
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Review Article - (2023)Volume 14, Issue 6
Background: Rebound pain is severe pain experienced after the resolution of regional anesthesia. Both patients, surgical and anesthesia related factors affect incidence as well as the severity of rebound pain. Use of perioperative multimodal decreases incidence as well as the severity of rebound pain after resolution of peripheral nerve block. Therefore, this systematic review aimed to review about incidence, risk, prevention, and management of rebound pain after resolution of peripheral nerve block.
Methods: A medical search engines of PubMed, Google Scholar, Cochrane Review, and PubMed Centeral to get access for current and updated evidences on procedures on risk stratification, prevention and management of corneal abrasion for non-ocular surgery and we formulate the key questions, scope, and eligibility criteria for the articles to be included, advanced search strategy of electronic sources from databases and websites was conducted. Screening of literatures was conducted with proper appraisal checklist. This review was reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement.
Results: A total of 8767 articles were identified from databases and websites using an electronic search. Two hundred articles were removed for duplication and 7720 studies were excluded after reviewing titles and abstracts. At the screening stage, 1205 articles were retrieved and evaluated for eligibility. Finally, 50 studies met the eligibility criteria and were included in this systematic review.
Conclusions and recommendation: The overall incidence of rebound pain after PNB resolved may reach 61.7%. Both patients, surgical and anesthesia related factors affect incidence as well as the severity of rebound pain. Use of perioperative multimodal strategy decreases incidence as well as the severity of rebound pain after resolution of peripheral nerve block.
Rebound pain; Regional anesthesia; Peripheral nerve block; Risk management; Prevention
EC: Ethiopian Calendar; GC: Gregorian Calendar; ISB: Inter Scalene Block; MI: Myocardial Ischemia; NRS: Numerical Rating Scale; PCA: Patient Controlled Analgesia; PNB: Peripheral Nerve Block; RP: Rebound Pain; RPS: Rebound Pain Score
Statement of the problem
Regional anesthesia, specifically Peripheral Nerve Blocks (PNBs) is routinely performed for perioperative analgesia/anesthesia in patients undergoing surgery [1]. It allows a great role in maximizing post-operative pain control while minimizing opioid consumption and a fast hospital discharge [2,3].
The intrinsic pro-inflammatory properties of local anesthetics, when associated with PNB nerve damage, may cause post-PNB hyperalgesia and neuropathic pain, and these manifestations may present as rebound pain [4].
Rebound Pain (RP) is mechanical surgical pain caused by unopposed nociceptive inputs that are brutally uncovered after PNB resolution and characterized by sudden, significant pain following regional nerve blockade regression [5]. It is a quantifiable difference in pain scores when the block is working versus the increase in acute pain encountered during the first few hours after the effects of perineurally single injection or continuous infusion local anesthetics resolve [6]. It may reduce or even negate the overall benefits of a peripheral nerve block. Rebound pain is defined as transient acute postoperative pain within 12 hrs-24 hrs that ensues following resolution of sensory blocked [7-12]. Rebound pain score the lowest pain score during the first 12 h before the PNB wears off is subtracted from the highest pain score during the first 12 h after the PNB wears off [13].
The incidence of rebound pain after Peripheral Nerve Block (PNB) resolves could reach around 40% of patients may be due to abnormal spontaneous C-fiber hyperactivity and nociceptor hyper-excitability without mechanical nerve lesion.
Damage to the peripheral nociceptor provokes a continuous firing of pain signals leading to either an exaggerated response to normally painful stimuli or a noxious response to normally non-painful stimulation.
Poorly managed postoperative pain can result in adverse consequences including impaired quality of recovery, opioid dependence, PPSP, and increased medical costs. Therefore it is important to examine if rebound pain may have a significant impact on other health related outcomes.
Postoperative pain is one of the most feared surgical complications reported by patients, which is frequently followed by a painful recovery and appropriate treatment of acute postoperative pain is associated with better clinical outcomes, while inadequate pain control may negatively impact patients' postoperative experience.
Some strategies used to prevent and manage rebound pain like continuous PNB catheter techniques, using local anesthetic adjuvant, multimodal analgesics and preoperative education and counseling regarding rebound pain were effective to prevent and managing rebound pain.
Due to the shortage of experimental and clinical studies, the incidence of rebound pain phenomenon is still poorly documented. Nevertheless, its occurrence has been increasingly reported by researchers it could profoundly impact the patient's recovery experience.
The occurrence of rebound pain may outweigh the benefits of PNBs and represent a clinically relevant problem.
Rebound pain is a common, yet under-recognized acute increase in pain severity after a Peripheral Nerve Block (PNB) has receded, typically manifesting within 24 h after the block was performed. Rebound pain is still a poorly understood concept and few studies have evaluated its full impact on the use of regional anesthesia as a strategy to reduce long term pain and opioid consumption. Despite economic pressure and the wellknown early benefits of PNBs, rebound pain unanswered questions are one more challenge in the area of perioperative management. Therefore, this systematic review aimed to review incidence, risk, and prevention and management of rebound pain after peripheral nerve block is resolved.
Search strategy
The literatures are searched from medical search engines of PubMed, Google Scholar, Cochrane Review, and PubMed Central to get access for current and updated evidences on procedures on Incidence, risk, prevention and management of Rebound pain after resolution of peripheral nerve block.
Different evidences are searched by using the key term (rebound pain AND Incidence) OR prevalence)) AND risk factor) and Rebound pain prevention AND management. Eligible criteria English language, human study focuses on the study topic, study in the last 20 years was implemented to identify or filter high level evidences. In this review, articles that fulfilled mention eligible criteria were included. Articles contain corneal abrasion due to ocular surgery are excluded. All of the research articles, which were identified from searches of electronic databases, were imported in to Endnote software and duplicates were removed. Then collected by filtering based on level of significance to this guideline with proper appraisal and evaluation of study quality with different level of evidence. This work has been reported in line with AMSTAR (Assessing the Methodological quality of Systematic Reviews) guidelines [14].
This review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 criteria (Figure 1) [15]. This review was registered in research registry with unique identifying number of review registry 1574.
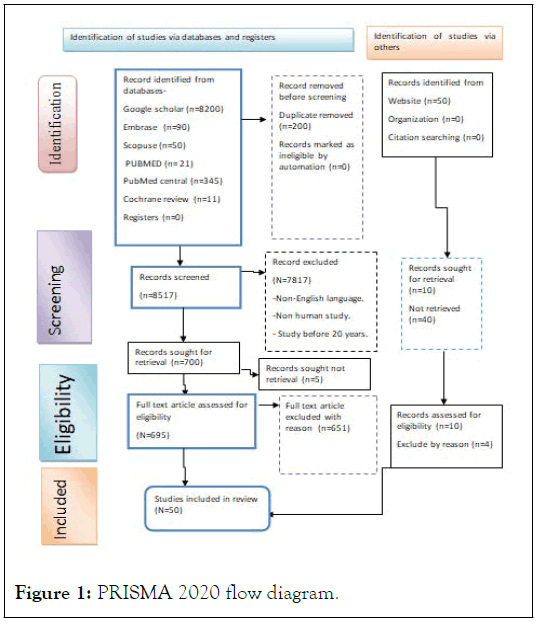
Figure 1: PRISMA 2020 flow diagram.
Eligibility criteria
All studies related to rebound pain in English language, with full text available for search and conducted across the globe were included in this systematic review. Those studies that reported duplicated sources, unrelated articles, case reports, and articles without full text available with attempts to contact the corresponding author via email were excluded in this systematic review.
Study selection
Selected articles for the review, which were exported in to endnote reference manager software to remove duplicates, and screened the titles and abstracts.
Study quality assessment
The article appraised using AMSTAR 2 methodological quality appraisal checklist. Any disagreement was discussed and resolved by the author. The critical analysis checklist has 16 parameters. The quality of this review after critical appraisal of its method was reported as high.
Study selection
A total of 8767 articles were identified from databases and websites using an electronic search. Two hundred articles were removed for duplication and 7817 studies were excluded after reviewing titles and abstracts. At the screening stage, 710 articles were retrieved and evaluated for eligibility. Finally, 50 studies met the eligibility criteria and were included in this systematic review.
Description of included studies
Out of 1445 articles retrieved, 50 studies met the eligibility criteria and were included in this systematic review. Out of all articles included, 13 were systematic reviews, 1 meta-analysis, 1 were cross-sectional studies, 3 were guidelines, 6 were cohort studies, 1 cohort and 3 were controlled trials.
Incidence of rebound pain
Following a Peripheral Nerve Block (PNB), rebound pain is a frequent but under-recognized acute increase in pain intensity that typically appears within 12 hours to 24 hours and negatively affects sleep quality [16]. The incidence of the rate of rebound pain could reach 40% of patients at PNB resolution. In Ethiopia, a cross-sectional study was done to determine the frequency of rebound pain following peripheral nerve block resolution. With a mean rebound pain score of 4.192.1 (95% CI: 3.94, 4.5), the overall incidence of rebound pain after peripheral nerve block was resolved was 61.7% (95% CI: 56.5-66.7) [17].
According to a Canadian retrospective cohort research, 49.6% of people experienced rebound pain after PNB was treated.
According to a prospective research conducted in Belgium, up to 40% of peripheral nerve block patients have rebound discomfort. In the past, between 35% and 41% of patients under regional anesthesia experienced severe rebound pain [18].
Risk factor for rebound pain
According to a cross-sectional study conducted in Ethiopia, using intravenous dexamethasone prior to surgery, having preoperative pain, having a specific type of surgery, using a postoperative NSAID, and using an opioid were all independent factors linked to rebound pain, technique of peripheral nerve block according to a New York comparative study, a single injection has a greater risk of rebound discomfort than a continuous peripheral nerve block [19]. This conclusion is reinforced by earlier research that found a strong correlation between rebound pain and intravenous dexamethasone use or a reduction in the risk of rebound pain after PNB disappeared. Surgical factors can produce an abnormal level of plasticity at the peripheral nociceptor level and in the central neurons involved in receiving and processing the direct and indirect inputs.
According to a cross-sectional study conducted in Ethiopia, using intravenous dexamethasone prior to surgery, having preoperative pain, having a specific type of surgery, using a postoperative NSAID, and using an opioid were all independent factors linked to rebound pain. Patients who had bone surgery had a substantial correlation with rebound pain, according to a prior cohort research.
This may be corroborated by studies across a range of noncardiac surgeries that found that preoperative pain level was a strong predictor of severe postoperative pain [20]. Preoperative pain may predisposition to rebound pain. This is also confirmed by patients' reports of rebound pain after complete hip or total knee arthroplasty using PNB, who were more likely to have preexisting joint pain. The gender of the patients in this prospective cohort study conducted in Canada and Netherlands showed no association with the prevalence of rebound pain, young age, female gender, and orthopedic (particularly upper limb) surgeries.
Rebound pain is 6.5 times more likely to occur in patients after bone surgery than those having soft tissue surgery. Additionally identified as independent risk factors for rebound pain are the patient's cognitive functioning and expectation of postoperative pain.
General Anesthesia (GA) was administered to patients having arthroscopic rotator cuff replacement surgery in three groups: GA alone, GA paired with a single inter scalene block, and GA combined with a peri-neural inter scalene catheter. The catheter group had much lower pain scores than the other two groups at all time intervals, and it experienced less rebound pain.
Comparatively to when surgery is performed under PNB alone, combining PNB with central neuraxial blockade aids in lessening the degree of rebound pain.
Age, surgery type, surgical site, fracture type, surgical regimen, PNB type, nerve injury, local anesthetic concentration, insufficient postoperative analgesia, inadequate patient education regarding pain management during the postoperative period, the presence of preoperative pain, and psychological factors are some factors that may be related to rebound pain. While rebound pain is very severe in some patients, especially younger patients, it is probably less of a problem in elderly patients.
Rebound pain may develop after surgery depending on the operative site and procedure type, and studies have indicated that some surgical procedures and techniques are more likely to do so. When compared to complex knee surgery, shoulder surgery caused more pain. PNBs are less safe in this situation because the use of PNBs for acute fracture surgery has not been adequately studied and because the evolution of postoperative pain in acute fractures differs from that in elective procedures. Rebound pain is particularly prevalent in patients under-going outpatient surgery, which is believed to occur as a result of greater difficulty in having adequate pain control outside the hospital setting and type of PNB used for anesthesia has not been objectively evaluated, but it is believed that neural damage caused by needle insertion and pressure trauma during local anesthetic injection may induce some perineurally inflammation. In vivo rebound pain intensity can be influenced by local anesthetic concentrations, but this component has not been clinically investigated.
Prevention and management of rebound pain
The occurrence of rebound pain may be reduced by taking an analgesic medication 1-2 hours before the PNB provided analgesia expires. Ineffective pain control during the transition phase for oral analgesics when the duration of analgesia supplied by PNB ceases may result from inadequate patient education regarding the necessity for a pain therapy, such as bridging analgesia, even in the absence of pain. Because patients with nerve damage may develop falsely low pain tolerance due to patients' expectations about PNB, this could affect how postoperative pain is perceived and treated.
Despite the fact that a recent systematic analysis found that all delivery methods are equal in terms of the length of block analgesia, 24 hours pain scores, and cumulative opioid intake at 24 hours postoperatively, dexamethasone has been proven to prolong PNB duration when administered perineurally as opposed to intravenously.
In a previous meta-analysis, dexamethasone at single dosages greater than 0.1 mg kg-1 was demonstrated to lessen postoperative discomfort. Instead of any potential impact on PNB duration, the reduction in rebound pain incidence and RPS reported may be consistent with the known effect of iv dexamethasone on postoperative pain generally.
Preoperative analgesia may be used as pre-emptive or preventive analgesia to reduce peripheral and central sensitization, which could help to explain this.
According to previous study, increasing the duration of analgesia while also reducing the overall dose needed for local anesthetics may help to lower the occurrence of rebound pain after PNB is treated. Patients who received postoperative analgesia, such as opioids and NSAIDs, in this study were less likely to develop a rebound after PNB was treated. This could be explained by employing perioperative multimodal analgesia, which has an opioid sparing effect and also reduces the intensity of postoperative pain, to reduce perioperative opioid consumption.
The incidence of rebound pain was significantly lower in the dexamethasone group compared to the control group (37.1% and 82.9%, respectively, P 0.001) in a prospective study by Woo, et al. The authors assessed whether perineurally administering dexamethasone as an adjuvant reduces the intensity and incidence of rebound pain in patients undergoing arthroscopic shoulder surgery.
The use of non-pharmacological methods, such as educating patients about post-PNB rebound pain and postoperative analgesia, and informing them about these topics.
Rebound pain control may benefit from the use of pharmaceuticals including gabapentin, acetaminophen, ibuprofen, and dextromethorphan. These medications may also assist sustain analgesia during the transitional phase as PNB fades. Avoiding the use of short acting opioids and volatile gases, as well as including the use of medications that modify pain response, like esmolol, is advised, dexamethasone, betamethasone, and alpha-2 agonists have been reported to prolong the effects of brachial plexus block when added to local anesthetics. When non-systemic perineurally combined with a clinical dose of bupivacaine, rebound hyperalgesia after blockade resolution and reversible bupivacaine induced neurotoxicity may be avoided. According to certain research, dexamethasone administered systemically may help PNB's effects last longer.
Use of combined peripheral nerve blocks reduce incidence of rebound pain. After arthroscopic rotator cuff repair, axillary and suprascapular nerve blocks guided by ultrasound reduced the phenomenon of rebound pain. The use of combined ultrasound-guided brachial plexus block and suprascapular nerve block reduced postoperative pain more effectively than single injection block within 36 hours after arthroscopic cuff repair, in addition to decreasing the rebound pain phenomenon.
Setting patient expectations with proper education about potential rebound pain will also help patients cope with the pain. A multimodal oral pain medication regimen can include paracetamol, a non-steroidal anti-inflammatory medication, an opioid analgesic, and a gabapentinoid.
The overall incidence of rebound pain after PNB resolved may reach 61.7%. Both patients, surgical and anesthesia related factors affect incidence as well as the severity of rebound pain. Use of perioperative multimodal decreases incidence as well as the severity of rebound pain after resolution of peripheral nerve block.
The diversity of factors was reviewed association with rebound pain, incidence and prevention and management in this systematic review considered the strength of the study. This study does not assess the specific time for which maximal rebound pain occurs and the effect of continuous peripheral nerve block on rebound pain incidence and severity not assessed.
Clinicians should stratify the risk of rebound pain. Continue to use preventative strategies; especially for patients at higher risk of experiencing rebound pain and future study should assess specific time occurrence for rebound pain after PNB is resolved and the effect of continuous PNB on rebound pain.
Not applicable.
Admassie BM developed key questions and keywords, analyzed the results of the search, prepared and revised the manuscript.
Review registry UIN1574.
Not applicable.
This work did not receive any grant from funding agencies in the public, commercial or not for profit sectors.
Not commissioned, externally peer-reviewed.
There is no any conflict of interest.
I would like to acknowledge University of Gondar for giving the chance to do this review. We would like to express special gratitude to the university of Gondar for appropriate funding as required. We would like also to thank you for giving us the chance to conduct this study, for constructive comments regarding the statistical issues of the study, and the whole process of the study being completed.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Admassie BM (2023) Incidence, Risks, Prevention and Management of Rebound Pain after Resolution of Peripheral Nerve Block. Systematic Review. J Anesth Clin Res. 14:1124.
Received: 08-May-2023, Manuscript No. JACR-23-23966; Editor assigned: 10-May-2023, Pre QC No. JACR-23-23966 (PQ); Reviewed: 24-May-2023, QC No. JACR-23-23966; Revised: 03-Dec-2023, Manuscript No. JACR-23-23966 (R); Published: 10-Dec-2023 , DOI: 10.35248/2155-6148.23.14.1124
Copyright: © 2023 Admassie BM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.