Journal of Medical & Surgical Pathology
Open Access
ISSN: 2472-4971
ISSN: 2472-4971
Review Article - (2021)Volume 6, Issue 8
The ophthalmologist often relies on the optometrist to receive patient referrals for retinal pathologies that need further investigation. However, both the optometrist and non-surgical retina specialist ophthalmologist, may often only have the tools available to assess the fundus and posterior pole while peripheral pathologies may go unnoticed yet may pose a strong threat to cause serious loss of vision or even blindness or need of surgery for the patient in the near or later future. In addition, mid and peripheral vitreoretinal pathologies are usually difficult if not impossible to visualize unless you use Indirect ophthalmoscopy ideally with 360-degree Scleral Indentation and thus, may go undiagnosed.
Mid and peripheral retina and vitreoretinal interface abnormalities span a wide range of conditions from incidental ophthalmoscopic findings that require monitoring.
Non-surgical; Retina; Ophthalmoscopic findings
A full vitreoretinal examination involves an assessment of the retina up to the ora serrata. This can only be achieved by performing a biomicroscopy in combination with indirect ophthalmoscopy with 360° Scleral Indentation (f. ex. Topcon PS12 indirect ophthalmoscope, Topcon corporation, Tokyo, Japan), a Pan Retinal® 2.2 hand-held lens (Volk optical, OH, USA) and a handheld scleral depressor (E5106, Storz, St Louis, USA). While the patient is placed in a supine position for increased patient comfort, the peripheral retina is examined in all clock hours. This assessment goes beyond any type of Ultra-Widefield Imaging to visualize the Retina [1]. To date, there is no Optical Coherence Tomography (OCT) nor ultra-widefield imaging technology that reaches the retinal Ora Serrata. Indirect ophthalmoscopy with Scleral Indentation is outside the remit of Optometrists. Hence, Slitlamp Biomicroscopy and perhaps ultra-widefield imaging often remains the only vitreoretinal assessments carried out at optometric and non-surgical retina specialist ophthalmologist’s practices. Where available, standard OCT devices may complement visualization of the posterior pole to screen for vitreoretinal conditions such as vein or artery occlusions, age-related macular degeneration, diabetic macular oedema, macular holes and epiretinal membranes, amongst others. However, usually areas of only 45° may be visualised up to a depth of only 2.6 mm, thus not allowing to collect sufficient information about the peripheral neuroretina and vitreoretinal Interface. This poses the risk of underdiagnosing mid and peripheral vitreoretinal abnormalities.
Multi-Wavelength Ultra-Widefield Imaging (MW UWFI) (California Optomap®, Optos® plc, Dunfermline, Scotland, UK) uses short and long wavelength light sources to visualise the mid and peripheral Retina either as a pseudo-colour image, or in the optional auto-fluorescent mode [2]. This ultra-widefield imaging technique allows for a field of view of up to 200°C and thus greatly improves the potential to diagnose vitreoretinal pathologies beyond the Posterior Pole, specially located in the mid and peripheral retina and vitreoretinal interface [3]. However, not only this imaging technology does not reach up to the ora serrata but actual vitreous anatomy and the vitreoretinal interface cannot be fully assessed with this technology as cross sectional imaging is necessary [4,5]. Display of imaging results in 2D which does not allow clinical assessment beyond the inner retinal layer (retinal surface) in order to differentiate pathologies as to their exact depth-location within the retina.
Optical Coherence Tomography (OCT) is a relatively new revolutionary non-invasive user-friendly retinal imaging technology which provides high-resolution cross-sectional information of the vitreous, retina, and choroid [6]. However, currently commercially and clinically available OCT systems can only image a small area because of the relatively short scan length, or they must resort to montages of multiple images that invariably result in registration artefacts [7]. Hence, due to the limited field of view, they are commonly used only for the assessment, diagnosis and management of diseases that primarily affect the posterior pole such as age-related macular degeneration, diabetic macular oedema, macular oedema in vein occlusion, epiretinal membrane, or macular holes [8].
Currently commercially available OCT technologies are not able to image the peripheral neuroretina and vitreoretinal interface with enough field of view and resolution nor provide 3D information of peripheral anatomical features [9].
The Canon Xephilio® S1 Widefield Swept Source Optical Coherence Tomography (SS-OCT) obtains non-invasive Single-Scan 3D captures which provide a cross-sectional view of the vitreous, retina and choroid with no depth-dependent loss of sensitivity across the images from the cortical vitreous to the choroid. This new technology performs 23 mm × 20 mm scans with an 80° viewing angle and a depth of 5.3 mm thus allowing high contrast and resolution visualisation from the cortical vitreous all the way through to the Sclera. It uses infrared illumination (1010-1110 nm) and allows to capture 100,000 A-scans per second. Being singlescan this eliminates the need to montage multiple images which would often result in registration artefacts and optical distortion [10,11].
We received this new and innovative OCT technology on December 20, 2019 and now routinely use it at “The Retina Clinic London” and therefore decided to carry out a retrospective study of our findings.
Our just published paper shows, to the best of our knowledge, the first successful 3D and cross-sectional Widefield imaging of peripheral vitreoretinal features [12,13].
Our imaging results are also supported by the correlation to Multi-Wavelength Ultra-Widefield Imaging (MW UWFI) and Histopathology reference where available.
Some retinal pathologies in the mid or peripheral retina or vitreoretinal interface initially may only require monitoring. A number of these pathologies can be commonly observed in the myopic patient, whose retina is constantly exposed to shear forces due to the elongated eyeball. Amongst these we observed white without pressure, lattice degeneration, peripheral retinoschisis, choroidal nevus, ora serrata pearls, vitreoretinal tuft, snail track, cobblestone degenerations and peripheral laser retinopexy (See Figures 1-7 for clinical examples). In the case of peripheral retinoschisis, for example, WF SS-OCT is an excellent technology which can highlight the cleavage between retinal layers and bridging elements thus differentiating the lesion from retinal detachment and avoiding unnecessary treatment in the form of laser retinopexy or surgery. In the case of vitreoretinal Tuft, WF SS-OCT can assist in differentiating between retinal tear or hole and rule out a vitreoretinal attachment or traction. In the case of a Rhegmatogenous Subclinical Retinal Detachment (SRD) (a Retinal Tear or Hole with surrounding subretinal fluid not extending further than two disc diameters), for example, this new imaging technology allows for the diagnosis of new findings and their objective recording for when Monitoring is decided. We have also found this new technology to be especially useful for the assessment of the status of the Vitreous, Vitreous Opacities and Posterior Vitreous Detachment (PVD). The use of longer scans (23 mm) is particularly helpful to diagnose or rule out PVD, as we can image beyond the posterior pole and with navigation, even close to the ora serrata. Both with age or in the myopic or high myopic eye, the vitreous undergoes structural changes becoming liquefied with collagen fibres tending to cluster together. These clusters can form aggregates so thick that they will eventually become visible for the patient as vitreous opacities secondary to vitreous floaters (myodesopsia) or PVD. Vision Degrading Myodesopsia (VDM) is the loss of Contrast Sensitivity as a result of Vitreous Opacities.
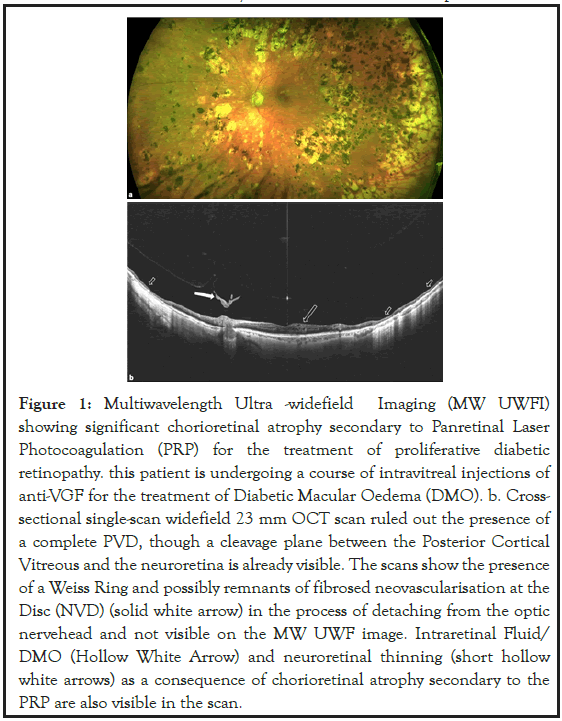
Figure 1: Multiwavelength Ultra -widefield Imaging (MW UWFI) showing significant chorioretinal atrophy secondary to Panretinal Laser Photocoagulation (PRP) for the treatment of proliferative diabetic retinopathy. this patient is undergoing a course of intravitreal injections of anti-VGF for the treatment of Diabetic Macular Oedema (DMO). b. Crosssectional single-scan widefield 23 mm OCT scan ruled out the presence of a complete PVD, though a cleavage plane between the Posterior Cortical Vitreous and the neuroretina is already visible. The scans show the presence of a Weiss Ring and possibly remnants of fibrosed neovascularisation at the Disc (NVD) (solid white arrow) in the process of detaching from the optic nervehead and not visible on the MW UWF image. Intraretinal Fluid/ DMO (Hollow White Arrow) and neuroretinal thinning (short hollow white arrows) as a consequence of chorioretinal atrophy secondary to the PRP are also visible in the scan.
Figure 2: Section of a MW-UWI to highlight one retinal tear (solid white arrow) and a retinal hole (hollow white arrow) in an area of peripheral retinal lattice. b. Radial scan pattern used and navigated peripheral cross-sectional OCT scans confirmed the presence of a Retinal Tear. Most importantly, the scans not only confirmed that the Retinal Hole (Solid White Arrow) was full-thickness but also revealed the presence of an elevated retina with Subclinical Retinal Detachment (SRD) and vitreous attachment/traction (hollow white arrow), possibly indicating the High Risk of progression. c. Peripheral Topography Map showing the area of SRD around to the retinal tear (solid white arrow). Cross-sectional scans showing vitreous attachment (solid white arrow).
Figure 3: MW-UWI shows Laser retinopexy carried out elsewhere around area of peripheral retinal lattice that was believed to be an area of retinal detachment secondary to a Retinal Tear. Inferiorly, a round area of onedisc diameter and compatible with pre-retinal fibrosis was noted (Solid White Arrow). b. Cross-sectional scans revealed the absence of retinal hole/ tear and the presence of a vitreous attachment (Solid White Arrow). c. 3D Rendering of navigated peripheral OCT scans showed a visually striking and elevated lesion compatible with a large vitreoretinal tuft (Solid White Arrow) with a vitreous attachment (Hollow White Arrow).
Figure 4: MMW-UWI showing a “cloudy ” Vitreous after a Haemorrhagic PVD (Solid White Arrows), a weiss ring and a peripapillary choroidal nevus. b. Cross-sectional scans confirmed the presence of a PVD, showed a Weiss Ring (Solid White Arrow) and Red Blood Cells (RBC) (Hollow White Arrow) in the detached posterior cortical vitreous. c. 3D Rendering showing PVD and an enhanced hyper-reflective posterior cortical vitreous due to the presence of RBC (Solid White Arrow).
Figure 5: MMW-UWFI showing an Argus II® Electronic epi-retinal implant (“Bionic Eye”) (Solid White Arrow) in a patient with advanced retinitis pigmentosa, implanted by PES, 9 years prior to these scans being obtained (the vertical red line is an artifact due to eye movement). b. MWUWFI Fundus autofluorescence highlighting typical features of the disease as well as the array of electrodes. c. Cross-sectional OCT scans showing the presence of a separation (Hollow White Arrow) between the Array and the neuroretina and not visible on biomicroscopy. The scans also show generalized retinal thinning (Solid White Arrow), Degenerative Intraretinal Changes (Short Solid White Arrow) and remnants of detached Internal Limiting Membrane (ILM) (Short Hollow White Arrows) (the vertical white lines are artifacts).
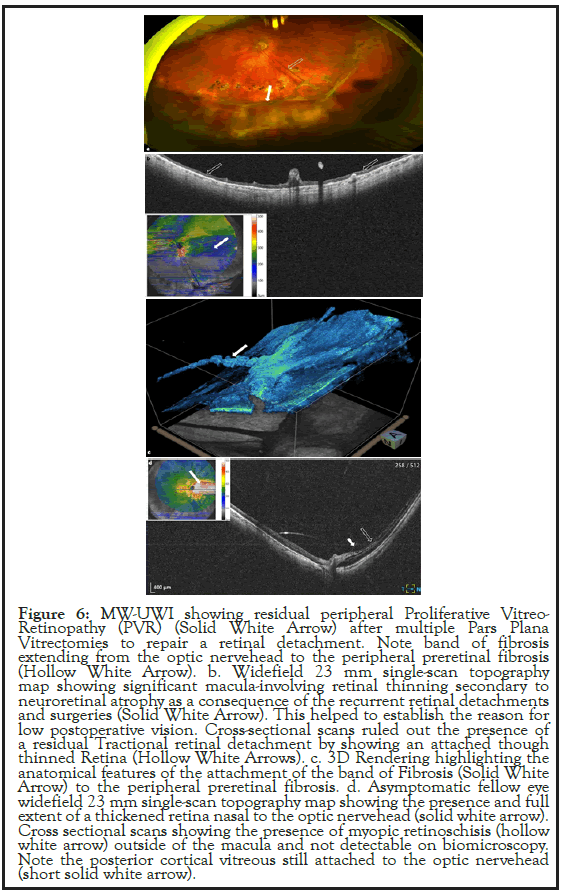
Figure 6: MW-UWI showing residual peripheral Proliferative Vitreo- Retinopathy (PVR) (Solid White Arrow) after multiple Pars Plana Vitrectomies to repair a retinal detachment. Note band of fibrosis extending from the optic nervehead to the peripheral preretinal fibrosis (Hollow White Arrow). b. Widefield 23 mm single-scan topography map showing significant macula-involving retinal thinning secondary to neuroretinal atrophy as a consequence of the recurrent retinal detachments and surgeries (Solid White Arrow). This helped to establish the reason for low postoperative vision. Cross-sectional scans ruled out the presence of a residual Tractional retinal detachment by showing an attached though thinned Retina (Hollow White Arrows). c. 3D Rendering highlighting the anatomical features of the attachment of the band of Fibrosis (Solid White Arrow) to the peripheral preretinal fibrosis. d. Asymptomatic fellow eye widefield 23 mm single-scan topography map showing the presence and full extent of a thickened retina nasal to the optic nervehead (solid white arrow). Cross sectional scans showing the presence of myopic retinoschisis (hollow white arrow) outside of the macula and not detectable on biomicroscopy. Note the posterior cortical vitreous still attached to the optic nervehead (short solid white arrow).
Figure 7: MMW-UFI showing inferior pigmented lesion (Solid White Arrow) in a patient suffering from symptoms of acute PVD. Pigmented retinal tear needs to be ruled out. b. Cross-sectional scans showing a PVD (Solid White Arrow). c. Scan pattern used and inferior navigated crosssectional scans showing a vitreoretinal tuft with a vitreous attachment (Solid White Arrow). The scans ruled out any associated retinal tear or hole and therefore the need of treatment. d. Asymptomatic fellow eye cross-sectional scans showing a partial posterior pole-only PVD (Solid White Arrows) with the vitreous still attached to the optic nervehead (Hollow White Arrow). The patient needs to be made aware of a possible near future Fellow Eye PVD, its symptoms and the need of a full vitreoretinal examination at the time.
Yag Laser Vitreolysis and Limited Vitrectomy are new management options.
A full vitreoretinal assessment is essential in all patients suffering from symptoms of Acute PVD such as change in or new vitreous floaters and/or flashes of light (photopsia) in order to rule out retinal tears. for this, the retina needs to be examined up to its edge, the ora serrata, and the only way to achieve this is by doing indirect ophthalmoscopy with 360° Scleral Indentation. It is our routine practice for all our patients presenting with symptoms of acute PVD to undergo Optos® MW UWFI, Canon Xephilio® S1 Navigated OCT imaging and indirect ophthalmoscopy with 360° Scleral indentation in a supine position. All these examinations are performed through fully dilated pupils.
WF SS-OCT has become essential in our practice, successfully assisting in the diagnosing of peripheral vitreoretinal pathologies and that of PVD. This new technology has also become essential to diagnose PVD in the fellow eye and therefore counsel the patient appropriately as towards the risk of PVD in the Fellow Eye and need, at the time, for a full vitreoretinal examination if symptomatic.
This technology is particularly helpful when the examiner comes across peripheral retinal pathologies that need monitoring such as peripheral Retinal Lattice that is superior and in the presence of an ongoing symptomatic PVD. Without the timely referral by the optometrist or non-surgical retina specialist ophthalmologist, such peripheral pathologies or Vitreous changes may quickly become problematic for the patient.
WF SS-OCT, as described above, has shown to provide managementchanging anatomic information that is otherwise not detectable with neither biomicroscopy nor indirect ophthalmoscopy.
WF SS-OCT has proven to allow early recognition of peripheral vitreoretinal pathologies needing treatment, thus reducing the risk of retinal detachment and thus potentially reducing the number of patients needing surgery. In our experience, using this new OCT technology (WF SS-OCT) and scanning technique (Navigation), it is possible to obtain high-quality and clinically meaningful images of the peripheral retina and vitreoretinal interface that are helpful in the decision-making process of indicating timing for a referral, whether urgent or not, or treatment particularly in an era of telemedicine or when there is limited or no access to a surgical retina specialist ophthalmologist and/or indirect ophthalmoscopy with 360°C Scleral Indentation.
Citation: Stanga PE, Reinstein U, Bashir NF, Zahavi O (2021) Improving the Accuracy of Mid and Peripheral Retina Pathology Referrals and Indication of Treatment. J Med Surg Pathol. 6:227.
Received: 04-Oct-2021 Accepted: 18-Oct-2021 Published: 25-Oct-2021 , DOI: 10.35248/2472-4971.21.6.227
Copyright: © 2021 Stanga PE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.