difference (MCID in the range of 3-8 points for IPSS) representing the effect delivered by the treatment procedure is apparent and clinically meaningful [35,36]. These outcomes related to UI improvement correspond to studies in women confirming the positive effect of HIFEM treatment on pelvic floor strengthening [37-40]. The HIFEM studies focusing on men’s UI problems are in ascension, varying in the field of indication e.g., non-invasive treatment of UI after prostatectomy.
IIEF questionnaire
Based on the IIEF data evaluation, the patients mainly improved (P<0.05) in sexual desire, orgasmic function, and erectile dysfunction domains, noticing a better ability to maintain the erection to completion of intercourse (37.0%), higher satisfaction with attempting sexual intercourse (24.2%), ejaculating frequency (10.7%), and having the feeling of orgasm or climax more often (18.9%). These outcomes suggest. PFM strengthening may play an important role in ED treatment [33]. However, IIEF assessment is limited by the superficial assessment of psychosexual background and the very limited assessment of partner relationships, both important factors in the presentation of male sexual dysfunction [34]. Based on the low intercourse satisfaction and overall satisfaction domain outcomes, psychosexual counseling should be considered. In the case of the erectile dysfunction domain score, consideration of the trial course of therapy with the medication is not yet needed. Moreover, despite traditional management, addressing the underlying pelvic floor muscles appears to be beneficial. Reduction in tone and alterations in contractile patterns may directly impact erectile strength and the ejaculatory process [33].
Contraction of the external penile muscles, ischiocavernosus muscle, and bulbospongiosus muscle, which are part of the male pelvic floor, leads to increased pressures in the corpus cavernosum. Its strengthening helps to stabilize the erect penis by compressing the crus penis and retarding the return of blood through the veins, so it appears to be beneficial in men with ED due to mild or moderate veno-occlusive dysfunction [41,42]. However, abnormally high PFM tone causing the spasm can provide extrinsic compression that restricts the lumen of the internal pudendal artery and thereby limits internal pudendal arterial inflow [42]. It is necessary to find a balance in the suitable treatment of ED involving PFM.
Ultrasound images
Transverse B-Mode ultrasound video scans were recorded along the long axis of the penile shaft from the tip to the base with the penis in a flaccid state. A linear transducer was used, the depth was set at 2 cm and the frame rate was approximately 30 frames per second. Copious amounts of ultrasound gel were applied to the top side of the penile shaft. The transducer was positioned on the top side of the shaft at the tip, perpendicular to the shaft. The transducer was moved along the shaft from the tip to the base at a steady rate keeping it perpendicular to the shaft. Separate video recordings of the left and right cavernosa were taken. The video scans were then processed through the Morphometrix algorithm which can assess penile vascularity in the flaccid state through the use of Tissue Segment Counts (TSC). TSC, CSA, and TSD were counted in all twenty (20) patients.
It was already described 43, that the corpus cavernosum of the penis is composed of a meshwork of interconnected smooth muscle cells lined by vascular endothelium. Of note, endothelial cells and underlying smooth muscle also line the small resistance helicine arteries that supply blood to the corpus cavernosum during penile tumescence [43]. Indeed, normal penile erection requires coordinated arterial endotheliumdependent vasodilation and sinusoidal endothelium-dependent corporal smooth muscle relaxation [43]. The smooth muscle and endothelial cells form the corpora cavernosa's vascular compartment and are essential for erectile function. The loss or dysfunction of these cells is thought to have a central role in the pathophysiology of erectile dysfunction [44].
After the treatments, tissue segmentation showed an increase in TSCs (103.7%) and CSAs (25.6%) in 11 patients, resulting in increased TSD (69.0%). These outcomes suggest increased blood flow from the internal pudendal artery (besides the dorsal and bulbourethral arteries, the internal pudendal artery branches into the cavernous arteries, which supply the spongy trabecular tissues trapping the blood during erection) due to HIFEM stimulation of pelvic floor muscles and contribute to neovascularization of corpus cavernosum endothelial tissue. Higher blood supply of trabecular meshwork of smooth muscle leads to improvement of ED (the most prominent improvement is shown in Figure 2 [45].
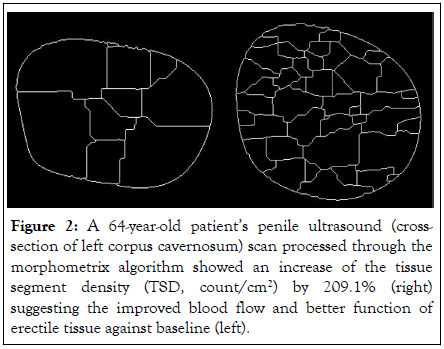
Figure 2: A 64-year-old patient’s penile ultrasound (crosssection of left corpus cavernosum) scan processed through the morphometrix algorithm showed an increase of the tissue segment density (TSD, count/cm2) by 209.1% (right) suggesting the improved blood flow and better function of erectile tissue against baseline (left).
With vascular regeneration, tissue repair and consecutive expression of neuronal NO synthase are promoted in endothelial, smooth muscle, and nerve cells [46,47]. This corresponds with outcomes of Nehra, et al., study, suggesting that erectile function is better preserved in patients whose endothelial cell and smooth muscle content is higher and declines as its content diminishes [48]. Also, Luo, et al., demonstrated that corpora expandability is related to the percent corporal smooth muscle content as an important predictor of corporal veno-occlusive function [49].
Similarly, a reduction in the number of smooth muscle cells has been demonstrated in relation to aging causing a decrease in penile oxygen tension [50]. However, blood flow arterialization during erections is felt to be crucial in providing the free oxygen necessary for the formation of NO by neuronal and endothelial nitric oxide synthase [51]. By neovascularization increasing the trabecular smooth muscle content and blood supply, the amount of oxygen in the area increases and helps to regulate nitric oxide synthesis in corpus cavernosum tissue and prevent the progression of ED [52-54].
In summary, this study highlights HIFEM's effectiveness in improving urinary symptoms and erectile dysfunction in men. Enhanced pelvic floor strength correlated with symptom alleviation, validated by questionnaires and ultrasound findings. While promising, further research with larger cohorts and longer-term follow-ups is crucial to confirm its lasting impact on men's health. In conclusion, HIFEM therapy may represent a significant advancement in the non-invasive treatment of male urinary incontinence and erectile dysfunction. Its ability to effectively strengthen pelvic floor muscles and improve pelvic region functions without the need for surgical intervention highlights its potential in clinical settings.
The HIFEM procedure belongs to the magnetic stimulation family and has three major advantages it can stimulate deeper than electrical stimulation, it can be done non-invasively while the patient is fully clothed, and it is considered a safer option with fewer side effects. Moreover, the HIFEM procedure focuses on the cause of the problem and not on the treatment of symptoms only as a pharmaceutical treatment and promises long-term results (best up to 6 months) as was already evidenced in studies for female UI and sexual function connected with PFM dysfunction. However, the mechanism of HIFEM treatment for ED is still unknown and future studies are needed. The biggest limitation of this study was defining the key subject. Most men are still unwilling to solve their intimate problems due to shyness. Also, greater emphasis should be placed on the uniformity of patients' indications and the specification of inclusion criteria, including age or medical history, because ED has various sources of causes and manifestations during different illnesses such as diabetes, cardiovascular disease, etc. A higher number of subjects should be enrolled and monitored for longer follow-up visits to observe the changes in the strength of PFM in the long term. In addition, the algorithm for assessing the ultrasound scans was primarily developed to characterize lesions in equine tendons and has been extended to characterize the tissue segments in a variety of organs. However, the results suggest that tissue segmentation is an excellent proxy for vascular and neovascular density in the tissue, provides information about the entire penis, and is less operator-dependent.
Urinary symptoms and ED are often accompanied by each other and can be both addressed by the HIFEM procedure. A combination of unbiased and balanced objective observations including valid questionnaires was used to assess the changes in urinary symptoms and ED severities. The effectiveness of HIFEM is now observed in both genders.
None.
The researcher confirms that there are no conflicts of interest regarding this study. The research presented here is entirely the result of the investigator's initiatives. It should be noted that the investigator sometimes acts as a speaker for BTL Industries and may potentially present or discuss this study in a capacity associated with BTL Industries.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Brandeis J (2024) Improving Male Pelvic Health: Efficacy of HIFEM Muscle Stimulation for Urinary Function and Sexual Dysfunction in Men. Reprod Syst Sex Disord. 13:401.
Received: 24-Jan-2024, Manuscript No. RSSD-24-29325; Editor assigned: 29-Jan-2024, Pre QC No. RSSD-24-29325 (PQ); Reviewed: 16-Feb-2024, QC No. RSSD-24-29325; Revised: 23-Feb-2024, Manuscript No. RSSD-24-29325 (R); Published: 01-Mar-2024 , DOI: 10.35248/2167-0250.24.13.401
Copyright: © 2024 Brandeis J. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.