International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2020)Volume 8, Issue 7
Aim of the work: Measure incidence of shoulder impingement syndrome (SIS) among carpal tunnel syndrome (CTS) patients and relationship with other risk factors.
Patients and Methods: This is a cross sectional study at outpatient setting, included 565 patients (210male and 355female) with clinical manifestation of CTS associated with shoulder pain.
Exclusion criteria: patients with manifestation suggestive of peripheral neuropathy, cervical radiculopathy or other neuromuscular disorder. Each patient was subjected to the following; detailed history, Pain score by visual analogue score, (VAS), neurological examination including Tinel’s sign and Phalen test, shoulder exam including Neer Impingement sign and Hawkins impingement sign, neck exam, Hemoglobin A1c level, nerve conduction study (NCS) for median, ulnar, Including the comparative techniques, electromyography of both upper extremities, MRI of shoulders if possible.
Results: Mean age was 48.2 y, majority was hard worker (56.8%), light worker (22.8%), house wives (16.8%) and house- keeping (3.5%). Only 161 patients (28.5%) had diabetes mellitus type II. Pain score was severe in 58.2%, moderate in 32.6% and mild in 3.7%, no pain in 5.5%. All studied patients (100%) had CTS confirmed by NCS. SIS was found on 380patients (67.25%). shoulder MRI was done for only 298 patients and all showed rotator cuff tendopathy. Significant incidence of SIS among diabetics (p 0.001). Significant incidence of MRI findings among diabetics (p 0.0001). Among diabetics 78.26% have both CTS and clinical impingement together, that is significantly higher than non-diabetics (p=0.0004). SIS had significantly high incidence among hard worker (p=0012). SIS was significantly correlated with prolonged distal median motor latency (right side p=0.011, left side p=0.023) and with prolonged peak median sensory latency (p=0.38 on right side and p=0.033 on left side). Pain score was significantly correlated with SIS (p=0.27) and MRI findings (p=0.031).
Conclusions: Significant high incidence of SIS among CTS patients This is higher among diabetic patients and manual worker. SIS significantly increases VAS among CTS patients and is significantly correlated with degree of CTS as reflected by median distal motor and peak sensory latency.
Shoulder impingement; Carpal tunnel syndrome; Tingling; Burning; Pain
Carpal Tunnel Syndrome (CTS) is one of the most common upper limb entrapment neuropathies. It constitutes approximately 90% of all entrapment neuropathies [1,2]. It is the result of squeezing or compression of median nerve at the carpal tunnel. An estimated one million adults from the united states annually have CTS requiring medical treatment with high cost burden on health care system [1-3]. Carpal Tunnel Syndrome presents clinically with variable symptoms depend on the severity of the disease. These symptoms include numbness, tingling, burning and pain in the hand predominantly, in the thumb, index, middle and lateral half of ring finger. The pain or tingling may travel up the forearm toward the shoulder. In addition to weakness, clumsiness of the hands. Among the presenting symptom of Carpal Tunnel Syndrome is shoulder pain [1,2].
Shoulder Impingement Syndrome (SIS) refers to a combination of shoulder symptoms, examination findings, and radiologic signs attributable to the compression of structures around the glenohumeral joint that occur with shoulder elevation. Such compression causes persistent pain and dysfunction. Shoulder pain is a common presenting complaint in primary care clinics, and SIS is likely the most common cause of shoulder pain [3-6].
The incidence and association of Carpal Tunnel Syndrome and SIS is not studied. The aim of this study was to measure the incidence of Shoulder Impingement Syndrome among Carpal Tunnel Syndrome (CTS) patients and relationship with other risk factors.
This was cross sectional study at outpatient setting that included 565 patients with clinical manifestation of Carpal Tunnel Syndrome associated with shoulder pain. All Included patients had signed informed consent prior to their participation.
Exclusion criteria
Patients with manifestation suggestive of peripheral neuropathy, cervical radiculopathy or other neuromuscular disorder. Also, patients with history of trauma to shoulder.
All Included patients were subjected to the following: Medical history, occupational history, social history, Pain score by VAS, neurological examination including Tinel’s sign [7] and Phalen test [8], detailed shoulder exam including Neer Impingement sign and Hawkins impingement sign [9], neck exam including Spurling test [10], Hemoglobin A1c level, Nerve Conduction Study (NCS) for median, ulnar, median-ulnar, median-radial comparative studies, F wave, electromyography of both upper extremities [11], shoulders MRI if possible.
Statistical analysis
The Data was collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 20) software.
Athematic mean, standard deviation, for categorized parameters, chai square test was used while for numerical data t-test was used to compare two groups while for more than two groups ANOVA test was used. To find the association between two variables. The level of significant was 0.05.
The study was conducted on 565 patients; 210 male (37.16%) and 355 female (62.83%). Mean age was 55.94 ± 12.97 (23-85 y). Table 1 showing the distribution of the clinical data among the studied patients. Pain score was severe in 58.2%. The majority were hard worker (321 patients 56.8%) followed by light worker 129 patients (22.8%) then house wives 95 patients (16.8%) and house-keeping 20 patients (3.5%). All studied patients (100%) had CTS confirmed by NCS. 76.8% had pure median sensory neuropathy and 23.2% had sensorimotor neuropathy. 97.3% had pure demyelinating neuropathy and 2.7% had demyelinating-axonal neuropathy (Figure 1).
| Number “n=565” | Percent | |
|---|---|---|
| Pain scale | ||
| No | 31 | 5.5 |
| Mild | 21 | 3.7 |
| Moderate | 184 | 32.6 |
| Severe | 329 | 58.2 |
| Range | 0-10 | |
| Mean ± S.D. | 6.83 ± 2.6 | |
| Present of numbness | 401 | 71 |
| Sensory exam | ||
| Intact | 346 | 61.2 |
| Impaired | 219 | 38.8 |
| Motor exam | ||
| Intact | 460 | 82.4 |
| Impaired | 105 | 18.6 |
| Tinnel's sign | 163 | 28.8 |
| No | 53 | 9.4 |
| Right side | 116 | 20.5 |
| Left side | 233 | 41.2 |
| Both side | ||
| Phalen's test | 301 | 53.3 |
| No | 44 | 7.8 |
| Right side | 73 | 12.9 |
| Left side | 147 | 26 |
| Both side | ||
| Muscle wasting | ||
| No | 515 | 91.2 |
| Right side | 10 | 1.8 |
| Left side | 32 | 5.7 |
| Both side | 8 | 1.4 |
Table 1: Distribution of the studied group regarding demographic and clinical data.
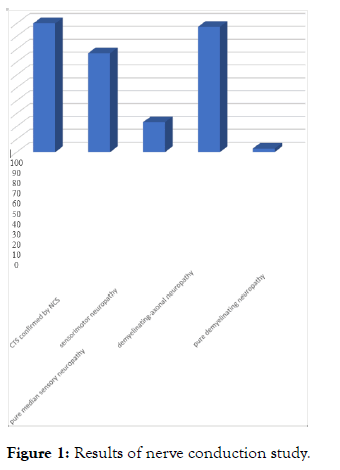
Figure 1: Results of nerve conduction study.
Table 2 demonstrates the distribution of Clinical Shoulder Impingement Syndrome, Diabetes Mellitus and MRI findings among the studied patients Only 161 patients (28.5%) had diabetes mellitus type II.SIS was found on 380 patients (67.25%). MRI was done for 298 patients (52.74%) all showed positive results of rotator cuff tendinopathy.
| Number “n=565” | Percent | |
|---|---|---|
| D.M. | ||
| Negative | 404 | 71.5 |
| Positive | 161 | 28.5 |
| Clinical impingement | ||
| No | 185 | 32.7 |
| Right side | 150 | 26.5 |
| Left side | 110 | 19.5 |
| Both side | 120 | 21.2 |
| MRI findings | ||
| No | 267 | 47.3 |
| Right side | 107 | 18.9 |
| Left side | 97 | 17.2 |
| Both side | 94 | 16.6 |
Table 2: Distribution of the studied group regarding incidence of DM, clinical impingement and MRI findings.
Table 3 presented the relationship between SIS, DM, and MRI findings. There is significant high incidence of clinical impingement among diabetics compared to non-diabetics (p=0.001).
| DM | X2P | ||||
|---|---|---|---|---|---|
| Negative | Positive | ||||
| No. | % | No. | % | ||
| Clinical impingent | 30.131 0.0001 |
||||
| No | 150 | 81.1 | 35 | 18.9 | |
| Right side | 117 | 78.0 | 33 | 22.0 | |
| Left side | 60 | 54.5 | 50 | 45.5 | |
| Both side | 77 | 64.2 | 43 | 35.8 | |
| MRI findings | 21.036 0.0001 |
||||
| No | 205 | 76.8 | 62 | 23.2 | |
| Right side | 85 | 79.4 | 22 | 20.6 | |
| Left side | 61 | 62.9 | 36 | 37.1 | |
| Both side | 53 | 56.4 | 41 | 43.6 | |
Table 3: Distribution of the studied group regarding incidence of DM, clinical impingement and MRI findings.
Significant incidence of MRI findings among diabetic compared to non-diabetic (p=0.0001).
Among diabetics 78.26% have both CTS and clinical impingement together, that is significantly higher than nondiabetics (p=0.0004). Clinical impingement had significantly high incidence among hard worker (p=0012) distributed as 75.3% on right side 62.7% on the left side and 43.3% on both shoulders. This is followed by house wives were 14.7% affecting right side, 25.5% on left side and 33.3% on both sides. Light worker was affected by both sides in 15%, right side in 8% and left side in 6.4%.
Table 4 demonstrates the relationship between SIS and distal motor median latency and peak sensory median latency. SIS was significantly correlated with prolonged distal median motor latency and prolonged peak median sensory latency.
| Clinical impingent | Motor distal latency | Peak median sensory | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| No Range Mean ± S.D. |
2.30-8.80 3.70 ± 0.85 |
2.40-5.50 3.17 ± 0.74 |
2.80-5.90 3.90 ± 0.63 |
2.80-6.00 3.76 ± 0.65 |
| Right side Range Mean ± S.D. |
0.00-12.70 4.15 ± 2.10 |
0.00-9.80 3.23 ± 1.59 |
1.40-5.40 3.91 ± 0.81 |
0.00-6.80 3.92 ± 1.37 |
| Left side Range Mean ± S.D. |
2.70-5.60 3.84 ± 0.77 |
0.00-9.80 3.44 ± 1.63 |
2.80-6.30 4.00 ± 0.90 |
1.30-6.50 3.92 ± 0.80 |
| Both side Range Mean ± S.D. |
0.00-9.10 3.64 ± 1.57 |
2.30-7.70 3.87 ± 0.99 |
0.00-7.10 4.07 ± 1.43 |
2.90-6.80 4.07 ± 1.03 |
| F | 3.761 | 3.139 | 2.426 | 2.451 |
| P | 0.011 | 0.0230 | 0.038 | 0.033 |
Table 4: Relation between clinical impingent and both motor distal latency and peak median sensory
Table 5 presents the relation between MRI findings and distal median motor latency and peak median sensory latency.
| MRI findings | Motor distal latency | Peak median sensory | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| No Range Mean ± S.D. |
0.00-9.10 3.55 ± 1.31 |
0.00-9.80 3.42 ± 1.26 |
0.00-7.10 3.78 ± 0.98 |
0.00-6.80 3.67 ± 1.00 |
| Right side Range Mean ± S.D. |
2.70-12.70 4.45 ± 1.90 |
2.50-6.90 3.96 ± 1.05 |
3.10-7.10 4.43 ± 0.99 |
2.80-6.30 4.19 ± 0.88 |
| Left side Range Mean ± S.D. |
2.70-5.60 3.83 ± 0.84 |
2.30-7.70 3.90 ± 1.05 |
1.40-6.30 3.91 ± 0.94 |
1.30-6.50 3.95 ± 0.89 |
| Both side Range Mean ± S.D. |
2.30-9.10 3.93 ± 1.46 |
2.30-9.80 4.05 ± 1.53 |
2.80-6.30 4.06 ± 0.88 |
3.00-6.80 4.19 ± 1.07 |
| F | 10.559 | 9.493 | 11.787 | 11.213 |
| P | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
Table 5: Relation between MRI findings and both motor distal latency and peak median sensory.
Table 6 shows the relation between VAS, SIS and MRI findings. Pain score was significantly correlated with clinical impingement (p=0.27) as well as MRI findings (p=0.031).
| Pain score | FP | ||||
|---|---|---|---|---|---|
| No | Right side | Left side | Both side | ||
| Clinical impingent Range Mean ± S.D. |
0.00-4.00 3.03 ± 0.738 |
0.00-10.00 7.30 ± 2.25 |
0.00-10.00 6.60 ± 2.58 |
3.00-10.00 7.24 ± 2.00 |
6.742 0.027 |
| MRI findings Range Mean ± S.D. |
0.00-4.00 3.21 ± 1.27 |
0.00-10.00 7.15 ± 2.22 |
0.00-10.00 6.53 ± 2.58 |
3.00-10.00 7.32 ± 2.08 |
5.98 0.031 |
Table 6: Relation between clinical impingent and MRI findings and pain score.
This study was conducted on patients with the clinical manifestations suggestive of CTS associated with shoulder pain. All the studied patients confirmed to have CTS by electrophysiological testing. Sixty seven percent of those patients proven to have SIS clinically. Confirmatory shoulder MRI was done for 52.74% of those patients and all showed rotator cuff tendinopathy.
In this study, also we have studied other associated risk factors that could influence the occurrence of SIS among CTS patients, mainly DM and occupation.
We have found that diabetes mellitus significantly increases the association of CTS and SIS.
As regards occupation, heavy manual worker increased the incidence of SIS and CTS among the studied patients.
There is no similar study in the literature, but Dalboge et al. [12] reported increased risk of surgery for SIS in relation to occupational cumulative mechanical exposure, DM and body mass index [12].
There are multiple studies in the previous literature documenting the rheumatological complication of DM including CTS and SIS [13-20].
Other studies documented the association between SIS and manual labor work [21-23].
Rosenbaum et al. reported high prevalence of SIS, epicondylitis and low back pain among latino poltry workers and manual workers [24].
Other studies documented the high incidence of work-related Carpal Tunnel Syndrome [25,26].
Previous researchers have studied the underlying mechanism by which diabetes results in its musculoskeletal complications. However, the mechanism is not fully established. A major hypothesis is that accumulation of Advanced Glycation End products (AGE)s and their crosslinking of collagen may contribute to the development of such complication including tendon degeneration in the rotator cuff and diabetes related hand disorders.
The accumulation of AGEs could also potentially affect tendon strength and repair and play a role in microvascular complications and inflammation [27,28].
This study documented significant relationship between the SIS as well as MRI findings and the severity of Carpal Tunnel Syndrome as demonstrated with electrophysiological findings of prolonged distal motor latency and prolonged peak sensory latency. This indicates that the severity of carpal tunnel is positively related with the presence of Shoulder Impingement Syndrome as well as its MRI findings. As there are no similar studies in the literature so no documentation about this evidence before. But Yurdakul et al. have studied the effect of diabetes and another metabolic syndrome. She concluded that the severity of carpal tunnel as evidenced by electrophysiological testing tends to be more severe with combination of diabetes mellitus and other metabolic syndromes [29].
For those who were diabetics in the study and showed significant association between CTS and SIS as well as MRI findings we can explain the significant relationship between the severity of electrophysiological findings of CTS and SIS in light of the previously suggested theory of the accumulated advanced glycation end products.
However, for the non-diabetic patients that showed also positive association between CTS and SIS as well as the severity of CTS as reflected by the electrophysiological findings, could be the work-related factor play a role for such association. Could be also a pre-diabetic status that was not detected and tested since complication of diabetes sometimes happened before the evidence of diabetes itself. This point needs further study.
We have found that the pain score by VAS was significantly correlated with SIS as well as the positive MRI findings. This could be explained by the presence of additional pathology i.e SIS to the existing CTS significantly increase the pain level.
There is significant high incidence of Shoulder Impingement Syndrome among patients with Carpal Tunnel Syndrome. The incidence is higher among diabetic patients and those who have occupations require hard manual working. The presences of impingement syndrome significantly increases the pain score among Carpal Tunnel Syndrome patients and is significantly correlated with degree of carpal tunnel as reflected by median distal motor and peak sensory latency.
None
Citation: Hussein N, Desmarets T, Vilchez R (2020) Incidence of Shoulder Impingement Syndrome Among Patients with Carpal Tunnel Syndrome: Epidemiological Study. Int J Phys Med Rehabil. 8:575.
Received: 19-Oct-2020 Accepted: 02-Nov-2020 Published: 09-Nov-2020 , DOI: 10.35248/2329-9096.20.8.575
Copyright: © 2020 Hussein N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.