Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Research Article - (2012) Volume 0, Issue 0
Risk for and progress of Coronary Heart Disease (CHD) can be influenced by minimizing modifiable risk factors. CHD patients were assigned to an intervention (IG) or control group (CG). A brief activating health-psychological intervention based on the Health-Action-Process-Approach (HAPA) was build into an educational group setting about heart-healthy nutrition. Patients were encouraged to make an action and coping plan for their future nutrition. Baseline assessment included perceived self-efficacy, intentional status, food consumption; follow-up data were collected two and six months after discharge. In total 201 patients participated (IG:N=143; 62±11.3 years, 64.3% male; CG:N=58; 64±10.3 years, 77.6% male). The IG reported a higher increase in vegetable fat consumption from baseline to two months (p<.05) and in low fat food and fish consumption from baseline to six months (both p<.01). Overall the program was feasibly to be carried out in an acute cardiac care hospital ward. One brief intervention based on the HAPA model could only change some dietary habits over a short period of time; follow-up sessions are necessary to have a larger impact on a wider set of dietary variables and habits over the long term.
Keywords: Health education program; Health psychology; HAPA model; Cardiology; Nutrition; Intention-behaviour gap; Coronary heart disease
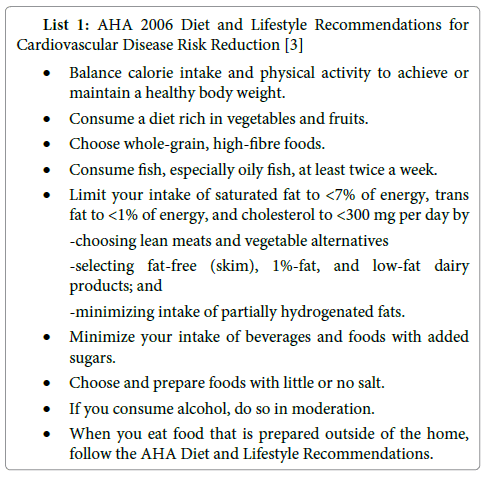
Coronary Heart Disease (CHD) as the most frequent cause of death in western countries [1] is primarily a lifestyle related disease. Several modifiable risk factors have been identified [2] and one of them is nutrition. Diet and lifestyle recommendations to reduce the risk for cardiovascular disease have been developed i.e. by the European Society of Cardiology, the German Association of Cardiology and the American Heart Association (AHA, List 1) [3].
Although the knowledge of physicians, patients and society in general about risk factors for CHD is increasing, the uptake of a healthy lifestyle is not. Clinical routine and patient briefings do not necessary improve patients’ knowledge on cardiovascular risk factors [4,5]. One explanation for that dilemma is motivational and volitional aspects in patients behaviour.
Since the early seventies several health psychological theories tried to explain how to change health behaviour and to identify the main factors having an effect on the process of changing health behaviour [6]. One of them, the Theory of Reasoned Action (TRA) [7] is derived from social psychology and was developed to explain the relationship between attitude and behaviour. The Theory of Planned Behaviour (TPB) [8,9] poses an enhancement of the TRA. The TPB proposes that intention is a predictor of behaviour. Intention on its part is influenced by attitude, social norms and perceived behavioural control.
Though many of these models of health behaviour see intention as the beginning of the health behaviour changing process, it isn’t a sufficient predictor for a behavioural change [10]. The Health Action Process Approach (HAPA) [6,11] is addressing this intention behaviour gap. The HAPA model assumes that health behaviour is consisting of two consecutive phases, the motivational phase and the volitional phase (Figure 1). In the motivational phase the intention to change health behaviour is formed. The intention development is influenced by three factors. It often starts with the emergence of certain risk awareness. Subsequently the positive and negative consequences of a behavioural change (outcome expectancies) are balanced. The third factor is the perceived self-efficacy to be able to develop a behavioural intention. Self efficacy was introduced in the social-cognitive theory of Bandura [12]. Self efficacy describes the self-conception of one’s own competence, to act out behaviour even if obstacles or difficulties are occurring. A cardiac patient for example may realise that heart-healthy nutrition would be good for him, but he doesn´t believe to be able to eat healthy for a long time. This is interpreted as a lack of self-efficacy.
Once an intention for the uptake of a healthy behaviour is formed, the motivational phase is considered complete. In the following volitional phase the intended behaviour has to be initiated, maintained for the longer term and restarted in case of setbacks. Like a few other theories [13,14] the HAPA model determines planning as essential intermediate step connecting intention and behaviour.
The HAPA model was applied in numerous studies on changing health behaviour, most frequently to examine the realisation of physical activity. Scholz and Sniehotta [15] tested the effectiveness of a planning and action control intervention on physical activity in 199 cardiac patients after rehabilitation. One year after discharge the patients in the intervention group were significantly more physically active than the control group.
A study of Sniehotta, Scholz and Schwarzer [16] on 307 cardiac rehabilitation patients confirmed planning, maintenance self-efficacy and action control to be mediators between exercise intentions and physical activity 4 months later. Another longitudinal study of Sniehotta et al. [17] on 352 cardiac patients showed that patients with higher levels of coping planning reported higher levels of exercise four months after discharge. In a longitudinal study on 443 orthopedic rehabilitation patients Ziegelmann et al. [18] found that baseline physical activity, action planning and coping planning are predictors for physical activity six months after discharge.
The HAPA model also has been applied in predicting nutrition behaviour change. Gutiérrez-Dona et al. [19] found that people have to dispose of sufficient self-efficacy for planning to be a mediator of the intention-behaviour relation. Renner et al. [20] showed self efficacy, intentions and planning to be predictors of a healthy diet particularly in South Korean women (N=358). A self-efficacy and a combined self-efficacy and action planning group both improved their fruit and vegetable consumption equally at 6 months in comparison to the control group (p<.01), as showed in a study by Luszczynska et al. [21]. To examine whether the intention-behaviour association is mediated by planning, Reuter et al. [22] used an experimental-causal-chain design to examine the association between intention and behaviour mediated by planning. In a first study on 304 healthy employees of a large service company who reported a lower than five portions a day fruit and vegetable consume per day were either assigned to a motivational intervention based on the HAPA model or a control group. The measurement of intentions and planning concerning fruit and vegetable consumption showed a significant increase of action planning in the intervention group after one month (p<.05). In a second study 246 participants with the intention to increase their fruit and vegetable consume were assigned to a planning intervention. One month later appeared a difference in dietary behaviour between intervention and control group (p=.08).
The aim of the present study was to investigate if a health education program for heart healthy nutrition based on the HAPA model is able to influence patients’ diet in a positive way over a 2-6 months period.
Study design
Following ethics committee approval inpatients with documented CHD and identified cardiac risk factors were approached at the Cardiology ward of the University hospital Innsbruck. Before implementing the intervention on the ward a control group was recruited. Patients of the intervention and the control group signed an informed-consent and both filled out the same battery of questionnaires (t0) at the time of recruitment. Postal follow-up data were collected two (t1) and six months (t2) after discharge (Figure 2).
Instruments
Data on sociodemografic and clinical variables were collected and patient charts were reviewed. Self reported risk factors such as smoking, diabetes, hypertension, hypercholesterolemia and depression were collected. The battery of questionnaires consisted of the following instruments:
General self efficacy (GSE): The German version of the GSE is a self-administered 10 item questionnaire designed to asses a general sense of perceived self-efficacy. The originally scale was developed by Jerusalem and Schwarzer in 1979, and later revised and adapted for 33 languages [23]. One of the items is “I can always manage to solve difficult problems if I try hard enough”, responses are made on a 4-point scale in the format “Not at all true”, “Hardly true”, “Moderately true” and “Exactly true”. A composite score is available with higher scores reflecting higher GSE. In numerous research projects the GSE demonstrated internal consistencies between α=.75 and .91 [24], in all of the german samples between .80 and .90 [25]. Criterionrelated validity is well documented [26]. Representative norms are available [27].
Measurement of intention, action and coping planning and action control: Items on the intention, action planning, coping planning and action control for a heart healthy diet were adapted from Sniehotta et al. [17]. The items have been processed using a 4-stage response format from 1 (not at all true) till 4 (exactly true). A higher sum score reflects higher intentions, action and coping planning or action control.
Intention: The intention for a heart healthy diet was assessed with six intentional statements. The item stem, “I intend to...” was followed for example by “...eat regularly food, which is healthy and good for my heart”.
Action planning: Action planning was assessed by means of 5 items. The stem “I have made a detailed plan regarding...” was followed by the items (a) ”...when to follow a balanced diet,” (b) “...where to follow a balanced diet,” (c) “...how to follow a balanced diet,” (d) “... how often to follow a balanced diet,” (e) “...with whom to follow a balanced diet”.
Coping planning: Coping planning was assessed with five items, for example: “I have made a detailed plan regarding...” “...what to do if something interferes with my plans,” or “...how to cope with possible setbacks”.
Action control: Action control was assessed by means of 6 items using two items for each facet: self-monitoring, awareness of standards and self-regulatory effort [28]. The items were introduced by the stem “During the last 4 weeks I have...” (a) “...consistently monitored myself whether I often subsist myself balanced,” (b) “...taken care to eat 2-3 times fish a week,” (c) “...often had my diet intentions on my mind,” (d) “...always been aware of my planned diet intentions,” (e) “...really tried hard to eat balanced regularly,” (f) “...done my best to act in accordance to my standards.”
Self reported items on diet: Diet satisfaction and perceived impact of diet on health were assessed by two items deriving from the German questionnaire on health behaviour (FEG) [29]. Responses on the two questions “How comfortable are you with your diet?” (Diet satisfaction) and “How does your diet affect your health?” (Impact of diet on health) are made on a 7 point scale from “extremely dissatisfied/ negative” (-3) to “extremely satisfied/positive” [3].
Food frequency questionnaire (FFQ): On account of the project construction we decided on the direct nutrition information assessing method [30] and assessed the last food consumption with food frequency lists. FFQs reflect the average consumption of certain food or food groups over a certain period of time. This kind of questionnaire provides information about the frequency of food-consumption and also about the serving size [31].
There are some different FFQs available. In the USA the Health Habits and History Questionnaire, the Harvard University Food Frequency Questionnaire and the NCI`s diet History questionnaire are widely used [31]. In Europe the interdisciplinary test kit from Ardelt- Gattinger et al. for diagnostics and evaluation of obesity and other lifestyle diseases such as diabetes, coronary heart disease, etc. is common [32]. Based on existing items [33] we designed an individual FFQ covering the relevant aspects of a heart healthy diet. The food frequency list contained questions about the consumption of low fat and rich food (meat, sausage, cheese and milk products), fish, alcoholic drinks and coffee, soft drinks and fruit juice, water, food with and without dietary fibre, eggs and vegetable fat. Patients had to estimate how often they consume certain food groups (daily, several times a week, once a week, less than once a week, never), with higher scores reflecting less frequent consumption.
Data on consumption frequency of certain food groups before and after the health education program were collected to assess changes in eating habits 2-6 months over time.
Intervention: The intervention consisted of three parts: a) information, b) activation, c) questions and answers.
a. Information about a heart healthy diet was presented and patients had the possibility to ask questions on the content of an appropriate diet.
b. Activation: subsequent the patients were encouraged to develop their own personal action and coping plans concerning hearthealthy nutrition. Action plans are simple “When”-“Where”- and “How”-plans to concretise the prospective healthy behaviour. A connection between situation (when, where) and behaviour (how) is built. Once the specified environmental cue of the action plan occurs, the planned behaviour can be acted out without high effort [14]. An example for such an action plan may be: “I will eat fish twice a week, Tuesday and Friday evening.” Action planning helps to act in the intended way [34] and to initiate goal behaviour faster [10]. Coping planning serves as support to overcome potential obstacles and barriers that may frustrate planned behaviour and link them with suitable coping strategies. For example: “I’m short of time to buy some fish, so I’m eating tinned fish.” Due to a coping plan acting out planned behaviour in spite of personal difficulties should be facilitated.
c. Q&A: Patients presented their plans, they were discussed and the session was finished with general questions and answers.
Statistical methods
Frequencies and means (± SD) were used to describe the clinical and sociodemographic variables. Analysis of covariance was used to examine differences over time adjusted for baseline and for significant baseline differences [35]. Assumptions for homogeneity and sphericity were controlled for. In addition all data were screened for univariate and multivariate outliers and checked for normal distribution.
Sociodemographic and clinical baseline characteristics
The mean age of the 143 participants in the intervention group (IG) (control group CG: n=58) was 62 ± 11.3 years (CG: 64 ± 10.3 years), 64.3% were men (CG:77.6%). No baseline differences for self reported risk factors as smoking, diabetes, hypertension and depression were found. Patients in the IG were treated more frequently for hypercholesterolemia (p= .045). No baseline differences in intentions for the uptake of a heart healthy diet, in general self efficacy, in diet satisfaction and in perceived impact of diet on health were found between the intervention and the control group (Table 1). Both IG (1.3 ± 1.6) and CG (1.02 ± 1.6) are rather satisfied with their diet and both IG (1.01 ± 1.71) and CG (.57 ± 1.8) realise a slightly positive impact of diet on their health (Table 1).
| CG (n=58) M ± SD; N (%) |
IG (n=143) M ± SD; N (%) |
p-value chi2/t |
||
| Age | 62.28 ± 11.3 | 63.96 ± 10.3 | .308 (t) | |
| Male | 45 (77.6%) | 92 (64.3%) | .068 (chi2) | |
| BMI | 27.12 ± 3 | 26.46 ± 3.7 | .263(t) | |
| Self reported risk factors | smoking | 9 (15.5%) | 19 (13.3%) | .735 (chi2) |
| depression | 2 (3.4%) | 14 (9.8%) | .128 (chi2) | |
| hypercholesterolemia | 23 (39.7%) | 78 (54.5%) | .045 (chi2) | |
| diabetes | 13 (22.4%) | 22 (15.4%) | .265 (chi2) | |
| hypertension | 35 (60.3%) | 75 (52.4%) | .265 (chi2) | |
| Self reported health (1=excellent; 5=bad) | 3.23 ± .8 | 3.13 ± .8 | .410 (t) | |
| Self reported health | excellent very good good fair poor |
2 (3.5%) 4 (7%) 31 (54.4%) 19 (33.3%) 1 (1.8%) |
4 (2.9%) 18 (12.9%) 75 (54%) 40 (28.8%) 2 (1.4%) |
.804 (chi2) |
| Educational background | < 10 years of education 10-15 years of education >15 years of education |
45 (77.5%) 6 (10.3%) 1 (1.7%) |
98 (68.5%) 16 (11.2%) 10 (0.7%) |
.284 (chi2) |
| Occupation | employed retired job seeking other |
17 (29.3 %) 38 (65.5%) 1 (1.7%) 1 (1.7%) |
34 (23.8%) 93 (65 %) 2 (1.4%) 9 (6.3%) |
.526 (chi2) |
| General self efficacy (10=low; 40=high) | 33.08 ± 4.7 | 32.74 ± 5.3 | .700 (t) | |
| Intentions (1=low; 4 high) | 3.15 ± .5 | 3.08 ± .6 | .435 (t) | |
| Diet satisfaction (-3=low; +3=high) | 1.02 ± 1.6 | 1.30 ± 1.6 | .333 (t) | |
| Impact of diet on health (-3=low; +3=high) | .57 ± 1.8 | 1.01 ± 1.71 | .162 (t) | |
Table 1: Patients characteristic at baseline (t0).
Between group baseline differences in dietary variables
Significant baseline differences between CG and IG regarding alcoholic drink and coffee consumption (p=.000) and consumption of food without dietary fibre (p=.011) were found. CG and IG did not differ in consumption of low fat food, rich food, fish, eggs, vegetable fat, soft drinks and fruit juice, water and food with dietary fibre. (Table 2)
| mean ± SD | ||||
| CG | IG | p-value | ||
| Low fat food | 2.83 ± .6 | 2.98 ± .7 | .477 | |
| Rich food | 3.17 ± .9 | 3.10 ± .7 | .464 | |
| Fish | 3.76 ± .6 | 3.69 ± .7 | .744 | |
| Eggs | 3.15 ± .9 | 3.60 ± .9 | .801 | |
| Vegetable fat | 2.24 ± 1.2 | 2.19 ± 1.0 | .681 | |
| Alcoholic drinks and coffee | 3.44 ± .7 | 3.11 ± .9 | .000 | |
| Soft drinks and fruit juice | 3.41 ± 1.1 | 3.54 ± 1.1 | .691 | |
| Water | 1.32 ± .8 | 1.33 ± .8 | .833 | |
| Food with dietary fibre | 1.96 ± .7 | 1.91 ± .7 | .221 | |
| Food without dietary fibre | 2.48 ± .5 | 2.27 ± .6 | .011 | |
Table 2: Between group baseline differences in dietary variables.
Between group differences at month 2 on intention, planning items and action control
At month 2 there were no significant differences between IG and CG regarding intention, planning items and action control (Table 3).
| mean ± SD | |||
| CG | IG | p-value | |
| Intention | 3.22 ± .5 | 3.25 ± .5 | .710 |
| Action planning | 2.87 ± .9 | 3.07 ± .6 | .190 |
| Coping planning | 2.73 ± .8 | 2.87 ± .7 | .326 |
| Action control | 2.90 ± .7 | 3.02 ± .6 | .321 |
Table 3: Between group differences at month 2 (t1) on intention, planning items and action control.
Changes from baseline to month 2
Mean changes of diet variables: Patients of the IG increased their consumption of low fat food, fish, water and food with dietary fibre and reduced their consumption of rich food, eggs, alcoholic drinks/coffee, soft drinks/fruit juice and food without dietary fibre; however no significant difference to the CG was found. The IG reported an increase in consumption of vegetable fat, which was significantly different from the CG (p=.022) (Table 4 and Figure 3).
| ∆ t0t1 | ∆ t0t2 | |||||
| mean ± SD | mean ± SD | |||||
| CG | IG | p-value | CG | IG | p-value | |
| Low fat food | .00 ± .66 | .15 ± .66 | .544 | -.26 ± .86 | .13 ± .64 | .001 |
| Rich food | -.49 ± .87 | -.32 ± .74 | .170 | -.50 ± .94 | -.34 ± .67 | .068 |
| Fish | .00 ± .59 | .01 ± .65 | .735 | -.09 ± .66 | .16 ± .66 | .007 |
| Eggs | -.03 ± .10 | -.16 ± .81 | .578 | -.25 ± 1.00 | -.08 ± .81 | .155 |
| Vegetable fat | -.12 ± .1.23 | .30 ± .1.08 | .022 | -.10 ± 1.12 | .20 ± 1.0 | .148 |
| Alcoholic drinks/ coffe | .21 ± 1.20 | -.28 ± .82 | .218 | -.04 ± .62 | -.17 ± .97 | .386 |
| Soft drinks/ fruit juice | .00 ± 1.05 | -.19 ± .84 | .686 | -.15 ± .88 | -.26 ± .89 | .646 |
| Water | -.18 ± .10 | .05 ± .82 | .190 | .05 ± .56 | -.14 ± .69 | .026 |
| Food with dietary fibre | -.02 ± .63 | .04 ± .52 | .544 | .12 ± .68 | .11 ± .49 | .929 |
| Food without dietary fibre | -.10 ± .65 | -.15 ± .65 | .411 | -.05 ± .60 | -.26 ± .69 | .435 |
Table 4: Mean changes in consumption of diet variables over time (between group differences controlled for baseline and baseline differences).
Mean changes in intention, diet satisfaction and impact of diet on health: No difference in mean changes from baseline to month 2 between CG and IG in intention, diet satisfaction and impact of diet on health were found. All variables increased in both groups (Table 5).
| ∆ t0t1 | |||
| mean ± SD | |||
| CG | IG | p-value | |
| intentions | -.04 ± .43 | -.14 ± .54 | .931 |
| diet satisfaction | -.28 ± 1.53 | -.21 ± 1.43 | .859 |
| impact of diet | -.30 ± 2.12 | -.63 ± 1.67 | .243 |
Table 5: Mean changes in intention, diet satisfaction and impact of diet on health (between group differences controlled for baseline and baseline differences).
Changes from baseline to month 6
Mean changes of diet variables: Patients of the IG increased their consumption of vegetable fat and food with dietary fibre, and reduced their consumption of rich food, eggs, alcoholic drinks/coffee, soft drinks/fruit juice and food without dietary fibre; however no significant difference to the CG was found. A significant mean difference was found in low fat food consumption (p=.001) and in fish consumption (p=.007). For both variables the IG reported an increase. However the water consumption significantly decreased in IG over time compared to the CG (p=.026) (Table 4 and Figure 3).
The study found that the application of the HAPA model in nutrition in an acute hospital setting showed limited effects on relevant diet behaviour in the short term.
To our knowledge the present study examined for the first time the impact of a HAPA model based intervention on dietary behaviour under use of a differential FFQ. So far studies have primarily focused on the change of intentions, action and coping planning. This enables to make a statement on real nutrition behaviour and not only to collect and report data on psychological constructs (e.g. intentions, planning behaviour, etc.) or global dietary behaviour variables (e.g. “I avoid cholesterol-rich food” [19], “I deliberately eat vitamin-rich food [19], “I deliberately eat vitamin-rich food” [20] or “Within the last two weeks how often have you eaten a portion of fruit and vegetables?” [21] ).
Patients participating in the education program based on the HAPA model showed after 2 months one desired short term change on their nutrition habits in contrast to the control group. They increased their consumption of vegetable fat. The increase of vegetable fat consumption continues to exist after 6 months, but with no significance in comparison to the CG. Over the six month period patients of the IG succeeded to increase their low fat food and fish consumption while the CG reduced both. One explanation for these results may be that a life style change including dietary change after an inpatient hospital stay takes some time. Patients returning back home are busy with their physical recovery and try to find back to their normal course of life. A dietary change requires a serious engagement with this issue.
At baseline both subgroups presented high intention scores for a heart healthy diet (CG: M=3.15; IG: M=3.08). However both groups showed actual little nutrition change over time. Due to the social components of eating, nutrition change is a more complicated process than for example increasing sports in daily routine. Breakfast, lunch and dinner involve more than only the patient (i.e. partner, family, etc.). Especially in elderly male patients the partner is often responsible for choosing food and cooking meals. This circumstance not only complicates implementing the in the health education program developed personal action and coping plans, but also asserts a claim for including family and first of all the partner in consultation and planning of dietary change. An additional intervention two months after baseline could make sense, on the one hand to control the implementation of the developed plans, on the other hand to sustain the maintenance of the implemented plans according to the HAPA model (Figure 1). In general follow-up meetings could be useful to readjust the developed plans to patient’s daily life. Such follow-up meetings could be part of a cardiac rehabilitation program.
A consequence of the results was to reconsider the nutrition topics of the educational group setting. Retrospectively it seems to be unrealistic to attain changes in all different nutrition category groups. A focus on selective topics (e.g. low fat food, fish or vegetable fat consumption) may have more effects and simplifies also the planning intervention for the patients.
Participants of the IG doubled their intentions and quadrupled their believe of impact of diet on their health, however there is no significant difference between IG and CG regarding intention, planning items and action control at month 2. For this very brief group intervention the first follow-up period of 2 months (t1) seems to be too long. Comparable studies [15] comprehend a person to person planning interview and a 6 week postal plan reminding intervention. However both IG and CG were able to enhance their intentions over a 2 month time period. Future studies should also include an ongoing monitoring of relevant variables (i.e. diet satisfaction, impact of diet on health, intention).
One limitation of this study is that there is no standardized FFQ available for cardiac patients. We therefore had to construct an appropriate questionnaire for this study. For an easier completion and more comprehension we decided to divide food into high and low fat food. The more scientific classification would be to differentiate between food with saturated and unsaturated fatty acids. However this could be more difficult to understand for patients.
Another potential problem in FFQ data collection is the probability for socially desirable answers. Socially desirable answers may become more frequently if knowledge on healthy diet is increasing.
A further limitation to the outcome of the present study can be seen in the small sample size in the two subgroups. Detection of moderate effects, even if the effect actually exists, could not be statistically demonstrated due to lack of power. For a further study a power analysis should be considered in the sample size calculation and a correspondingly larger sample size should be planned.
Finally a limitation for this study may be the missing randomisation in the assigning process of the participants to IG or CG. We collected CG data two months prior the start of the health education program on the cardiology ward. The inclusion criteria were the same for both groups.
In conclusion the present study demonstrates that a very short singular health psychological intervention, well applicable in inpatients routine, leads to some desired changes in patients’ nutrition behaviour in the short term. However to enlarge and stabilise changes in heart healthy nutrition a follow-up intervention, e.g. in the course of a cardiac rehabilitation program following acute care could be beneficial.
The present study was funded by the Quality Promotion Program of the Tyrolean Health Fund [#10-02/78].